Preventive Healthcare
What is Nonalcoholic Fatty Liver Disease? Symptoms, Causes, and Treatment
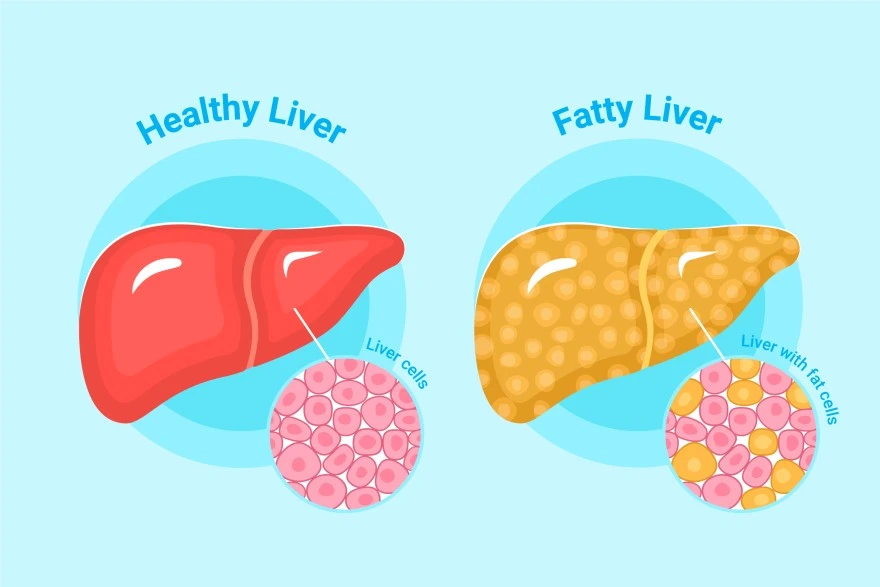
Table of Contents
What is Nonalcoholic Fatty Liver Disease?
Nonalcoholic fatty liver disease, now officially termed metabolic dysfunction-associated steatotic liver disease (MASLD), is a condition where excess fat builds up in liver cells in people who consume minimal alcohol. This liver disease is strongly linked to overweight or obesity, type 2 diabetes, abnormal blood lipids, and other features of metabolic syndrome.
Many people develop simple steatosis, which involves fat accumulation without significant inflammation. However, a more serious form called metabolic dysfunction-associated steatohepatitis (MASH), previously known as nonalcoholic steatohepatitis (NASH), includes liver inflammation and cell injury. If left untreated, this progressive liver disease can advance to fibrosis, cirrhosis, liver failure, or even hepatocellular carcinoma (liver cancer).
A concerning aspect of nonalcoholic fatty liver disease is that it often causes no symptoms, particularly in its early stages. Many people discover they have this condition incidentally during routine blood tests or imaging performed for other reasons. This silent progression makes regular health monitoring crucial for early detection and management.
Symptoms of Nonalcoholic Fatty Liver Disease
Recognizing the symptoms of nonalcoholic fatty liver disease can be challenging because the condition often remains silent in its early stages. When nonalcoholic fatty liver disease symptoms do appear, they typically include:
- Persistent fatigue or feeling unusually tired throughout the day
- General malaise or feeling unwell without a specific cause
- Dull pain or discomfort in the upper right abdomen, where the liver is located
- Unexplained weakness affecting daily activities
- Loss of appetite and unintentional weight loss, particularly in advanced stages
- Nausea or feeling sick to your stomach
- Itchy skin (pruritus) as the condition progresses
- Yellowing of skin and eyes (jaundice) in advanced disease
- Abdominal swelling from fluid buildup (ascites)
- Swelling in legs and ankles (oedema)
- Spider-like blood vessels (spider angiomas) under the skin in liver cirrhosis
- Mental confusion or difficulty concentrating in severe disease
- Gastrointestinal bleeding from enlarged veins in advanced liver cirrhosis
Common Symptoms and Their Impact on Daily Life
Since nonalcoholic fatty liver disease often remains silent, you might feel completely normal or notice only subtle fatigue or vague right-sided abdominal discomfort. These symptoms can easily be mistaken for stress, indigestion, or general fatigue.
Persistent tiredness and weakness significantly reduce your energy levels, productivity, and exercise tolerance. This creates a challenging cycle where reduced physical activity makes it harder to maintain the healthy lifestyle crucial for managing fatty liver disease.
As the condition progresses to MASH and potentially liver cirrhosis, symptoms like poor appetite, nausea, abdominal swelling, leg swelling, itching, and sleep problems can severely affect your eating patterns, mobility, sleep quality, and mood.
Causes of Nonalcoholic Fatty Liver Disease
Nonalcoholic Fatty liver disease develops when the liver stores more fat than it can process or eliminate, typically occurring alongside metabolic dysfunction. The major risk factors for developing fatty liver disease include obesity (particularly excess abdominal fat), insulin resistance, prediabetes or type 2 diabetes, high triglycerides, abnormal cholesterol levels, and high blood pressure. These conditions often occur together as metabolic syndrome, creating an environment where the liver accumulates fat.
Additional contributing factors include rapid weight loss, certain medications (such as some cancer drugs, corticosteroids, and calcium channel blockers), bowel diseases that affect nutrient absorption, and previous bariatric surgery. Hormonal factors, genetics, and changes in gut bacteria also influence how individuals store fat and develop liver inflammation.
Interestingly, fatty liver disease can occasionally occur in people without obvious risk factors, suggesting that genetic predisposition and environmental factors play important roles. This condition becomes more common after age 40 and affects men and women differently, with postmenopausal women showing increased risk.
How Lifestyle and Diet Contribute to NAFLD
Diets high in calories, added sugars (especially fructose from soft drinks), refined carbohydrates, and saturated fats promote weight gain and insulin resistance, leading to fat accumulation in the liver.
Physical inactivity compounds these effects by reducing your body's ability to burn fat and regulate blood sugar effectively. When you consume more calories than you burn, the excess energy gets stored as fat, including in liver cells. Over time, this fat accumulation triggers inflammation and can progress to more serious liver diseases.
Conversely, adopting healthier eating patterns and increasing physical activity can dramatically improve liver health. Research shows that even modest weight loss of 3-5% of body weight can significantly reduce liver fat. Regular exercise enhances insulin sensitivity and helps your body use fat more efficiently, reducing the burden on your liver.
How to Diagnose Nonalcoholic Fatty Liver Disease
Doctors usually suspect nonalcoholic fatty liver disease when blood tests show mildly elevated liver enzymes such as ALT and AST, or when imaging performed for other reasons reveals fatty liver changes. The diagnostic process begins with a detailed medical history, including your alcohol intake, current medications, and metabolic risk factors.
During physical examination, doctors look for signs of liver diseases such as an enlarged liver, abdominal swelling, or skin changes that might indicate advanced disease. This comprehensive assessment helps distinguish nonalcoholic fatty liver disease from other liver conditions and determines the appropriate diagnostic approach.
Additional blood tests help rule out other causes of liver disease, including viral hepatitis, autoimmune liver disease, and haemochromatosis. When advanced scarring is suspected or the diagnosis remains uncertain, doctors may recommend a liver biopsy to distinguish simple fatty liver from steatohepatitis and accurately stage any fibrosis.
Imaging and Diagnostic Tests to Identify NAFLD
- Ultrasound examination: Often the first imaging test performed; shows increased liver echogenicity, suggesting fat infiltration.
- CT scan: Reveals reduced liver density compared to the spleen, indicating fat accumulation.
- MRI and specialised MRI techniques: Provide more accurate quantification of liver fat content.
- Transient elastography (FibroScan): Uses ultrasound technology to measure liver stiffness and estimate fibrosis severity.
- FibroMax (Fibrosis, Activity, Steatosis, ASH, and NASH) panel: Provide a comprehensive assessment of liver fibrosis, steatosis, inflammation, hepatitis and cirrhosis.
- Liver Function Test (LFT): Measure ALT, AST, alkaline phosphatase, and bilirubin levels.
- Comprehensive Metabolic Panel: Assesses liver and kidney function and electrolyte balance.
- Fatty Liver Profile: Aids in differentiating fatty liver from other liver diseases.
- Liver Biopsy: Gold standard for distinguishing simple steatosis from steatohepatitis when necessary.
Treatment Options for Nonalcoholic Fatty Liver Disease
Currently, no specific medication can cure nonalcoholic fatty liver disease, making lifestyle modification the cornerstone of treatment. The primary goal focuses on addressing underlying metabolic risk factors through sustained lifestyle changes that promote gradual, healthy weight loss.
According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), losing approximately 7-10% of your body weight can reduce liver fat, improve inflammation, and may even reverse early fibrosis. This weight loss should occur gradually through a combination of calorie-controlled eating and increased physical activity.
Managing associated medical conditions is equally important. Controlling blood sugar in diabetes, lowering cholesterol and triglycerides, and treating high blood pressure reduces risks for both liver and cardiovascular complications. For selected patients, particularly those with obesity and difficult-to-control diabetes, bariatric surgery can significantly improve fatty liver disease and steatohepatitis.
How to Manage and Treat NAFLD Effectively
- Achieve gradual weight loss through sustainable dietary changes and regular physical activity.
- Follow a Mediterranean-style diet emphasizing vegetables, fruits, whole grains, lean proteins, and healthy fats.
- Limit added sugars and refined carbohydrates, particularly sugary beverages and processed foods.
- Exercise regularly, aiming for at least 150 minutes of moderate-intensity activity per week.
- Manage diabetes effectively through medication compliance and blood sugar monitoring.
- Control cholesterol and triglyceride levels with appropriate medications when necessary.
- Maintain healthy blood pressure through lifestyle modifications and medications if needed.
- Avoid alcohol entirely to prevent additional liver stress.
- Monitor liver function regularly through scheduled blood tests and imaging.
Conclusion
Nonalcoholic fatty liver disease (MASLD) represents a growing global health concern affecting millions worldwide. Understanding the definition of nonalcoholic fatty liver disease, recognising its symptoms, and knowing its causes empower you to take proactive steps towards better liver health. While the condition often remains silent in its early stages, implementing lifestyle changes focused on gradual weight loss, healthy eating, and regular exercise can significantly improve outcomes and prevent progression to liver cirrhosis or liver failure.
The key to managing fatty liver disease lies in addressing underlying metabolic risk factors through sustainable lifestyle modifications. Regular monitoring through appropriate diagnostic tests helps track your progress and adjust treatment strategies as needed.
At Metropolis Healthcare, we understand the importance of early detection and monitoring in managing liver diseases effectively. Our comprehensive portfolio of over 4,000 tests includes specialised liver function panels and metabolic assessments that deliver accurate and timely results. With our extensive network of a network of over 220 laboratories and 10,000+ convenient home sample collection points across India, accessing quality diagnostic care has never been easier.
FAQs
What causes nonalcoholic fatty liver disease?
Nonalcoholic fatty liver disease primarily results from metabolic dysfunction, including obesity, insulin resistance, diabetes, high triglycerides, and metabolic syndrome, leading to excess fat accumulation in liver cells.
How can nonalcoholic fatty liver disease be prevented?
Prevention involves maintaining a healthy weight, eating a balanced diet low in added sugars, exercising regularly, managing diabetes and cholesterol levels, and avoiding excessive alcohol consumption.
Can nonalcoholic fatty liver disease be cured?
While no specific cure exists, nonalcoholic fatty liver disease can often be reversed through sustained weight loss, dietary improvements, regular exercise, and proper management of associated metabolic conditions.
What are the complications of nonalcoholic fatty liver disease?
Untreated nonalcoholic fatty liver disease can progress to liver inflammation, fibrosis, cirrhosis, liver failure, and increased risk of liver cancer, making early intervention crucial for prevention.
References
1. https://www.nhs.uk/conditions/non-alcoholic-fatty-liver-disease/
2. https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash/treatment
3. https://medlineplus.gov/genetics/condition/non-alcoholic-fatty-liver-disease/
4. https://www.mdpi.com/2227-9717/9/1/135




























