Web Stories
Latest Blogs
Low AMH: What it Means for Fertility & Treatment Options
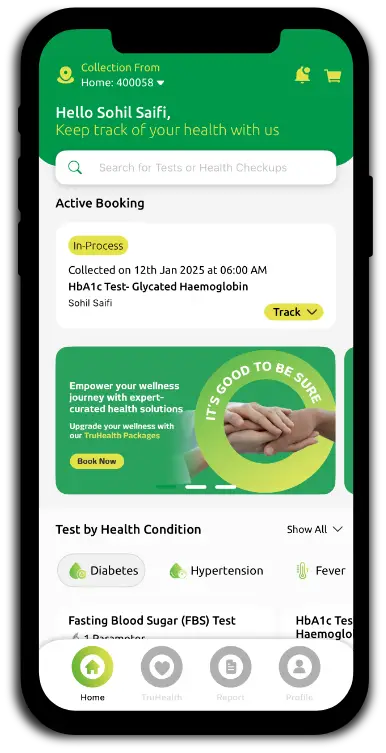
Low AMH: What it Means for Fertility Low AMH indicates that you have fewer developing follicles in your ovaries compared to what's typically expected for your age. This condition suggests reduced ovarian reserve, meaning fewer eggs are available each month for potential fertilisation. However, it's essential to understand that low AMH primarily measures egg quantity rather than quality. Low AMH can shorten your reproductive window and may affect how your ovaries respond to fertility medications during treatments like IVF. However, many women with low AMH levels successfully conceive both naturally and through assisted reproductive technologies. Understanding Low AMH and Fertility According to MedlinePlus, AMH levels naturally decline with age, reflecting the gradual decrease in your egg supply from birth to menopause. This hormone serves as a reliable indicator of how your ovaries might respond to fertility treatments, particularly during IVF procedures. Fertility specialists use AMH testing alongside other assessments, including antral follicle count through ultrasound and follicle-stimulating hormone (FSH) levels, to create a comprehensive overview of your reproductive health. It's important to note that AMH doesn't directly measure your ability to conceive naturally or predict pregnancy outcomes. A woman with low AMH but regular periods may still ovulate normally and conceive without assistance. Causes of Low AMH Natural ageing and ovarian ageing: AMH decreases steadily with age as your egg pool diminishes, eventually reaching undetectable levels at menopause. Genetic conditions: Some women inherit fewer eggs than average for their age due to genetic factors or primary ovarian insufficiency. Previous ovarian surgery: Procedures like cyst removal or endometrioma surgery can damage ovarian tissue and lower AMH. Cancer treatment: Chemotherapy and pelvic radiation can destroy ovarian follicles, significantly reducing AMH and fertility potential. Autoimmune diseases: Certain autoimmune conditions that target ovarian tissue may deplete follicles and lower AMH levels. Endometriosis: When it involves the ovaries, this condition can reduce ovarian reserve, particularly after repeated surgeries. Environmental factors: Smoking and exposure to certain toxins are associated with faster ovarian ageing. Turner syndrome: This genetic condition affects ovarian development and function. PCOS/PCOD: Although typically linked to high AMH, some women with these conditions may experience lower levels over time. Signs and Symptoms of Low AMH Difficulty conceiving after trying for several months. Shortened menstrual cycles (lasting 21–24 days instead of the typical 28). Irregular or skipped periods in some cases. Hot flashes or night sweats if associated with early ovarian insufficiency. Poor response to fertility medications during previous treatment cycles. Vaginal dryness or other menopausal-like symptoms. It's worth noting that many women with low AMH but regular periods experience no symptoms at all, making routine testing important for those planning pregnancy. How Low AMH Affects Fertility Low AMH levels primarily impact fertility by reducing the number of eggs available each menstrual cycle. With fewer developing follicles, your monthly chances of conception may decrease compared to women with normal AMH levels for their age. In fertility treatments, particularly IVF, low AMH often correlates with fewer eggs retrieved during the collection process. This can mean fewer embryos available for transfer and potentially lower success rates per cycle. However, it's crucial to remember that pregnancy success depends on egg quality, not just quantity. The relationship between low AMH and natural conception is complex. Some women with low AMH but regular periods continue to ovulate quality eggs and conceive without assistance. Your reproductive endocrinologist can help interpret your AMH levels alongside other fertility factors to provide personalised guidance. How is AMH Tested? The Anti-Müllerian Hormone (AMH) test involves a simple blood draw that can be performed on any day of your menstrual cycle, as AMH levels remain relatively stable throughout the month. A healthcare professional will take a blood sample from a vein in your arm using a small needle; after the needle is inserted, a small amount of blood is collected into a test tube or vial, and you may feel a brief sting. The process usually takes less than five minutes, and a small bandage is placed over the area afterward. The blood sample is then analysed in a laboratory to measure AMH concentration, typically reported in nanograms per millilitre (ng/mL). Treatment Options for Low AMH Timed intercourse: If you're young with normal menstrual cycles, your doctor may recommend optimising natural conception timing. Ovulation induction: Medications can stimulate egg development and improve the chances of conception each cycle. Intrauterine insemination (IUI): Combined with ovulation drugs, this can increase pregnancy likelihood. In vitro fertilisation (IVF): Customised stimulation protocols can maximise egg retrieval from reduced reserves. Egg freezing: Preserving current eggs for future use before further decline occurs. Donor eggs: When ovarian reserve is severely diminished, using younger donor eggs can significantly improve success rates. Fertility preservation: Storing eggs or embryos before cancer treatment or other interventions. Lifestyle optimisation: Supporting overall reproductive health through diet, exercise, and stress management. The choice of low AMH treatment depends on your age, your partner's fertility status, how low your AMH levels are, and your personal preferences regarding treatment intensity and timeline. How Lifestyle Changes Can Improve AMH Levels Stop smoking immediately: Tobacco accelerates ovarian ageing and further reduces AMH levels. Maintain a healthy weight: Balanced nutrition and regular exercise support hormonal balance. Manage chronic conditions: Proper treatment of endometriosis, thyroid disorders, and autoimmune diseases. Limit exposure to toxins: Avoid pesticides, heavy metals, and industrial chemicals when possible. Prioritise sleep quality: Adequate rest supports hormone production and overall health. Manage stress effectively: Chronic stress can impact reproductive hormones. IVF and Egg Freezing for Low AMH Customised stimulation protocols help maximise egg retrieval in cases of reduced ovarian reserve. Higher medication doses may be necessary to achieve an adequate ovarian response. Multiple retrieval cycles may be recommended to collect an adequate number of eggs for treatment. Realistic expectations about egg numbers and potential cycle cancellations. Focus on egg quality rather than quantity, particularly in younger women. Preimplantation genetic testing (PGT) may be considered to identify chromosomally healthy embryos. Should I Consider Donor Eggs for Low AMH? Donor eggs may be recommended when AMH levels are extremely low, previous IVF cycles have yielded poor results, or age-related factors compound ovarian reserve concerns. Using eggs from younger donors typically offers significantly higher pregnancy and live birth rates compared to using your own eggs with severely diminished reserves. This decision involves careful consideration of emotional, financial, and ethical factors. Counselling with fertility specialists and mental health professionals can help you navigate these complex choices and determine the best path forward for your family-building goals. Can Low AMH Levels Be Reversed? Currently, no proven medical treatments can restore ovarian reserve or significantly increase AMH levels once follicles are lost. Rather than focusing on reversing low AMH, current medical approaches emphasise accurate assessment, timely intervention, and optimised treatment strategies. Working with experienced fertility specialists ensures you receive evidence-based care tailored to your specific situation and reproductive goals. Low AMH and Pregnancy: What You Should Know Having low AMH doesn't mean pregnancy is impossible, but it may require more strategic planning and potentially medical assistance. Many women with low AMH conceive naturally, especially if they're younger and have no other fertility issues. The key is avoiding delays in trying to conceive and seeking medical advice if pregnancy doesn’t occur within six months. Research indicates that pregnancy outcomes in women with low AMH who do conceive are generally similar to those with normal AMH levels. The main challenge is achieving pregnancy rather than maintaining it once established. Age and Low AMH: A Critical Factor Age significantly influences how strongly low AMH levels impact your fertility prospects. A 25-year-old with low AMH may have better chances of conception than a 35-year-old with normal AMH levels because egg quality remains more important than quantity for successful pregnancy outcomes. Women under 35 with low AMH often have more time to try various treatments, while those over 35 may need to consider more aggressive interventions sooner. This is why age-specific counselling about fertility options is crucial for making informed decisions about your reproductive timeline. How Low AMH Affects IVF Success Rates Low AMH treatment through IVF typically involves individualized stimulation protocols to maximize egg retrieval from a diminished ovarian reserve. Success rates depend heavily on age, with younger women maintaining better pregnancy chances despite low AMH. Studies show that while egg numbers may be reduced, embryo quality and implantation rates can remain reasonable, particularly under age 35. Low AMH Treatment Options: Success Rates Natural conception: 20-30% chance if under 35 and ovulating regularly; drops sharply after 40. IUI with ovulation induction: 10-20% per cycle, depending on age and other factors. IVF with own eggs: 15–30% per cycle, varying significantly with age and AMH severity. Donor egg IVF: 60-70% per cycle, largely independent of the recipient's AMH levels. Multiple IVF cycles: Cumulative 50-70% after 3 cycles with own eggs. What Happens After IVF for Low AMH? Following IVF treatment for low AMH, your care team monitors pregnancy progress closely. Successful pregnancies from IVF with low AMH generally progress normally, though some women may require additional hormonal support during early pregnancy. If initial IVF cycles are unsuccessful, your fertility specialist will review the response and adjust protocols for future attempts. This might involve changing medications, or timing or considering alternative approaches like donor eggs. Can You Still Get Pregnant with Low AMH? Yes, pregnancy with low AMH is absolutely possible. While it may require more time, strategic planning, or medical intervention, many women with low AMH levels successfully conceive and deliver healthy babies. The key is receiving proper evaluation, understanding your individual prognosis, and pursuing appropriate treatment without unnecessary delay. Early intervention often improves outcomes, particularly when age is a factor alongside low AMH. Conclusion Understanding low AMH and its implications for fertility empowers you to make informed decisions about your reproductive journey. While low AMH levels present challenges, they're not an insurmountable obstacle to parenthood. The key lies in early assessment, appropriate treatment selection, and maintaining realistic but hopeful expectations throughout the process. Whether through natural conception, fertility treatments, or alternative family-building options, many paths to parenthood remain available. Working with experienced healthcare providers who understand the complexities of low AMH ensures you receive personalised care tailored to your unique circumstances. At Metropolis Healthcare, we understand the importance of accurate, timely diagnostic testing in your fertility journey. Our comprehensive portfolio of over 4,000 tests includes specialised hormone assessments and fertility panels designed to provide the precise information you and your healthcare provider need. With convenient home sample collection available across our extensive network of 10,000+ touchpoints throughout India, accessing reliable AMH testing and other fertility-related diagnostics has never been easier. FAQs What is considered a low AMH level? AMH levels below 1.0 ng/mL are generally considered low, though interpretation varies with age and individual circumstances, and specialist evaluation is required. Can low AMH be treated with natural remedies? While lifestyle improvements support overall reproductive health, no natural remedies have proven effective for significantly increasing AMH levels. How can I improve my AMH levels? Focus on maintaining optimal overall health through proper nutrition and exercise Avoid smoking and limit alcohol consumption Manage stress effectively through relaxation techniques Consider appropriate supplements after consulting your healthcare provider At what age does AMH start to decrease? AMH begins declining from birth but becomes more noticeable after age 30, with accelerated decrease typically occurring after age 35. What is the role of AMH in IVF? AMH helps predict ovarian response to stimulation medications and guides treatment protocol selection for optimal egg retrieval outcomes. References 1. https://www.who.int/news-room/fact-sheets/detail/infertility 2. https://medlineplus.gov/lab-tests/anti-mullerian-hormone-test/ 3. https://my.clevelandclinic.org/health/diagnostics/22681-anti-mullerian-hormone-test 4. https://academic.oup.com/jcem/article/105/11/3361/5890022?login=false 5. https://pmc.ncbi.nlm.nih.gov/articles/PMC4870438/
Hair Fall in Women: Causes, Hormonal Links & Treatments
Hair Fall in Women Hair fall in women is a common concern that can range from mild thinning to significant hair loss. According to the American Academy of Dermatology Association, it’s normal to shed about 50–100 hairs each day as part of the natural hair growth cycle. However, when this process becomes excessive or follicles are damaged, noticeable thinning occurs. Many women experience seasonal variations, with seasonal hair fall during monsoon and winter being particularly common due to humidity changes and reduced sunlight exposure affecting hair health. The key lies in identifying whether the causes of hair loss are hormonal, genetic, medical, or lifestyle-related. Early intervention significantly improves treatment outcomes and prevents progression. What Causes Hair Fall in Women? Female pattern hair loss, a genetic condition influenced by hormones, represents the most common type, affecting the crown and top of the scalp while typically preserving the frontal hairline. Telogen effluvium causes another frequent pattern, where significant physical or emotional stress pushes large numbers of hairs into the resting phase simultaneously. Major life events such as childbirth, serious illness, surgery, rapid weight loss, or intense psychological stress can trigger this type of diffuse shedding. Medical conditions such as thyroid disorders, polycystic ovary syndrome (PCOS), iron-deficiency anemia, and autoimmune diseases can disrupt normal hair growth. Additionally, certain medications, nutritional deficiencies, and harsh hair care practices may damage follicles or interfere with healthy growth cycles. Hormonal Links to Hair Fall Androgens, particularly dihydrotestosterone (DHT), can miniaturise hair follicles in genetically predisposed women, leading to progressive thinning characteristic of female pattern hair loss. Oestrogen levels play a major role in maintaining hair health. During menopause, declining estrogen levels reduce protection for hair follicles, often resulting in increased shedding and thinning. Pregnancy and the postpartum period also cause hormonal fluctuations that can trigger temporary hair loss (postpartum telogen effluvium). Both hypothyroidism and hyperthyroidism can cause diffuse hair loss, making thyroid function testing crucial when evaluating the causes of hair fall in women. Other hormones, including prolactin, growth hormone, and cortisol, also influence hair health and can contribute to various forms of alopecia. Common Symptoms of Hair Fall in Women Gradual thinning on the crown and along your parting line, particularly noticeable in bright lighting or photographs. Widened part that reveals more scalp than previously visible. Excessive shedding on pillows, in shower drains, or on hairbrushes, significantly more than the normal 50-100 hairs daily. Sudden diffuse hair loss occurring weeks to months after major illness, surgery, childbirth, or severe stress. Patchy bald spots that may indicate autoimmune conditions like alopecia areata. Receding frontal hairline or temple thinning, which can suggest hormonal influences. Scalp sensitivity, including itching, burning, or tenderness, potentially indicating inflammatory conditions. Thinning of eyebrows or body hair alongside scalp hair loss, suggesting systemic causes. The Role of Stress in Hair Fall Physical stressors such as high fever, major surgery, or rapid weight loss can trigger telogen effluvium, where stress hormones push large numbers of follicles into the resting phase simultaneously. Chronic psychological stress elevates cortisol levels, disrupting normal hair growth cycles and potentially accelerating genetic hair loss patterns. The causes of hair loss often include prolonged work pressure, relationship difficulties, or financial concerns that maintain elevated stress hormones over extended periods. Diagnostic Tests for Identifying Hair Fall in Women Detailed medical history, including recent illnesses, medications, menstrual patterns, and family history of hair loss. Physical examination of the scalp, hair pattern, and overall health assessment. Pull test where gentle traction on hair clusters helps identify active shedding phases. Dermoscopy or trichoscopy providing magnified examination of follicles and hair shafts Scalp biopsy in select or complex cases helps distinguish between different types of alopecia. Blood tests tailored to clinical findings: Thyroid Profile Test CBC (Complete Blood Count) test and Ferritin Serum test for iron deficiency Vitamin D test and vitamin B12 test if nutritional deficiency is suspected Androgen profile or PCOS screening panels (Profile-1, -2, or -3) may be recommended for women showing PCOS symptoms DHEA (Dehydroepiandrostenedione), serum test and Testosterone Profile to assess hormone levels Are Genetics a Factor in Hair Fall? Genetics play a substantial role in female pattern hair loss, the most common cause of hair thinning in women. This condition involves inherited sensitivity of hair follicles to androgens and age-related hormonal changes, leading to progressive miniaturisation of follicles over time. A family history on either the maternal or paternal side increases your risk, though the genetic patterns are complex and polygenic. You might develop female pattern hair loss even without an obvious family history, as multiple genes contribute to susceptibility, and environmental factors also influence expression. Treatments for Hair Fall in Women Effective treatment depends on accurate diagnosis, severity assessment, and individual patient factors. Evidence-based approaches include both topical and oral medications that promote hair growth or reduce hormonal effects on follicles. Addressing underlying medical conditions is a crucial component of effective treatment. Correcting thyroid dysfunction, treating iron deficiency, managing PCOS, or adjusting medications that contribute to hair loss often produces significant improvement in hair growth patterns. Dermatologists may recommend in-office procedures, such as corticosteroid injections for inflammatory conditions, low-level laser therapy, or platelet-rich plasma (PRP) treatments. In carefully selected cases, hair transplantation can provide excellent results for women with stable pattern hair loss and adequate donor hair availability. Medical Treatments for Hair Fall Topical minoxidil (2% or 5%), FDA-approved first-line treatment that prolongs growth phase. Oral minoxidil, a low-dose option when topical therapy proves ineffective. Anti-androgen medications, such as spironolactone or certain oral contraceptives for hormonal causes. Corticosteroids in various forms for inflammatory or autoimmune causes. Targeted therapies, including JAK inhibitors for severe alopecia areata in specialist settings. Treatment of underlying conditions such as thyroid hormone replacement, iron supplementation, PCOS management. Low-level laser devices, which are FDA-cleared adjunct therapies, can help improve hair density. Hair transplantation may be considered for selected women with stable pattern hair loss and sufficient donor hair. Natural Remedies for Hair Fall in Women Gentle hair care practices: Avoiding tight hairstyles, harsh chemicals, frequent high-heat styling, and aggressive brushing that can cause breakage. Proper scalp hygiene: Keeping the scalp clean, treating dandruff promptly, and avoiding irritating products. Evidence-based supplements: Iron, vitamin D, or other nutrients should only be taken when medically confirmed deficiencies exist. Scalp massage: May improve circulation, though evidence for hair growth benefits remains limited. Stress management techniques: Regular exercise, meditation, adequate sleep, and stress reduction strategies. Protective styling: Using silk pillowcases, gentle hair accessories, and avoiding tight ponytails or braids. Diet and Nutrition for Healthy Hair Proper nutrition supports optimal hair growth, though supplements should only be used when deficiencies are confirmed through testing. Hair follicles require adequate protein, iron, zinc, and vitamins for healthy function. Include lean proteins, leafy greens, nuts, seeds, and fish in your diet to provide essential nutrients. Iron-rich foods like spinach, lentils, and lean meats support healthy blood oxygen transport to follicles. Crash dieting or severe calorie restriction can trigger telogen effluvium, as the body prioritizes essential functions over hair growth during nutritional stress. When to Seek Medical Help for Hair Loss Consult a doctor if you notice sudden, significant hair loss, patchy bald spots, or hair loss accompanied by scalp irritation, pain, or other symptoms. Early intervention usually leads to better outcomes, especially for conditions such as alopecia areata or scarring alopecias. Seek immediate medical attention if hair loss occurs alongside symptoms suggesting underlying medical conditions, such as fatigue, weight changes, irregular periods, or skin changes. These may indicate thyroid disorders, hormonal imbalances, or other systemic conditions requiring prompt treatment. Conclusion Hair fall in women stems from various causes, including hormones, genetics, stress, and medical conditions. The causes of hair loss range from temporary conditions like telogen effluvium to chronic issues requiring ongoing management. Whether you're experiencing hair fall in monsoon due to humidity and fungal infections or hair fall in winter from dry conditions and reduced circulation, identifying triggers helps guide appropriate interventions. Effective treatment combines medical therapies with lifestyle modifications, nutritional support, and stress management. Early diagnosis and intervention significantly improve outcomes, making professional consultation essential for persistent hair loss. At Metropolis Healthcare, we understand that diagnosing hair fall in women requires comprehensive testing to identify underlying causes. Our extensive portfolio of over 4,000 tests includes hormonal panels, nutritional assessments, and specialized profiles to accurately identify the causes of hair fall in women. With our convenient home sample collection service spanning 10,000+ touchpoints across India, you can access accurate diagnostics from the comfort of your home. FAQs What is the most common cause of hair loss in women? The most common cause of hair loss in women is androgenetic alopecia (female-pattern hair loss). It results from genetics and hormonal sensitivity, leading to gradual thinning on the crown and part line. How can I prevent hair loss in women? Maintain gentle hair care practices and avoid harsh styling Manage stress through regular exercise and relaxation techniques Ensure adequate nutrition with proper protein and iron intake Address underlying health conditions promptly Avoid crash dieting and extreme weight loss Is hair loss a sign of something serious in women? Most hair loss in women results from benign causes like genetics or temporary stress. However, sudden or severe hair loss may indicate underlying medical conditions requiring evaluation. Can hormonal changes cause hair loss in women? Yes, hormonal fluctuations during menopause, pregnancy, thyroid disorders, and PCOS commonly trigger hair loss through effects on hair growth cycles and follicle sensitivity. When should I see a doctor for hair loss? Consult a doctor for sudden hair loss, patchy bald spots, scalp irritation, or hair loss accompanied by other concerning symptoms like fatigue or weight changes. Can stress cause hair loss in women? Yes, both physical and emotional stress can trigger telogen effluvium, leading to noticeable diffuse hair shedding two to four months after a stressful event. References 1. https://www.aad.org/public/diseases/hair-loss/insider/shedding 2. https://www.healthdirect.gov.au/female-pattern-hair-loss 3. https://my.clevelandclinic.org/health/diseases/16921-hair-loss-in-women 4. https://pmc.ncbi.nlm.nih.gov/articles/PMC6322157/ 5. https://pmc.ncbi.nlm.nih.gov/articles/PMC10379895/
Prenatal Vitamins: What to Take & Why They Matter
What Are Prenatal Vitamins? Prenatal vitamins are specialized multivitamin supplements designed specifically for women who are pregnant or planning to conceive. Unlike regular multivitamins, these supplements contain higher concentrations of nutrients crucial for pregnancy, including folic acid, iron, calcium, and vitamin D. A woman's prenatal vitamin differs significantly from standard supplements because it addresses the unique nutritional requirements during pregnancy. Your body needs increased amounts of certain nutrients to support fetal growth, placental development, and the maintenance of your own health throughout pregnancy. Why Are Prenatal Vitamins Important? Taking prenatal vitamins during pregnancy serves multiple critical functions for both mother and baby. The primary benefit is preventing serious birth defects, particularly neural tube defects such as spina bifida and anencephaly, which affect the brain and spinal cord. These defects occur in the early weeks of pregnancy, often before women realise they're pregnant. Taking prenatal vitamins also helps prevent common pregnancy complications, such as anemia, preeclampsia, gestational diabetes, and low birth weight. Research shows that adequate nutrition during pregnancy reduces the risk of impaired foetal development and supports optimal brain, bone, and organ formation. Key Nutrients in Prenatal Vitamins Folic Acid (Vitamin B9): Prevents neural tube defects and supports DNA synthesis and cell division. This B vitamin is crucial during the first trimester when the neural tube develops. Iron: Prevents anemia and supports increased red blood cell production to meet the body’s growing oxygen needs. Iron deficiency during pregnancy can lead to fatigue, weakness, and premature birth. Calcium: Essential for fetal bone and tooth development while maintaining maternal bone strength. Vitamin D: Aids calcium absorption and supports immune function for both mother and baby. DHA: An omega-3 fatty acid crucial for foetal brain and eye development. Vitamin C: Enhances iron absorption and supports collagen formation for healthy skin and tissues. Zinc: Supports cell division, immune function, and protein synthesis during pregnancy. Choline: Supports brain development and helps prevent neural tube defects. Iodine: Essential for foetal thyroid development and brain function. What to Look for When Choosing Prenatal Vitamins Adequate folic acid content: Ensure your supplement provides at least 400 micrograms (mcg) of folic acid daily, ideally starting before conception and continuing through the first 12 weeks of pregnancy to prevent neural tube defects effectively, as suggested by the NHS. Appropriate iron levels: Choose a supplement containing 18–27 mg of iron to prevent anaemia and support increased blood volume during pregnancy. Third-party testing: Choose prenatal vitamins from reputable manufacturers that have undergone independent quality testing. Easy absorption: Look for chelated minerals and active vitamin forms (like methylfolate instead of folic acid) for better bioavailability. Tolerability: Some formulations may cause less nausea or constipation than others. Healthcare provider approval: Always consult your doctor before starting any prenatal vitamin regimen. Complete nutrient profile: Ensure the supplement includes calcium, vitamin D, DHA, and other essential nutrients mentioned above. Reputable manufacturer: Select established brands with good safety records. Can Prenatal Vitamins Replace a Healthy Diet? Prenatal vitamins are supplements, not substitutes for a balanced and nutritious diet. While these vitamins help fill nutritional gaps, they cannot replace the complex array of nutrients, fibre, and beneficial compounds found in whole foods. Combining nutrient-dense foods with prenatal vitamins during pregnancy creates the optimal nutritional environment for your baby's development. Your doctor can help you create a meal plan that, combined with the best prenatal vitamins, ensures you meet all your nutritional needs throughout pregnancy. Focus on consuming plenty of fruits, vegetables, whole grains, lean proteins, and dairy products alongside your prenatal supplementation. Common Mistakes When Taking Prenatal Vitamins Starting too late: Beginning supplementation only after discovering pregnancy means missing the critical early weeks when neural tube defects can occur. Inconsistent intake: Skipping doses can reduce their protective benefits against birth defects and pregnancy complications. Choosing regular multivitamins: Standard vitamins lack the specific nutrient ratios needed to prevent neural tube defects and support pregnancy. Not consulting healthcare providers: Your doctor can recommend the best prenatal vitamins based on your individual needs and health history. Ignoring side effects: Rather than stopping supplementation due to nausea or constipation, work with your doctor to find solutions. Taking with certain foods: Some nutrients compete for absorption (for example, calcium can reduce iron absorption), so timing matters for best results. Prenatal Vitamins During Each Trimester First Trimester (Weeks 1-12): During the first trimester, prenatal vitamins focus on preventing neural tube defects and supporting early organ development. Folic acid becomes crucial for DNA synthesis and cell division. Iron helps prevent anaemia as blood volume begins expanding. Vitamin B6 may help reduce morning sickness severity. DHA supports early brain and nervous system development during this critical period. Second Trimester (Weeks 13-27): The second trimester emphasises supporting rapid foetal growth and maternal health. Calcium and vitamin D become increasingly important for the development of bones and teeth. Iron requirements continue to rise to support increased blood volume expansion. DHA remains essential for ongoing brain and eye development. Magnesium may help lower the risk of preeclampsia and support muscle and nerve function. Third Trimester (Weeks 28-40): In the final trimester, prenatal vitamins prepare your body for delivery whilst supporting continued foetal development. Iron requirements peak to prevent anemia and support red blood cell and fetal blood production. DHA continues supporting brain maturation. Vitamin C enhances immune function and supports tissue repair. Adequate nutrition during this phase helps ensure optimal birth weight and reduces complications. Are There Risks to Taking Prenatal Vitamins? Prenatal vitamins are generally safe when taken as directed, and their benefits far outweigh potential risks. Most women tolerate these supplements well, experiencing significant protection against serious pregnancy complications and birth defects. Some women may experience mild side effects, usually due to the iron content. These can include nausea, constipation, or stomach upset. However, these issues can usually be managed by taking vitamins with food, adjusting timing, or switching formulations under medical guidance. The key is maintaining consistent supplementation throughout pregnancy, as stopping prenatal vitamins increases the risk of neural tube defects, anaemia, and other complications. Your doctor can help address any concerns while ensuring you receive optimal nutrition. How to Take Prenatal Vitamins Correctly Start early: Begin taking prenatal vitamins when trying to conceive, or immediately after confirming pregnancy to prevent neural tube defects effectively. Take daily: Establish a consistent routine, taking your vitamin at the same time each day to maintain steady nutrient levels. Take with food: This reduces nausea and improves absorption of fat-soluble vitamins whilst minimising stomach upset. Stay hydrated: Drink plenty of water, especially if experiencing constipation from iron supplementation. Should I Take Prenatal Vitamins If I'm Not Pregnant? Prenatal vitamins are not generally recommended for non-pregnant women, as they contain higher doses of nutrients like folic acid, iron, and calcium tailored specifically for pregnancy needs. These elevated nutrient levels may exceed standard requirements for non-pregnant adults and could cause constipation, digestive discomfort, or excess vitamin intake, especially if your regular diet is already well-balanced and nutritionally adequate. Conclusion Prenatal vitamins play a crucial role in supporting healthy pregnancies by preventing serious complications like neural tube defects, anaemia, preeclampsia, and low birth weight. Understanding what prenatal vitamins are and choosing the best prenatal vitamins for your needs helps ensure optimal nutrition for both you and your developing baby. Remember that these supplements work best alongside a balanced diet and regular prenatal care, not as a replacement for healthy eating habits. Taking the right women's prenatal vitamin consistently throughout pregnancy significantly reduces risks of impaired foetal development and supports your health during this transformative time. Whether you're planning pregnancy or already expecting, consulting with your doctor about prenatal vitamins during pregnancy ensures you're making the best choices for your unique situation. At Metropolis Healthcare, we support your pregnancy journey with comprehensive diagnostic services designed to monitor your health and your baby's development. With over 4,000 advanced tests and profiles available through our network of 220+ laboratories, we provide accurate, reliable results that guide effective pregnancy care. Our convenient home sample collection service, spanning 10,000+ touchpoints across India, ensures convenient access to essential pregnancy-related health monitoring from the comfort of your home. FAQs What are the best prenatal vitamins to take? The best prenatal vitamins contain adequate folic acid, iron, calcium, vitamin D, and DHA. Consult your doctor for personalised recommendations based on your individual nutritional needs and health status. Can prenatal vitamins cause side effects? Mild side effects, such as nausea or constipation, may occur, typically due to the iron content. Taking vitamins with food and staying hydrated usually helps manage these symptoms effectively. Is it OK to take prenatal vitamins after pregnancy? Yes, continuing prenatal vitamins while breastfeeding supports milk production and maternal nutrient stores. Your doctor can advise when to transition to regular multivitamins. References https://my.clevelandclinic.org/health/drugs/9754-pregnancy-prenatal-vitamins https://www.nhs.uk/pregnancy/keeping-well/vitamins-supplements-and-nutrition/ https://medlineplus.gov/druginfo/meds/a625022.html https://www.acog.org/womens-health/faqs/nutrition-during-pregnancy https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/expert-answers/prenatal-vitamins/faq-20057922
Second Trimester of Pregnancy: What to Expect
What is the Second Trimester of Pregnancy? The second trimester of pregnancy spans from week 13 to week 27, encompassing months four through six of your pregnancy. During these weeks, many women experience increased energy levels and a noticeable reduction in morning sickness symptoms that characterised the first trimester. Your uterus grows significantly during this time, expanding beyond your pelvis and creating the distinctive baby bump that makes your pregnancy more visible. This is also when you'll likely feel your baby's first movements, typically between weeks 18 and 20, creating a wonderful emotional connection between you and your growing baby. The second trimester of pregnancy, week by week, brings remarkable developments for your baby. According to the American Pregnancy Association, major organs continue maturing, senses develop, and the the fetus grows from approximately 6 inches (15 cm) to about 14 inches (35 cm) in length. Meanwhile, your body adapts to accommodate this growth, preparing for the final stretch of pregnancy and eventual delivery. Physical Changes During the Second Trimester Visible baby bump development as your uterus expands upward into your abdomen. Breast enlargement and increased sensitivity with darkening of nipples and areolae. Skin changes, including the appearance of linea nigra (dark line on abdomen) and possible melasma (facial pigmentation). Stretch marks on your abdomen, breasts, thighs, or buttocks are due to rapid skin stretching. Body aches and pains, particularly in your back, hips, and lower abdomen, result from ligament stretching. Round ligament pain causes sharp or aching sensations on one or both sides of your lower belly. Increased vaginal discharge that appears thin, white, and mildly scented. Nasal congestion and occasional nosebleeds from increased blood volume. Varicose veins and hemorrhoids can occur as blood volume increases and pressure builds on pelvic veins. Leg cramps often occur at night. More frequent urination as your expanding uterus continues pressing on your bladder. Common Symptoms in the Second Trimester Reduced nausea and vomiting, with many women experiencing significant relief from morning sickness. Increased energy levels compared to the first trimester, though some fatigue may persist. Heartburn and indigestion are caused by hormonal changes that affect your digestive system. Constipation and gas from slower intestinal movement and uterine pressure. Back pain and pelvic discomfort from postural changes and weight gain. Headaches or episodes of dizziness in the second trimester of pregnancy are associated with changes in blood volume. Mild shortness of breath during physical activity as your uterus grows upward. Braxton Hicks contractions – irregular, painless practice contractions. Emotional fluctuations, including anxiety or mood swings, despite generally feeling better. Mild swelling in your ankles or feet may occur, especially later in this trimester. Vomiting in the second trimester of pregnancy should be less frequent than in early pregnancy, but persistent or severe symptoms warrant medical attention. Similarly, dizziness can occur due to blood pressure changes; frequent episodes require evaluation. Health Considerations and Precautions Maintaining optimal health during the second trimester of pregnancy requires attention to several key areas. Regular prenatal care becomes increasingly important, with appointments typically scheduled every four weeks in uncomplicated pregnancies. Your doctor monitors blood pressure, weight gain, and foetal growth and screens for potential complications, including gestational diabetes and preeclampsia. Nutrition plays a crucial role during this period. Your diet during the second trimester should focus on balanced meals rich in essential nutrients. Increase your intake of iron-rich foods like lean meats, leafy greens, and legumes to help prevent anaemia. Calcium-rich dairy products, fortified cereals, and dark leafy vegetables support your baby's bone development. Omega-3 fatty acids from fish, chia seeds, walnuts, and flaxseeds support your baby’s brain development. Safe physical activity remains beneficial during the second trimester of pregnancy. Walking, swimming, and prenatal yoga can help manage back pain, improve mood, and maintain healthy weight gain. However, avoid activities with fall risks or contact sports, and always consult your doctor before starting new exercise routines. Tests to Do in the 2nd Trimester Routine prenatal assessments include blood pressure monitoring, weight checks, fundal height measurements, and fetal heart rate monitoring at each visit. A detailed anatomy ultrasound scan is performed between weeks 18-22 to assess fetal development, organ formation, placental position, and amniotic fluid levels. Maternal Screen (Quadruple Marker) – Second Trimester (14–22.6 weeks) and Maternal screen (Triple Marker) - 2nd Trimester, Serum to assess risks for chromosomal conditions like Down syndrome and neural tube defects. Gestational Diabetes Mellitus (GDM) Test to screen for early signs of elevated blood sugar and guide management. Additional diagnostic procedures, such as amniocentesis (weeks 15–20), may be recommended if screening tests indicate an increased risk for genetic conditions. Blood tests for anaemia (such as Anaemia Profile - Mini or Anaemia Profile - Maxi) and other conditions, with follow-up iron supplementation, if needed. Infection screening using tests, such as the urine culture test or STD Profile-I Test, is performed when clinically indicated based on your risk factors. When to Seek Medical Advice in the Second Trimester Vaginal bleeding or blood clots, especially if heavy or accompanied by cramping. Severe abdominal or pelvic pain that doesn't improve with rest. Fluid leakage from the vagina could indicate premature rupture of membranes (PROM). Regular contractions before 37 weeks or increased pelvic pressure. Fever above 38°C with chills or flu-like symptoms. Painful urination or blood in urine suggests a urinary tract infection. Severe headaches with vision changes or sudden facial swelling, potential signs of preeclampsia. Chest pain or severe shortness of breath at rest. A significant decrease in fetal movement after you’ve established a regular pattern. Persistent vomiting prevents fluid intake or causes dehydration. Tips for a Healthy Second Trimester Maintain regular prenatal appointments to monitor your health and your baby's development. Eat a balanced diet with emphasis on iron, calcium, folate, and protein-rich foods. Stay hydrated by drinking plenty of water throughout the day. Take prenatal vitamins as prescribed, particularly those containing folic acid and iron. Practice good posture and use supportive pillows whilst sleeping. Engage in safe exercises such as walking, swimming, or prenatal yoga. Get adequate rest and sleep, using pregnancy pillows for comfort. Manage stress through relaxation techniques, meditation, or prenatal classes. Avoid harmful substances, including alcohol, tobacco, and recreational drugs. Practice food safety by avoiding unpasteurized products, undercooked meat, and raw seafood. Wear comfortable, supportive clothing, including well-fitting maternity bras. Understanding the Growth of Your Baby in the 2nd Trimester The second trimester of pregnancy, week by week, reveals remarkable fetal development. Between weeks 13–16, your baby’s facial features become more defined, and the external genitalia develop enough for sex determination during an ultrasound. By weeks 17-20, you may feel those first magical movements as your baby becomes more active. The anatomy scan during this period provides detailed images of your baby's organs and development. From weeks 21-24, your baby's hearing develops, and they begin responding to sounds from outside the womb. Fat deposits start forming under the skin, and the lungs continue to develop rapidly. By weeks 25-27, your baby's brain undergoes rapid growth, eyelids begin opening, and the chances of survival improve significantly if premature birth occurs. Throughout this period, regular monitoring ensures your baby's healthy development whilst addressing any concerns promptly. What to Expect in the Third Trimester? As you approach the third trimester of pregnancy, beginning around week 28, new physical and emotional changes await. The third trimester of pregnancy brings increased frequency of prenatal visits, typically every two weeks until week 36, then weekly until delivery. You may experience different symptoms, including increased shortness of breath, more pronounced back pain, and frequent urination as your baby grows larger and puts more pressure on your organs. The third trimester of pregnancy focuses heavily on preparing for labour and delivery, with discussions about birth plans, pain management options, and recognising signs of labour. Your baby will gain significant weight during this period, and you'll likely feel stronger, more frequent movements. Understanding what lies ahead helps you transition smoothly from the comfortable second trimester of pregnancy into the final stretch of your pregnancy journey. Conclusion The second trimester of pregnancy represents a unique opportunity to enjoy your pregnancy whilst maintaining optimal health for you and your baby. By understanding what the second trimester of pregnancy is and recognising normal changes versus warning signs, you can navigate this period with confidence. Remember that every pregnancy is different, and maintaining open communication with your doctor ensures personalized care tailored to your unique needs. Regular monitoring through appropriate tests, maintaining a healthy lifestyle, and staying informed about your body's changes contribute to a positive pregnancy experience. Whether you're dealing with dizziness in the second trimester of pregnancy, planning appropriate meals for the second trimester, or tracking your second trimester week by week, having reliable information empowers you to make informed decisions. Metropolis Healthcare, supports your pregnancy journey with comprehensive diagnostic services across a network of over 220 laboratories and 4,600 service centres. Our home sample collection service brings convenience to your doorstep, ensuring you can access essential pregnancy tests and health check-ups without stress. FAQs What tests are done in the second trimester of pregnancy? Second-trimester tests include routine prenatal assessments, a detailed anatomy ultrasound (18–22 weeks), Maternal Screen (Triple Test) Second Trimester Test, Gestational Diabetes Mellitus (GDM) Test, blood tests for anaemia, such as Anaemia Profile – Mini/Maxi, and infection screening, such as Urine Culture Test or STD Profile – 1. How many weeks is the second trimester? The second trimester spans from week 13 to week 27 of pregnancy, encompassing approximately 15 weeks or the fourth through sixth months of pregnancy. What are the signs of a healthy second-trimester pregnancy? Signs include increased energy, reduced nausea, appropriate weight gain, a feeling of foetal movements, normal blood pressure, and good results on routine prenatal tests. How to manage fatigue in the second trimester? Combat fatigue through adequate sleep, balanced nutrition, gentle exercise, stress management, proper hydration, and taking short rest breaks throughout the day when needed. How often should I see a doctor during the second trimester? Typically, every four weeks for low-risk pregnancies, though your doctor may recommend more frequent visits based on individual circumstances or risk factors. Can you have a baby bump in the second trimester? Yes, most women develop a noticeable baby bump during the second trimester as the uterus grows beyond the pelvis and becomes visible. References 1. https://my.clevelandclinic.org/health/articles/16092-pregnancy-second-trimester 2. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/pregnancy/art-20047732 3. https://americanpregnancy.org/healthy-pregnancy/pregnancy-health-wellness/second-trimester/ 4. https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-second-trimester 5. https://www.nhs.uk/best-start-in-life/pregnancy/week-by-week-guide-to-pregnancy/2nd-trimester/week-13/
First Trimester of Pregnancy: Symptoms & Health Tips
What is the First Trimester of Pregnancy? The first trimester of pregnancy encompasses the initial 13 weeks, calculated from the first day of your last menstrual period. During the first trimester, remarkable developments occur as the fertilized egg implants in the uterine wall, forming the placenta and initiating organ formation. This period is characterised by rapid hormonal changes that trigger various symptoms, while your baby’s major organs, brain, spinal cord, and heart begin developing. According to the NHS, by week 13, your baby measures approximately 7.4 centimetres (about 3 inches). The first trimester of pregnancy is considered the most critical phase for foetal development, making it essential to establish healthy habits early. Common Symptoms During the First Trimester Missed menstrual period: Often the first sign prompting a pregnancy test. Nausea and vomiting: The most common symptom among pregnant women, typically beginning around weeks 4-6. Breast tenderness and swelling: Caused by increased oestrogen and progesterone levels. Extreme fatigue: Linked to rising progesterone levels and increased metabolic demands. Frequent urination: Results from increased blood flow to the kidneys and growing uterus pressure. Light spotting or cramping: Implantation bleeding is normal, but heavy bleeding during the first trimester of pregnancy requires immediate medical attention. Food cravings and aversions: Heightened sensitivity to tastes and smells. Mood swings: Hormonal fluctuations affecting emotional regulation. Bloating and constipation: Progesterone slows digestive processes. Headaches and dizziness: Often related to changes in blood pressure and increased blood volume. Nausea and Morning Sickness: How to Manage? Eat small, frequent meals every 2–3 hours to prevent your stomach from becoming empty. Choose bland, easily digestible foods such as bananas and rice. Stay hydrated with small sips of water, ginger tea, or electrolyte solutions. Avoid trigger foods, including spicy, greasy, or strong-smelling items. Try ginger tea or supplements, which may naturally help reduce nausea. Get adequate rest, as fatigue can worsen nausea symptoms. Consider vitamin B6 supplements under medical supervision for severe cases. Contact your doctor if you experience severe vomiting that prevents keeping food or fluids down, as this may indicate hyperemesis gravidarum requiring medical intervention. Fatigue and How to Cope with It Prioritise rest by going to bed earlier and taking short daytime naps when possible. Listen to your body and reduce non-essential activities when feeling exhausted. Maintain stable blood sugar by eating balanced meals and healthy snacks regularly. Engage in light exercise such as walking, if approved by your healthcare provider. Stay well-hydrated, as dehydration can worsen fatigue significantly. Ask your doctor to check for iron-deficiency anemia or thyroid issues if fatigue becomes severe. Physical Changes: What to Expect Breast changes, including increased size, tenderness, and darker areolas, as mammary glands prepare for breastfeeding. Mild weight fluctuations, with some women experiencing slight weight loss due to nausea. Abdominal bloating creates a fuller feeling before the characteristic pregnancy bump appears. Skin changes, such as increased pigmentation, particularly around nipples and a dark line (linea nigra) down the abdomen. Increased vaginal discharge — thin, milky leukorrhea is normal and helps prevent infections. Visible veins on breasts and abdomen as blood volume increases. Mild cramping as the uterus expands, though severe pain warrants medical evaluation. Healthy Eating Tips for the First Trimester Focus on nutrient-dense foods, including fruits, vegetables, whole grains, lean proteins, and healthy fats. Take prenatal vitamins containing at least 400 micrograms of folic acid to prevent neural tube defects. Include iron-rich foods, such as lean meats, poultry, beans, and fortified cereals, to support increased blood volume. Consume calcium-rich foods, such as dairy products, leafy greens, and fortified plant-based alternatives. Stay hydrated by drinking water regularly throughout the day. Eat protein with each meal to maintain stable blood sugar levels and support foetal growth. Choose complex carbohydrates over simple sugars for sustained energy. Limit processed foods high in sodium, added sugars, and unhealthy fats. Choose small, frequent meals if experiencing nausea, heartburn, or bloating. First Trimester Health Tips Schedule your first prenatal appointment ideally between weeks 8 and 10 or as soon as you receive a positive pregnancy test. Start prenatal vitamins immediately with folic acid and other essential nutrients. Eliminate harmful substances, including alcohol, tobacco, and recreational drugs, completely. Review all medications with your healthcare provider to ensure pregnancy safety. Establish safe exercise routines, such as walking, swimming, or prenatal yoga, with medical approval. Practice stress management through meditation, deep breathing, or counselling when needed. Maintain good hygiene to prevent infections that could affect pregnancy. Avoid high-risk activities such as contact sports, hot tubs, saunas, and anything with a risk of falling. What Tests Are Done in the First Trimester? Comprehensive physical examination, including blood pressure, weight, and medical history review. CBC (Complete Blood Count) Test to check for anaemia. Blood Group (ABO & Rh Typing), EDTA Blood to identify potential incompatibility issues. Infectious disease screening (such as HIV, HBV, and HCV viral marker profiles) for HIV, hepatitis B and hepatitis C. Immunity testing for rubella (such as Rubella (German Measles) - IgG & IgM antibody, Serum), varicella (such as VZV (Varicella Zoster Virus) DNA Detection by RT-PCR, EDTA Blood) and other vaccine-preventable diseases. Urine Routine Test (Urine R/M Test) to detect infections, protein, or glucose abnormalities. Comprehensive thyroid profile tests to ensure proper hormone levels for fetal brain development. Genetic carrier screening (such as Maternal Screen (QUAD test) - 1st Trimester with Preeclampsia, Serum and Maternal screen (Dual Marker) - 1st Trimester, Serum) based on family history. How to Handle Emotional Changes in the First Trimester Acknowledge your feelings as valid responses to significant life changes. Communicate with your partner about your emotions and concerns openly. Join pregnancy support groups to connect with other expectant mothers. Practice stress-reduction techniques such as deep breathing, meditation, or gentle yoga. Maintain social connections with supportive friends and family members. Consider professional counselling if anxiety or depression becomes overwhelming. First Trimester: When to Contact Your Doctor Heavy bleeding at any time during the first trimester, with or without cramping. Severe abdominal or pelvic pain that doesn't improve with rest. Persistent vomiting that prevents you from keeping any food or fluids down. High fever above 38°C with or without other symptoms. Severe headaches accompanied by vision changes or swelling. Burning sensation during urination indicates a possible infection. Complete absence of pregnancy symptoms if previously present. Fainting or severe dizziness that interferes with daily activities. Conclusion The first trimester of pregnancy is a remarkable journey of transformation that requires careful attention to your health and well-being. Understanding what to eat, recognizing normal symptoms, and knowing when to seek medical care empower you to navigate this crucial period confidently. From managing morning sickness to attending essential lab tests during pregnancy, each step contributes to your baby's healthy development. Remember that some symptoms, such as heavy bleeding or severe pain during the first trimester, require immediate medical attention. As you progress through the critical first trimester of pregnancy and into the third trimester, maintaining open communication with your medical team ensures optimal care. At Metropolis Healthcare, we support your pregnancy journey with comprehensive diagnostic services designed around your needs. Our extensive portfolio of over 4,000 tests includes all essential lab tests during pregnancy, from routine blood work to specialised screenings. With our convenient home sample collection service spanning 10,000+ touchpoints across India, you can access reliable pregnancy testing and monitoring from the comfort of your home. FAQs What are the first signs of pregnancy? The earliest pregnancy signs include missed periods, breast tenderness, nausea, fatigue, and frequent urination, typically appearing around weeks 4-6 after your last menstrual period. How long does the first trimester last? The first trimester spans 13 weeks, from conception through the end of week 13, calculated from the first day of your last menstrual period. What should I avoid during the first trimester? Alcohol, tobacco, and recreational drugs. Raw or undercooked meats and eggs. Unpasteurised dairy products. Excessive caffeine intake. When do pregnancy symptoms start to ease? Most first-trimester symptoms, particularly nausea and fatigue, typically begin improving around weeks 12-14 as hormone levels stabilise, entering the second trimester. Can I exercise during the first trimester? Yes, gentle exercise like walking, swimming, or prenatal yoga is generally safe and beneficial, but always consult your healthcare provider first. References 1. https://www.nhs.uk/best-start-in-life/pregnancy/week-by-week-guide-to-pregnancy/2nd-trimester/week-13/ 2. https://my.clevelandclinic.org/health/articles/9699-first-trimester 3. https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/pregnancy/art-20047208 4. https://www.betterhealth.vic.gov.au/health/healthyliving/pregnancy-week-by-week#first-trimester-of-pregnancy-%E2%80%93-conception-to-12-weeks
What is Nonalcoholic Fatty Liver Disease? Symptoms, Causes, and Treatment
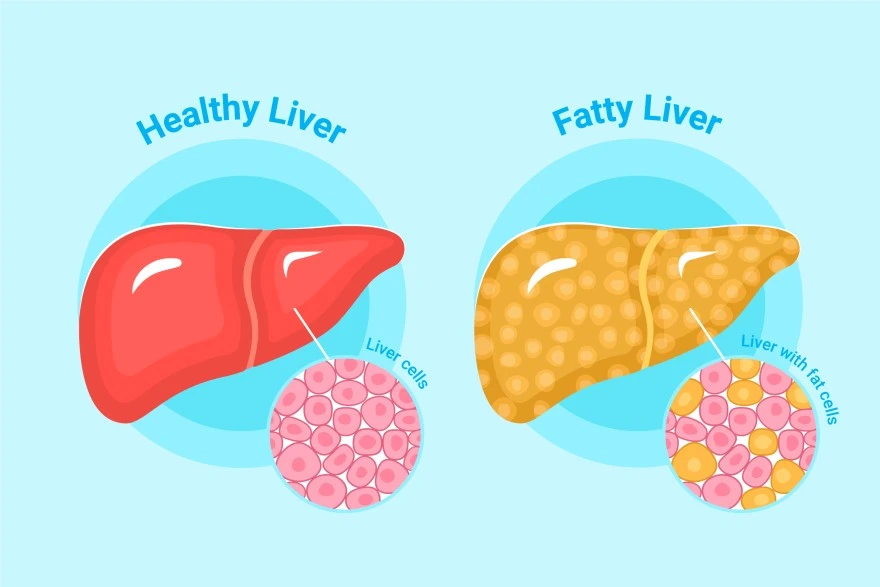
What is Nonalcoholic Fatty Liver Disease? Nonalcoholic fatty liver disease, now officially termed metabolic dysfunction-associated steatotic liver disease (MASLD), is a condition where excess fat builds up in liver cells in people who consume minimal alcohol. This liver disease is strongly linked to overweight or obesity, type 2 diabetes, abnormal blood lipids, and other features of metabolic syndrome. Many people develop simple steatosis, which involves fat accumulation without significant inflammation. However, a more serious form called metabolic dysfunction-associated steatohepatitis (MASH), previously known as nonalcoholic steatohepatitis (NASH), includes liver inflammation and cell injury. If left untreated, this progressive liver disease can advance to fibrosis, cirrhosis, liver failure, or even hepatocellular carcinoma (liver cancer). A concerning aspect of nonalcoholic fatty liver disease is that it often causes no symptoms, particularly in its early stages. Many people discover they have this condition incidentally during routine blood tests or imaging performed for other reasons. This silent progression makes regular health monitoring crucial for early detection and management. Symptoms of Nonalcoholic Fatty Liver Disease Recognizing the symptoms of nonalcoholic fatty liver disease can be challenging because the condition often remains silent in its early stages. When nonalcoholic fatty liver disease symptoms do appear, they typically include: Persistent fatigue or feeling unusually tired throughout the day General malaise or feeling unwell without a specific cause Dull pain or discomfort in the upper right abdomen, where the liver is located Unexplained weakness affecting daily activities Loss of appetite and unintentional weight loss, particularly in advanced stages Nausea or feeling sick to your stomach Itchy skin (pruritus) as the condition progresses Yellowing of skin and eyes (jaundice) in advanced disease Abdominal swelling from fluid buildup (ascites) Swelling in legs and ankles (oedema) Spider-like blood vessels (spider angiomas) under the skin in liver cirrhosis Mental confusion or difficulty concentrating in severe disease Gastrointestinal bleeding from enlarged veins in advanced liver cirrhosis Common Symptoms and Their Impact on Daily Life Since nonalcoholic fatty liver disease often remains silent, you might feel completely normal or notice only subtle fatigue or vague right-sided abdominal discomfort. These symptoms can easily be mistaken for stress, indigestion, or general fatigue. Persistent tiredness and weakness significantly reduce your energy levels, productivity, and exercise tolerance. This creates a challenging cycle where reduced physical activity makes it harder to maintain the healthy lifestyle crucial for managing fatty liver disease. As the condition progresses to MASH and potentially liver cirrhosis, symptoms like poor appetite, nausea, abdominal swelling, leg swelling, itching, and sleep problems can severely affect your eating patterns, mobility, sleep quality, and mood. Causes of Nonalcoholic Fatty Liver Disease Nonalcoholic Fatty liver disease develops when the liver stores more fat than it can process or eliminate, typically occurring alongside metabolic dysfunction. The major risk factors for developing fatty liver disease include obesity (particularly excess abdominal fat), insulin resistance, prediabetes or type 2 diabetes, high triglycerides, abnormal cholesterol levels, and high blood pressure. These conditions often occur together as metabolic syndrome, creating an environment where the liver accumulates fat. Additional contributing factors include rapid weight loss, certain medications (such as some cancer drugs, corticosteroids, and calcium channel blockers), bowel diseases that affect nutrient absorption, and previous bariatric surgery. Hormonal factors, genetics, and changes in gut bacteria also influence how individuals store fat and develop liver inflammation. Interestingly, fatty liver disease can occasionally occur in people without obvious risk factors, suggesting that genetic predisposition and environmental factors play important roles. This condition becomes more common after age 40 and affects men and women differently, with postmenopausal women showing increased risk. How Lifestyle and Diet Contribute to NAFLD Diets high in calories, added sugars (especially fructose from soft drinks), refined carbohydrates, and saturated fats promote weight gain and insulin resistance, leading to fat accumulation in the liver. Physical inactivity compounds these effects by reducing your body's ability to burn fat and regulate blood sugar effectively. When you consume more calories than you burn, the excess energy gets stored as fat, including in liver cells. Over time, this fat accumulation triggers inflammation and can progress to more serious liver diseases. Conversely, adopting healthier eating patterns and increasing physical activity can dramatically improve liver health. Research shows that even modest weight loss of 3-5% of body weight can significantly reduce liver fat. Regular exercise enhances insulin sensitivity and helps your body use fat more efficiently, reducing the burden on your liver. How to Diagnose Nonalcoholic Fatty Liver Disease Doctors usually suspect nonalcoholic fatty liver disease when blood tests show mildly elevated liver enzymes such as ALT and AST, or when imaging performed for other reasons reveals fatty liver changes. The diagnostic process begins with a detailed medical history, including your alcohol intake, current medications, and metabolic risk factors. During physical examination, doctors look for signs of liver diseases such as an enlarged liver, abdominal swelling, or skin changes that might indicate advanced disease. This comprehensive assessment helps distinguish nonalcoholic fatty liver disease from other liver conditions and determines the appropriate diagnostic approach. Additional blood tests help rule out other causes of liver disease, including viral hepatitis, autoimmune liver disease, and haemochromatosis. When advanced scarring is suspected or the diagnosis remains uncertain, doctors may recommend a liver biopsy to distinguish simple fatty liver from steatohepatitis and accurately stage any fibrosis. Imaging and Diagnostic Tests to Identify NAFLD Ultrasound examination: Often the first imaging test performed; shows increased liver echogenicity, suggesting fat infiltration. CT scan: Reveals reduced liver density compared to the spleen, indicating fat accumulation. MRI and specialised MRI techniques: Provide more accurate quantification of liver fat content. Transient elastography (FibroScan): Uses ultrasound technology to measure liver stiffness and estimate fibrosis severity. FibroMax (Fibrosis, Activity, Steatosis, ASH, and NASH) panel: Provide a comprehensive assessment of liver fibrosis, steatosis, inflammation, hepatitis and cirrhosis. Liver Function Test (LFT): Measure ALT, AST, alkaline phosphatase, and bilirubin levels. Comprehensive Metabolic Panel: Assesses liver and kidney function and electrolyte balance. Fatty Liver Profile: Aids in differentiating fatty liver from other liver diseases. Liver Biopsy: Gold standard for distinguishing simple steatosis from steatohepatitis when necessary. Treatment Options for Nonalcoholic Fatty Liver Disease Currently, no specific medication can cure nonalcoholic fatty liver disease, making lifestyle modification the cornerstone of treatment. The primary goal focuses on addressing underlying metabolic risk factors through sustained lifestyle changes that promote gradual, healthy weight loss. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), losing approximately 7-10% of your body weight can reduce liver fat, improve inflammation, and may even reverse early fibrosis. This weight loss should occur gradually through a combination of calorie-controlled eating and increased physical activity. Managing associated medical conditions is equally important. Controlling blood sugar in diabetes, lowering cholesterol and triglycerides, and treating high blood pressure reduces risks for both liver and cardiovascular complications. For selected patients, particularly those with obesity and difficult-to-control diabetes, bariatric surgery can significantly improve fatty liver disease and steatohepatitis. How to Manage and Treat NAFLD Effectively Achieve gradual weight loss through sustainable dietary changes and regular physical activity. Follow a Mediterranean-style diet emphasizing vegetables, fruits, whole grains, lean proteins, and healthy fats. Limit added sugars and refined carbohydrates, particularly sugary beverages and processed foods. Exercise regularly, aiming for at least 150 minutes of moderate-intensity activity per week. Manage diabetes effectively through medication compliance and blood sugar monitoring. Control cholesterol and triglyceride levels with appropriate medications when necessary. Maintain healthy blood pressure through lifestyle modifications and medications if needed. Avoid alcohol entirely to prevent additional liver stress. Monitor liver function regularly through scheduled blood tests and imaging. Conclusion Nonalcoholic fatty liver disease (MASLD) represents a growing global health concern affecting millions worldwide. Understanding the definition of nonalcoholic fatty liver disease, recognising its symptoms, and knowing its causes empower you to take proactive steps towards better liver health. While the condition often remains silent in its early stages, implementing lifestyle changes focused on gradual weight loss, healthy eating, and regular exercise can significantly improve outcomes and prevent progression to liver cirrhosis or liver failure. The key to managing fatty liver disease lies in addressing underlying metabolic risk factors through sustainable lifestyle modifications. Regular monitoring through appropriate diagnostic tests helps track your progress and adjust treatment strategies as needed. At Metropolis Healthcare, we understand the importance of early detection and monitoring in managing liver diseases effectively. Our comprehensive portfolio of over 4,000 tests includes specialised liver function panels and metabolic assessments that deliver accurate and timely results. With our extensive network of a network of over 220 laboratories and 10,000+ convenient home sample collection points across India, accessing quality diagnostic care has never been easier. FAQs What causes nonalcoholic fatty liver disease? Nonalcoholic fatty liver disease primarily results from metabolic dysfunction, including obesity, insulin resistance, diabetes, high triglycerides, and metabolic syndrome, leading to excess fat accumulation in liver cells. How can nonalcoholic fatty liver disease be prevented? Prevention involves maintaining a healthy weight, eating a balanced diet low in added sugars, exercising regularly, managing diabetes and cholesterol levels, and avoiding excessive alcohol consumption. Can nonalcoholic fatty liver disease be cured? While no specific cure exists, nonalcoholic fatty liver disease can often be reversed through sustained weight loss, dietary improvements, regular exercise, and proper management of associated metabolic conditions. What are the complications of nonalcoholic fatty liver disease? Untreated nonalcoholic fatty liver disease can progress to liver inflammation, fibrosis, cirrhosis, liver failure, and increased risk of liver cancer, making early intervention crucial for prevention. References 1. https://www.nhs.uk/conditions/non-alcoholic-fatty-liver-disease/ 2. https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/treatment 3. https://medlineplus.gov/genetics/condition/non-alcoholic-fatty-liver-disease/ 4. https://www.mdpi.com/2227-9717/9/1/135
Semen Retention: What It Is, Myths & Possible Health Effects
What is Semen Retention? Semen retention is the intentional practice of avoiding ejaculation, either through complete abstinence from sexual activity or by engaging in sexual activity without reaching climax. This behavioural practice has roots in several spiritual and religious traditions, including certain forms of Taoism and Tantric practices. The semen retention meaning encompasses different aspects. Some practitioners abstain completely from masturbation and sexual activity, while others engage in sexual stimulation but stop before ejaculation occurs. This technique, sometimes called coitus reservatus, involves attempting to achieve orgasm without semen release. Modern interest in semen retention has expanded through online communities and social media, where individuals share anecdotal claims of enhanced energy, focus, and confidence. However, it's important to understand that these claims largely lack robust scientific evidence. The Science Behind Semen Retention From a medical perspective, semen retention represents a voluntary period of ejaculatory abstinence. Research on this topic primarily focuses on semen parameters and fertility rather than the broader health claims often associated with the practice. Current scientific evidence shows that sperm production continues normally in the testes regardless of ejaculation frequency. When ejaculation doesn't occur, older sperm naturally break down and are reabsorbed by the body through normal physiological processes. This is similar to what happens after a vasectomy and doesn't result in any harmful accumulation. Studies examining ejaculatory abstinence suggest that shorter periods (typically less than seven days) may improve sperm motility and viability compared with prolonged abstinence. This finding challenges the assumption that extended semen retention necessarily enhances sperm quality or overall health. How Semen Retention Works Understanding how semen retention functions requires examining the physiological processes involved: Complete abstinence approach - Individuals avoid all sexual activity, including masturbation, for predetermined periods Modified sexual behaviour - Practitioners engage in sexual activity but deliberately avoid ejaculation using techniques such as edging Physiological response - Sperm production continues normally, while unused sperm are naturally reabsorbed by the body Psychological effects - Many practitioners report subjective changes in mood, energy, and motivation The body's natural sperm production cycle continues regardless of ejaculation patterns. New sperm cells replace those that are reabsorbed, maintaining the reproductive system's normal function without any medical intervention required. Myths and Misconceptions About Semen Retention Several misconceptions surround semen retention, often perpetuated by online communities and social media content: • Myth: Semen is too nutritionally valuable to waste Reality: Semen does contain nutrients like zinc and amino acids, but these are present in minimal quantities compared with normal dietary intake • Myth: Semen retention dramatically increases testosterone long-term Reality: Scientific evidence for sustained increases in testosterone due to semen retention is weak and inconsistent • Myth: Avoiding ejaculation boosts athletic performance Reality: No high-quality clinical trials have demonstrated direct performance benefits from semen retention • Myth: Frequent ejaculation harms prostate health Reality: Large cohort studies indicate that more frequent ejaculation may be associated with a reduced risk of prostate cancer • Myth: Semen retention treats mental health conditions Reality: No major medical organisation recommends semen retention as treatment for anxiety, depression, or ADHD Health Benefits of Semen Retention The benefits of semen retention remain largely anecdotal, with limited direct clinical evidence supporting most popular claims: • Improved sexual self-awareness - Some men report a better understanding of their arousal patterns and greater control during sexual activity • Indirect lifestyle benefits - Practitioners often simultaneously adopt healthier habits like reduced pornography use, increased exercise, and better sleep • Subjective energy and focus improvements - Many report feeling more motivated and focused, though these effects lack scientific validation • Short-term fertility considerations - Research suggests shorter abstinence periods may improve sperm motility for fertility planning It's crucial to understand that most widely advertised semen retention benefits, such as massive testosterone boosts or guaranteed muscle growth, lack robust scientific support. Any positive effects likely result from accompanying lifestyle changes rather than semen retention itself. Potential Risks of Semen Retention While semen retention isn't physically dangerous for healthy individuals, several potential risks deserve consideration: • Increased psychological pressure - Strict self-imposed rules regarding ejaculation may cause anxiety, guilt, or distress if goals are not achieved • Relationship impact - Partners may feel rejected, confused, or excluded if the practice isn’t discussed openly without clear communication about semen retention practices • Delayed medical attention - Focusing on semen retention might cause men to ignore underlying sexual health issues requiring professional evaluation • Misinformation reliance - Social media content about semen retention often contains inaccurate or exaggerated claims Does Semen Retention Improve Sexual Health? The relationship between semen retention and sexual health is complex and remains largely understudied. Some men report improved sexual control and awareness through practices that delay ejaculation, which may help with conditions like premature ejaculation. However, these benefits likely stem from increased mindfulness about sexual responses rather than semen retention itself. A systematic review published in PubMed Central found that shorter ejaculatory abstinence may improve sperm motility (particularly progressive motility and velocity) even though semen volume and sperm concentration may be lower. Evidence remains insufficient for advanced markers like DNA fragmentation, ROS, antioxidant capacity, and pregnancy outcomes, so guideline “ideal abstinence” ranges may warrant re-evaluation. For men experiencing sexual health concerns, including premature ejaculation, retrograde ejaculation, or sperm cramps, consulting healthcare professionals remains the most appropriate approach. These conditions require proper medical evaluation and evidence-based treatment rather than unproven practices. Semen Retention in Modern Culture Social media platforms and online communities have significantly influenced modern perceptions of semen retention. Popular culture often portrays this practice as a pathway to enhanced masculinity, success, and vitality. However, recent studies examining men's health content on social media found that semen retention discussions frequently contain inaccurate information not produced by medical experts. This disconnect between popular claims and scientific evidence highlights the importance of seeking reliable health information from qualified medical sources rather than social media influencers or unverified online communities. How to Practice Semen Retention Safely For those considering semen retention despite limited scientific evidence, safety considerations include: • Start gradually - Avoid extreme or prolonged abstinence that might create psychological stress or relationship strain • Communicate openly - Discuss intentions with sexual partners to maintain healthy relationships • Monitor mental health - Be aware of any anxiety, guilt, or obsessive thoughts related to the practice • Seek medical advice - Consult healthcare providers if experiencing sexual health concerns • Maintain realistic expectations - Understand that dramatic health transformations are unlikely based on current evidence Remember that sexual health encompasses physical, emotional, and relational well-being, requiring balanced approaches rather than extreme practices. Semen Retention and Mental Health Claims about semen retention's mental health benefits remain largely anecdotal: • Reported mood improvements - Some practitioners describe feeling more confident and motivated • Potential placebo effects - Positive expectations might contribute to perceived benefits • Lifestyle factor confusion - Concurrent healthy changes might explain any mental health improvements • Risk of psychological distress - Overly rigid rules about ejaculation can trigger anxiety, obsessive behaviours, or guilt Mental health conditions require evidence-based treatments, and semen retention shouldn't replace professional care for anxiety, depression, or other psychological concerns. Semen Retention and Physical Performance Athletic and physical performance claims associated with semen retention lack scientific validation: • No proven strength benefits - High-quality studies don't support muscle growth or strength improvements • Testosterone misconceptions - Claims about dramatic hormone increases aren't supported by research • Energy level reports - Subjective energy improvements likely result from lifestyle changes rather than semen retention • Performance anxiety - Excessive focus on avoiding ejaculation may increase stress and impair athletic or sexual performance Athletes seeking performance improvements should focus on proven strategies like proper nutrition, training, and recovery rather than unvalidated practices. Conclusion Semen retention is largely a personal or cultural practice, and while some individuals report subjective benefits such as improved focus or self-control, current medical evidence does not support extreme claims about dramatic hormonal or physical changes. Men’s sexual and reproductive health is influenced by a combination of lifestyle, mental well-being, and underlying physiological factors, making informed, evidence-based decisions far more reliable than relying on myths or online trends. For a clearer understanding of your health, Metropolis Healthcare offers more than 4,000 diagnostic tests, comprehensive full-body health checkups, and advanced speciality testing, supported by accurate reporting and quick turnaround times. With convenient booking via website, call, app, or WhatsApp, and a strong home sample collection network spanning 10,000+ touchpoints, Metropolis makes proactive health monitoring accessible, reliable, and patient-friendly. FAQs What is the purpose of semen retention? Practitioners cite various purposes for semen retention, including spiritual growth, improved energy, and enhanced focus. However, these goals lack scientific validation, and the practice primarily represents a behavioural choice rather than a medical treatment with proven benefits. Are there health risks associated with semen retention? Semen retention isn't physically harmful for healthy individuals, but potential risks include psychological stress, relationship strain, and delayed medical attention for underlying sexual health issues. The practice may also lead to reliance on misinformation about male health. Does semen retention increase testosterone? Current evidence doesn't support claims that semen retention significantly increases testosterone levels long-term. While some small studies suggest minor fluctuations, these changes aren't medically significant or proven to improve health, strength, or mood. How long should one practice semen retention for the benefits? There's no evidence-based recommendation for semen retention duration because the practice lacks proven health benefits. Any positive effects reported by practitioners likely result from concurrent lifestyle improvements rather than ejaculation avoidance itself.