Web Stories
Latest Blogs
Hyoid Bone: Functions, Structure, and Common Disorders Explained
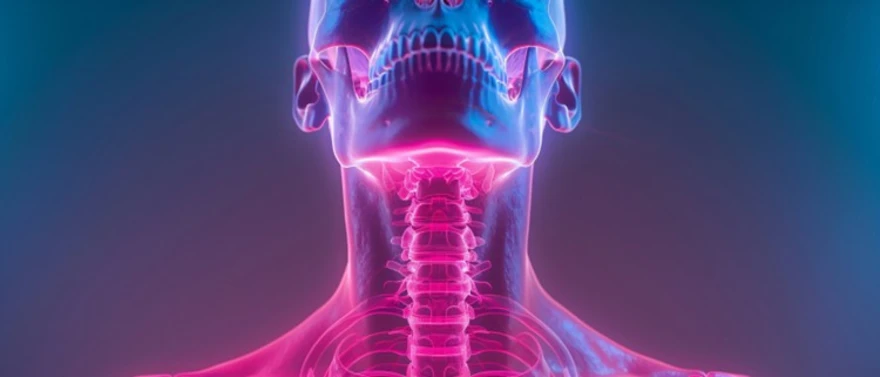
What is the Hyoid Bone? The hyoid bone is a small, U-shaped bone located in the front of the neck that plays a critical role in swallowing, speech, and airway protection. Unlike most bones in the human body, the hyoid bone does not directly articulate with any other bone. Instead, it is suspended by a network of muscles and ligaments, allowing it to serve as a stable anchor for the tongue and throat. Despite its small size, the hyoid bone is essential for everyday functions such as talking, chewing, breathing, and swallowing. As noted in a study published in StatPearls (NCBI), its unique “free-floating” design—supported by muscles and ligaments rather than direct bone-to-bone connections—makes it central to coordinated swallowing and speech, while also helping protect the airway. Where is the Hyoid Bone Located? The hyoid bone is located in the anterior neck, positioned between lower jaw (mandible) and the thyroid cartilage (Adam’s apple). It typically lies at the level of the third cervical vertebra (C3). This strategic placement allows the hyoid bone to coordinate movements between the tongue, larynx, and pharynx during swallowing and speech. Because it is protected by soft tissues rather than other bones, the hyoid bone is relatively mobile yet vulnerable to trauma. Anatomy of the Hyoid Bone The hyoid bone anatomy consists of three main components that work together to support its various functions: Body (Corpus): Central, thick portion that forms the main structure. Rectangular shape with a slightly curved front surface. Provides the primary attachment point for tongue muscles. Greater Horns (Greater Cornua): Two long, curved projections extend backward from each end. Serve as attachment sites for major neck and throat muscles. Help coordinate swallowing and speech movements. Lesser Horns (Lesser Cornua): Small, conical projections that point upward. Connect to ligaments that suspend the hyoid bone. Provide stability for the floating bone structure. What Makes the Hyoid Bone Unique? The hyoid bone is unique because: It is the only bone in the body that does not articulate with another bone It is suspended entirely by muscles and ligaments It serves as a floating support structure for the tongue and larynx Its movement is essential for coordinated swallowing and speech This anatomical uniqueness makes the hyoid bone both highly functional and clinically significant. Functions of the Hyoid Bone The hyoid bone function extends across multiple vital processes: Supports the tongue during speech and swallowing Anchors the muscles of the floor of the mouth Assists in jaw movement and stabilisation Helps elevate the larynx during swallowing Maintains airway patency during breathing Disruption of these functions can cause difficulty swallowing (dysphagia), changes in voice, or breathing difficulties. Role of Hyoid Bone in Speech and Voice Production During speech, the hyoid bone provides a stable base for tongue movement and laryngeal positioning. Subtle adjustments in its position allow modulation of pitch, tone, and articulation. Because the hyoid bone coordinates tongue and voice box movement, disorders affecting it may result in hoarseness, vocal fatigue, or difficulty pronouncing certain sounds. Hyoid Bone and Airway Protection The hyoid bone plays a key role in airway protection during swallowing. As food is swallowed, the hyoid bone elevates and moves forward, helping close the airway and prevent aspiration of food or liquids into the lungs. Impairment of this mechanism can increase the risk of choking or recurrent respiratory infections. Common Hyoid Bone Disorders Several conditions can affect the hyoid bone, including: A hyoid bone fracture, usually due to blunt neck trauma, strangulation, or road accidents. Hyoid bone syndrome, a rare condition characterised by chronic throat or neck pain caused by abnormal movement or ligament strain. Muscle strain or inflammation around the hyoid attachments. Degenerative or age-related stiffness. Post-surgical or post-intubation irritation or inflammation. Although rare, these conditions require prompt evaluation due to their proximity to vital airway structures. Diagnosis of Hyoid Bone Disorders Diagnosis begins with a detailed clinical history and physical examination. Doctors assess pain, swallowing difficulty, voice changes, and a history of trauma. Imaging studies are often required to confirm structural abnormalities, displacement, or fractures, especially when symptoms are persistent or severe. Tests for Hyoid Bone Disorders When doctors suspect hyoid bone problems, they may recommend several diagnostic tests: Clinical exam (palpation + pain on swallowing/neck movement) Neck X-ray (initial screen) CT scan neck (best for hyoid bone fracture/displacement) MRI neck (soft-tissue/muscle–ligament injury) Flexible laryngoscopy (voice/airway symptoms) Swallow study (VFSS/MBSS) (swallowing difficulty) CBC, ESR, and inflammatory markers (if infection or inflammation is suspected) Treatment Options for Hyoid Bone Problems Treatment approaches vary depending on the specific condition affecting your hyoid bone: Conservative management Rest and avoidance of activities that aggravate symptoms Anti-inflammatory/pain medicines Physical therapy to improve neck–throat muscle coordination Specialised therapies Speech therapy (voice/articulation issues) Swallowing therapy (dysphagia) Soft-tissue or myofascial therapy for muscle spasm and tension Surgical treatment Rare; considered mainly for severe or displaced fractures or persistent symptoms not improving with conservative care May involve repair/removal of the affected segment based on specialist evaluation Hyoid Bone Variations in Children vs Adults The hyoid bone undergoes significant changes throughout life, with important differences between children and adults. In infants and young children, the hyoid bone sits higher in the neck, at approximately the C2-C3 level, and is largely cartilaginous rather than bony. As children grow, the hyoid bone gradually descends to its adult position, typically between C4 and C5. The cartilaginous portions slowly ossify, becoming fully bony by adulthood. This developmental process affects the bone's vulnerability to injury, with children's cartilaginous hyoid bones being more flexible and less prone to fracture. In elderly adults, the hyoid bone may become more brittle and susceptible to fracture even from minor trauma. Age-related changes in surrounding muscles and ligaments can also affect the mobility and function of the hyoid bone. When to See a Doctor for Hyoid Bone Pain or Injury You should seek medical attention for hyoid bone-related symptoms in several situations: Immediate Medical Care: Severe neck pain following trauma or injury Difficulty swallowing or breathing Sudden voice changes or loss of voice Signs of neck swelling or bruising Routine Medical Evaluation: Persistent neck pain lasting more than a few days Gradual changes in swallowing function Chronic throat discomfort or voice problems Recurring episodes of neck muscle tension Emergency Situations: Any breathing difficulties or airway obstruction Severe trauma to the neck area Signs of infection with fever and neck pain Conclusion The hyoid bone is small but vital for swallowing, speech, and airway protection. If you have persistent neck/throat pain, changes in your voice, difficulty swallowing, or any neck injury, get evaluated early to avoid complications. If you’re being assessed for throat or neck symptoms, Metropolis Healthcare supports your diagnostic journey with 4,000+ tests, speciality testing, and comprehensive full-body checkups—backed by accurate results and a quick turnaround. You can book easily via website, call, app, or WhatsApp, and opt for home sample collection through our strong network of 10,000+ touchpoints, making reliable testing convenient and accessible. FAQs What is the function of the hyoid bone? Supports the tongue Assists in swallowing Stabilises the larynx Helps protect the airway Why is the hyoid bone unique? The hyoid bone is unique because it does not connect directly to any other bone and is suspended entirely by muscles and ligaments. Can the hyoid bone break? Yes, a hyoid bone fracture can occur, usually due to blunt neck trauma, though it is rare. What causes pain in the hyoid bone? Muscle strain Hyoid syndrome Inflammation Trauma or fracture Post-surgical irritation Is the hyoid bone important for speech? Yes, it plays a vital role in tongue positioning and voice modulation during speech. What muscles attach to the hyoid bone? Suprahyoid muscles Infrahyoid muscles Tongue and laryngeal muscles Can a person live without a hyoid bone? Severe impairment of hyoid function would significantly affect swallowing and speech, making normal function difficult. What happens if the hyoid bone is damaged? Damage may cause pain, difficulty swallowing, changes in voice, or breathing problems. How is a hyoid bone fracture diagnosed? Diagnosis is confirmed using imaging, most commonly a CT scan of the neck. Does the hyoid bone grow with age? The hyoid bone gradually ossifies and becomes more rigid with age, especially from adolescence into adulthood.
Understanding the Sternum: Functions, Symptoms of Injury, and Conditions
What Is Sternum? The sternum, commonly called the breastbone, is a flat, elongated bone that forms the central front portion of your chest wall. This elongated, flat bone serves as the anchor point for your rib cage and provides structural support to your entire thoracic region. Your sternum measures approximately 15–20 centimetres (about 6–8 inches) in length and consists of dense, protective bone tissue. The breastbone develops through a process in which separate bone segments gradually fuse during childhood and adolescence. This fusion creates the solid, unified structure that protects your heart, lungs, and other vital organs throughout your life. Where Is the Sternum Located? The sternum location is precisely in the midline of your chest, running vertically along your body's central axis. You can easily locate your breastbone by placing your hand flat against the centre of your chest, just below your collarbone. Your sternum extends from the base of your neck down to the upper abdomen, forming the front wall of your rib cage. Anatomy of the Sternum Manubrium: The broad, upper portion that connects to your collarbones and first two ribs Body (Gladiolus): The longest middle section that attaches to ribs three through seven Xiphoid Process: The small, pointed lower tip that varies in shape between individuals Key anatomical features include: Sternal Angle: The critical junction between the manubrium and body, serving as a landmark for the second rib Clavicular Notch: Grooves on either side of the manubrium where your collarbones attach Suprasternal Notch: The hollow at the top of your breastbone, easily felt at the base of your throat Costal Notches: Indentations along the sides where rib cartilages attach to the sternum Parts of the Sternum Explained The manubrium forms the uppermost portion of your sternum and serves as the attachment point for your first two ribs and both collarbones. This broad, shield-like segment measures approximately 5 to 6 centimetres in height. It provides crucial stability for your shoulder girdle, helping transfer forces from your arms and shoulders through the chest wall. The body of the sternum, also called the gladiolus, is the longest segment at around 10 to 12 centimetres. It contains ridges where ribs two to seven attach, supporting muscle attachment and protecting the heart and major vessels. The xiphoid process is small but significant, remaining cartilaginous until later adulthood and serving as an attachment for the diaphragm and abdominal muscles. How Does the Sternum Connect to the Rib Cage? The sternum connects to your rib cage through a sophisticated system of costal cartilages that form sternocostal joints. These flexible connections allow your chest to expand and contract during breathing while maintaining structural stability. The manubrium attaches to the first and second ribs, while the body connects to ribs 2–7 through these cartilaginous joints. This connection system forms the anterior (front) portion of your rib cage, providing a protective enclosure for your vital organs. The sternum's function includes serving as the central anchor point that helps coordinate rib movements during respiration. Functions of the Sternum Structural Support: Provides the central framework for your entire rib cage system Organ Protection: Creates a bony shield protecting your heart, lungs, and major blood vessels from frontal impacts Respiratory Facilitation: Enables chest wall movements essential for breathing by serving as the anchor point for rib attachments Muscle Attachment: Offers connection points for essential muscles, including the pectoralis major and sternocleidomastoid Additional sternum functions include: Anatomical Landmark: Healthcare providers use the breastbone as a reference point for medical procedures and examinations Blood Cell Production: The bone marrow within the sternum produces red and white blood cells and platelets Calcium Storage: Like other bones, the sternum stores calcium and other minerals essential for metabolic processes Sternum and Its Role in Protecting Vital Organs The breastbone, working together with your rib cage, creates a shield that safeguards your heart, lungs, thymus gland, and major blood vessels from frontal trauma and impacts. This protective function becomes particularly important during accidents, sports activities, or emergency medical procedures like CPR. The sternum's central location and solid construction help absorb and distribute impact forces, reducing the risk of severe internal injuries. Simple actions like carrying heavy objects or playing contact sports rely on the breastbone's structural integrity to protect your vital organs. Sternum Anatomy in Men, Women, and Children Men typically have broader, thicker sterna than women, reflecting overall differences in chest wall dimensions and muscle mass. In children and adolescents, the sternum anatomy differs significantly from that of adults. The entire breastbone, particularly the xiphoid process, remains cartilaginous mainly during childhood, gradually ossifying as development progresses. In some children and adults, incomplete fusion of the sternum may result in a small opening known as a sternal foramen. Adult sterna show more complete calcification and may develop age-related changes or deformities such as pectus excavatum (sunken chest) or pectus carinatum (protruding chest). Common Sternum Disorders & Conditions Sternal Foramen: A harmless hole in the breastbone from incomplete fusion during development Pectus Excavatum: A sunken chest deformity that may compress internal organs Pectus Carinatum: A protruding chest deformity creating a 'pigeon chest' appearance Costochondritis: Inflammation of the cartilage connecting ribs to the sternum, causing chest pain Sternal Osteomyelitis: A serious bone infection requiring immediate medical attention Sternal Fractures: Usually result from severe blunt force trauma, such as car accidents Sternocostal Joint Injuries: Damage to the connections between ribs and sternum Causes of Sternum Pain Chest trauma or injury from falls, car accidents, or sports impacts, potentially causing bruising, contusion, or sternal fracture. Costochondritis, inflammation of the cartilage where your ribs attach to the sternum Tietze syndrome, similar to costochondritis but with visible swelling of one or more costochondral joints Muscle strain affecting chest wall muscles from heavy lifting, intense exercise, or persistent coughing Surgical procedures involving the sternum, such as open-heart surgery, can lead to postoperative discomfort. Osteoarthritis or degenerative joint disease can affect the joints connecting the sternum and ribs. Inflammatory conditions such as rheumatoid arthritis and ankylosing spondylitis affect the joints of the chest wall. Bone infections of the sternum sometimes occur after surgery or trauma. Primary bone tumours or metastases (cancer spread) affecting the sternum. Gastro-oesophageal reflux disease causes burning sensations behind the breastbone. Cardiac causes, including angina or myocardial infarction (heart attack), require immediate medical attention. Pulmonary conditions such as pneumonia or pulmonary embolism (blood clots in the lungs). Anxiety or panic attacks cause chest tightness near the sternum. Sternum Pain After Exercise or Coughing Sternum pain following physical activity or persistent coughing typically results from strain or inflammation of the chest wall structures that attach to or move with your breastbone. High-intensity upper-body workouts can overload the chest wall muscles, costal cartilages, and joints attached to the sternum, leading to costochondritis, muscle strain, or irritation of the xiphoid process. Similarly, prolonged forceful coughing from respiratory infections places significant stress on the ribs and costochondral joints, producing sharp or aching pain in the chest. The repetitive motion of coughing creates tension in the chest wall muscles and can inflame the delicate cartilage connections between your ribs and sternum. How are Sternum Conditions Diagnosed? Detailed medical history, including onset, duration, character, and triggers of pain Assessment of recent trauma, surgery, infections, or new exercise routines Physical examination with palpation to reproduce pain patterns Chest X-rays to detect fractures, lung problems, or heart size changes CT scans for detailed evaluation of bone alignment, tumours, or post-surgical complications MRI to assess bone marrow, cartilage, soft tissues, and potential infections Ultrasound for evaluating superficial tissues and guiding procedures Blood tests for inflammatory markers (such as CRP Test, hsCRP (High Sensitivity CRP) Test) when infection is suspected Cardiac enzyme tests (such as troponin I/T, CK-MB, or comprehensive cardiac profiles) to rule out a heart attack if symptoms suggest cardiac involvement Complete blood count to assess for signs of infection or inflammation Electrocardiogram (ECG) to evaluate heart rhythm and detect cardiac issues Bone scans to identify areas of increased bone activity from fractures or tumours Pulmonary function tests or specialized panels (such as an ILD Complete profile if lung involvement is suspected) if breathing difficulties accompany chest pain Treatment Options for Sternum Injuries & Pain Rest and avoid activities that exacerbate your pain Pain relievers that help with inflammation, like ibuprofen, according to the NHS Cold therapy using ice packs during the first 48-72 hours for acute injuries Heat application after the initial period to relax muscles and reduce stiffness Physical therapy involving guided stretching and strengthening exercises Corticosteroid injections into affected costochondral joints may relieve persistent inflammation and pain Antibiotics for bone infections affecting the sternum Disease-modifying therapies for inflammatory arthritis conditions Acid-suppressing medications for reflux-related chest pain Surgical fixation for significantly displaced fractures Chest wall stabilisation procedures for complex injuries Recovery Time for Sternum Fractures & Inflammation Recovery timelines for sternum-related conditions vary considerably depending on the specific diagnosis, injury severity, and individual healing factors. For sternal fractures, healing typically takes 6-8 weeks for the bone to unite sufficiently, though complete recovery may require 3-6 months. During this period, you'll need activity restrictions to prevent displacement of fracture fragments. Costochondritis and other inflammatory conditions usually respond to treatment within 2-6 weeks, though some cases may persist for several months. Factors that influence recovery include age, overall health status, adherence to treatment recommendations, and the presence of underlying conditions like arthritis or autoimmune diseases. When is Sternum Pain an Emergency? Severe, crushing, or squeezing chest pain that radiates to your arms, neck, jaw, or back Chest pain accompanied by shortness of breath, sweating, nausea, or dizziness Sudden, sharp chest pain with difficulty breathing may indicate a blood clot in your lungs. Chest pain following significant trauma (such as a car accident or major fall). Rapid or irregular heartbeat combined with chest discomfort Fainting or loss of consciousness associated with chest pain Chest pain that doesn't improve with rest or worsens progressively Prevention Tips for Sternum Injuries Wearing appropriate seat belts and ensuring proper airbag function in vehicles Using proper protective equipment during sports and recreational activities Maintaining good posture to reduce strain on the chest wall muscles Avoiding activities that put excessive stress on your chest area when recovering from injury Learning proper lifting techniques to prevent muscle strain Maintaining a healthy body weight to reduce stress on your chest and musculoskeletal system Managing underlying conditions such as arthritis or osteoporosis that may increase fracture risk Avoiding smoking, which can weaken bones and impair healing Ensuring adequate calcium and vitamin D intake for bone health Managing stress levels, as tension can contribute to muscle strain and pain Following proper safety protocols in high-risk occupations When to See a Doctor Chest pain that persists for more than a few days despite rest and over-the-counter pain relief Gradually worsening chest discomfort that interferes with daily activities Chest pain accompanied by swelling, redness, or warmth over the sternum area Recurring episodes of chest pain, particularly if they're becoming more frequent or severe Chest pain associated with fever, persistent cough, or difficulty breathing New chest symptoms if you have a history of heart disease, cancer, or other serious medical conditions Conclusion Understanding your sternum anatomy and function empowers you to recognise potential chest-related concerns and seek appropriate medical care. The breastbone's central role in protecting vital organs and supporting respiratory function makes it essential to address any persistent chest pain or discomfort promptly. Key takeaways include recognising that costochondritis and other sternum conditions are treatable, understanding the normal location and anatomy of the sternum, and knowing when chest symptoms warrant medical evaluation. Early intervention often leads to better outcomes and prevents complications. If you experience persistent chest pain, breathing difficulties, or concerns about your chest wall structure, consult a doctor for proper evaluation. At Metropolis Healthcare, we support your journey toward better chest health with comprehensive diagnostic services. Our network of over 220 laboratories and 4,600 service centres ensures access to accurate testing when you need it most. With convenient home sample collection available at 10,000+ touchpoints across India, you can access essential blood tests and health screenings to identify underlying conditions contributing to chest symptoms. FAQs What is the function of the sternum? Protects vital organs, including the heart, lungs, and major blood vessels Provides attachment points for ribs, forming the protective rib cage structure Serves as an anchor point for major chest muscles involved in breathing and arm movement involved in breathing and arm movement Supports the structural integrity of the entire chest wall during daily activities Why does my sternum hurt? Sternum pain commonly results from costochondritis, muscle strain from exercise, or trauma. Persistent coughing, poor posture, and stress can also contribute to discomfort in this area. Can the sternum break easily? The sternum is relatively strong and doesn't break easily under normal circumstances. Fractures typically require significant trauma, such as car accidents or high-impact sports injuries, to occur. How long does a fractured sternum take to heal? Initial bone healing typically occurs within 6-8 weeks Complete recovery may take 3-6 months, depending on fracture severity and complications Simple fractures heal faster than complex injuries involving multiple structures Age, overall health, and adherence to treatment recommendations influence healing time What causes popping in the sternum? Sternum popping usually results from the movement of cartilage and joints between the ribs and the breastbone. Is sternum pain serious? Most sternum pain is benign, often caused by muscle strain or costochondritis. However, pain accompanied by shortness of breath, sweating, or radiating symptoms requires immediate medical evaluation. Can costochondritis cause sternum pain? Yes, costochondritis directly causes sternum pain by inflaming the cartilage connections between ribs and breastbone. Where is the sternum located? The sternum location is at the centre of your chest, running vertically from just below your collarbone to the upper abdomen, forming the front part of your rib cage. What organs does the sternum protect? The sternum protects your heart, lungs, major blood vessels, and part of the oesophagus. It forms a vital protective barrier for these essential organs within your chest cavity. Can exercise cause sternum pain? Yes, exercise can cause sternum pain from muscle strain, costochondritis, overuse, or poor technique. Activities such as heavy lifting, push-ups, or high-impact sports may irritate the chest muscles or rib joints and worsen pain with repeated movement.
What is an Osteophyte? Causes, Symptoms, and Treatment Options
What is an Osteophyte (Bone Spur)? An osteophyte is a smooth, bony outgrowth that develops along the edges of bones, particularly where bones meet at joints or along your spine. These bone spurs form gradually as Your body’s adaptive response to mechanical stress, pressure, or cartilage damage. The development of bone spurs often accompanies conditions like osteoarthritis, where cartilage breakdown triggers your body's repair mechanisms. Osteophytes typically appear as small, pointed projections on X-rays, resembling small bony ridges or spikes extending from the bone’s surface. Where do Osteophytes Commonly Occur? Spine (cervical, thoracic, lumbar): Along vertebral edges and around facet joints where spinal segments meet Knees: Around joint margins where the thighbone, shinbone, and kneecap connect, particularly with advancing osteoarthritis Hips: Along the rim of the hip socket, where the rounded femoral head meets the acetabulum Heels and feet: Especially on the underside of the heel bone, where the plantar fascia attaches, creating painful heel spurs Shoulders: Around the acromion and glenohumeral joint, often associated with rotator cuff problems Hands and fingers: Around the distal and proximal interphalangeal joints, forming characteristic Heberden’s and Bouchard’s nodes in osteoarthritis Other joints: Including elbows, wrists, and ankles, particularly following previous injuries or chronic stress What Causes Osteophytes to Form? • Osteoarthritis: The leading cause, where cartilage breakdown prompts compensatory bone growth at joint margins • Natural ageing and wear-and-tear: Chronic joint use and microscopic damage accumulate over time, stimulating bone formation • Tendonitis or ligament stress: Conditions like plantar fasciitis create chronic pulling forces that trigger bone spur development • Spinal disc degeneration: Loss of disc height and instability trigger compensatory osteophyte formation along vertebral margins • Previous injuries or trauma: Fractures, dislocations, or ligament tears can disrupt joint surfaces and promote abnormal bone growth • Inflammatory conditions: Certain types of arthritis or metabolic disorders can contribute to excessive bone formation How do Osteophytes Develop (Pathophysiology) The formation of an osteophyte involves a complex biological process called osteophytosis. When cartilage becomes damaged or joints become unstable, your body activates special bone-forming cells called osteoblasts. These cells produce new bone tissue as a repair mechanism, often aiming to stabilise affected joints by reinforcing bone margins. In spinal conditions, disc degeneration creates cracks and loss of height, which loosens surrounding ligaments. Your body responds by growing bone spurs to reinforce these weakened areas. Types of Osteophytes • Marginal osteophytes: Develop along joint surface edges as part of degenerative arthritis in knees, hips, and finger joints • Spinal osteophytes: Form on vertebral bodies, facet joints, or around nerve exit openings throughout the cervical, thoracic, and lumbar spine • Enthesophytes: Arise where soft tissues attach to bone, such as heel spurs at plantar fascia insertions • Acromial osteophytes: Develop on the shoulder blade's acromion process, often causing rotator cuff impingement • Hand joint osteophytes: Create characteristic bony enlargements at finger joints known as Heberden’s nodes (distal joints) and Bouchard’s nodes (proximal joints) • Hip rim osteophytes: Form along the hip socket edge or femoral neck in hip osteoarthritis and impingement syndromes Symptoms of Osteophytes • Joint pain or aching that typically worsens with activity • Stiffness and reduced range of motion in affected joints • Localised swelling or palpable bony prominences • Grinding, catching, or locking sensations during joint movement • Nerve-related symptoms, such as radiating pain, numbness, or tingling • Back or neck pain • Heel pain during standing or walking • Shoulder pain during overhead activities Asymptomatic Osteophytes: When You May Not Feel Anything Because bone spurs are typically smooth and may not interfere with surrounding tissues or joint function, they often go completely unnoticed throughout a person's lifetime. These asymptomatic osteophytes represent signs of underlying wear-and-tear or age-related changes rather than active sources of pain or dysfunction. Osteophytes in the Spine Spinal osteophytes form along vertebral edges and facet joints due to disc degeneration and chronic stress. They may narrow nerve openings (foraminal stenosis) or press on the spinal canal, causing pain, stiffness, and nerve-related symptoms such as radiating pain, numbness, tingling, or weakness in specific areas of the arms or legs. Osteophytes in the Knee Knee osteophytes form along joint margins where the thighbone, shinbone, and kneecap meet, most commonly developing in the setting of knee osteoarthritis. These bone spurs can cause knee pain, stiffness, and grinding sensations during movement, particularly when climbing stairs, squatting, or rising from seated positions. Osteophytes in the Hip Hip osteophytes typically develop along the acetabular rim or femoral neck as hip osteoarthritis progresses, creating characteristic changes visible on X-rays. These bone spurs can cause deep hip pain that may radiate to your groin, buttock, or thigh, often worsening with walking, climbing stairs, or prolonged sitting. Heel Spurs (Calcaneal Osteophyte) Heel spurs (calcaneal osteophytes) represent a specific type of bony outgrowth that forms on the underside of the heel bone where the plantar fascia attaches. This bone spur often develops alongside plantar fasciitis, creating sharp, stabbing heel pain that's typically worst with your first steps in the morning or after prolonged sitting. Osteophytes in Shoulders & Fingers Shoulder osteophytes commonly form on the acromion process, potentially impinging on the rotator cuff tendons and causing pain during overhead activities such as reaching, lifting, or throwing. Finger osteophytes create characteristic bony enlargements at joint margins, forming Heberden’s nodes at the distal interphalangeal joints and Bouchard’s nodes at the proximal interphalangeal joints. What Causes Osteophyte Pain? • Direct pressure on surrounding tissues, including muscles, tendons, ligaments, or joint capsules • Nerve compression (pinched nerve) causing radiating pain, numbness, or weakness • Joint space narrowing leading to increased friction between bone surfaces during movement • Inflammation in the surrounding soft tissues triggered by mechanical irritation from bone spurs • Mechanical impingement limiting normal joint motion and causing compensatory strain patterns • Muscle spasm develops as a protective response to joint dysfunction and pain How Osteophytes Are Diagnosed • Medical history and physical examination to evaluate symptoms and joint function • X-rays are the primary imaging method for visualising bone spurs and assessing joint space narrowing • MRI scans are used to evaluate soft tissue, cartilage, or nerve compression in complex cases • CT scans provide detailed imaging of bone anatomy, especially useful in evaluating spinal osteophytes • Blood tests such as the Rheumatoid Arthritis Profile, CRP (C-reactive protein), and synovial fluid analysis may be ordered to rule out inflammatory arthritis to rule out inflammatory arthritis or other systemic conditions • Nerve conduction studies are performed if pinched nerve symptoms suggest nerve compression or damage Treatment Options for Osteophytes • Rest and activity modification: Reducing stress on affected joints • Pain relievers: Non-steroidal anti-inflammatory drugs (NSAIDs) • Physical therapy: Strengthening exercises and mobility improvement • Corticosteroid injections: For significant inflammation and pain • Surgical intervention: Considered only when conservative treatments fail or when nerve compression causes significant neurological symptoms Non-Surgical Treatments for Bone Spurs • Medications to reduce pain, such as paracetamol and ibuprofen, according to the NHS • Physical therapy to improve joint mobility and strengthen supporting muscles • Activity modification to avoid movements that exacerbate symptoms • Heat and cold therapy for symptom management and inflammation control • Corticosteroid injections for targeted anti-inflammatory treatment • Weight management to reduce mechanical stress on weight-bearing joints • Supportive devices like braces, orthotics, or ergonomic aids to improve joint function Surgical Options for Osteophyte Removal Surgical options include minimally invasive arthroscopic removal in accessible joints like the knee or shoulder, open surgical procedures for complex cases, spinal decompression surgery when bone spurs cause significant nerve compression, and joint replacement for severe osteoarthritis with extensive osteophyte formation. Complications of Untreated Osteophytes • Progressive joint damage and accelerated osteoarthritis development • Chronic pain that becomes progressively harder to control with standard treatment • Permanent nerve damage if a pinched nerve remains compressed without treatment • Reduced mobility and functional decline affecting independence and quality of life • Muscle weakness and atrophy from compensatory movement patterns • Secondary problems in other joints due to altered movement mechanics Prevention Tips for Osteophytes • Maintain a healthy body weight to reduce mechanical stress on weight-bearing joints • Exercise regularly with low-impact activities to maintain joint mobility and muscle strength • Use proper body mechanics during lifting, carrying, and repetitive activities • Address injuries promptly to prevent long-term joint damage and instability • Manage underlying conditions like osteoporosis through appropriate medical treatment and lifestyle modifications • Wear appropriate footwear with good support and cushioning for daily activities • Take breaks during repetitive activities to allow joints to rest and recover When to See a Doctor for Osteophyte Symptoms? • Persistent joint pain lasting more than a few days without improvement • Progressive stiffness that interferes with daily activities or sleep • Numbness, tingling, or weakness suggesting possible nerve compression • Significant functional limitations affecting work, exercise, or personal care • Pain that worsens despite rest and over-the-counter pain management • Signs of inflammation, including joint swelling, warmth, or redness Conclusion Osteophytes represent your body's natural response to joint stress and wear, but they don't have to control your life. Understanding osteophyte causes, recognising symptoms early, and pursuing appropriate treatment can help you maintain an active, comfortable life. Early diagnosis through proper imaging and blood tests can identify underlying conditions like osteoporosis that contribute to joint problems. Conservative treatments often provide significant relief, while surgical options remain available for severe cases. At Metropolis Healthcare, we support your journey toward better joint health with comprehensive diagnostic services to identify and monitor conditions such as osteophytes. Our extensive network of over 220 laboratories and 4,600+ service centres ensures accessible, accurate testing when you need it most. With convenient home sample collection spanning 10,000+ touchpoints across India, you can access the diagnostic clarity needed to guide effective treatment decisions from the comfort of your home. FAQs What is an osteophyte? An osteophyte is a smooth bony growth on bone edges, often at joints, that forms from repair processes such as osteoarthritis; it is usually harmless but may cause pain. What causes bone spurs to develop? • Osteoarthritis and cartilage loss • Ageing and natural wear-and-tear • Joint instability from disc degeneration • Repetitive stress and overuse injuries Do osteophytes go away on their own? Osteophytes do not disappear naturally, as they are permanent bony growths, though symptoms may improve with proper treatment and management strategies. Are osteophytes serious? Most osteophytes are harmless and asymptomatic, but they become serious when they compress nerves, causing chronic pain or significantly limiting mobility and function. How do you treat osteophytes naturally? • Apply ice and heat therapy • Perform gentle stretching exercises • Maintain a healthy weight • Follow anti-inflammatory diet principles Can osteophytes cause nerve compression? Yes, osteophytes can compress nerves, particularly in the spine, causing numbness, tingling, weakness, and pain radiating to arms or legs. What is the difference between osteophytes and arthritis? Osteophytes are bony growths that often result from arthritis, while arthritis is the underlying inflammatory joint disease causing cartilage breakdown. Can exercise help osteophytes? Yes, appropriate exercise strengthens supporting muscles, maintains joint mobility, and can reduce symptoms, though it won't eliminate existing bone spurs. How are osteophytes diagnosed? Healthcare providers use X-rays as the primary diagnostic tool, supplemented by MRI or CT scans for detailed assessment of soft tissue. When should I worry about bone spurs? Seek medical attention for persistent or worsening joint pain, numbness, tingling, weakness, difficulty with daily activities, or symptoms unresponsive to conservative treatment.
What is a Bone Bruise? Causes, Symptoms, and Recovery Process
What is a Bone Bruise? A bone bruise represents a traumatic injury to the bone that is more severe than a soft tissue bruise but less severe than a complete fracture. Unlike surface bruises that affect only skin and soft tissues, a bone contusion involves damage to the inner trabecular (spongy) bone and bone marrow. This injury occurs when small blood vessels in the bone marrow rupture, causing bleeding and fluid accumulation within the bone. What makes bone bruise symptoms particularly challenging is that the pain often persists long after any visible skin discolouration fades. Bone marrow swelling and internal bleeding increase pressure within the rigid bone matrix, leading to the characteristic deep, aching pain that worsens with movement or pressure. How Does a Bone Bruise Differ from a Bone Fracture? Feature Bone Bruise Fracture Damage Type Microfractures and bleeding in bone marrow; bone remains intact Complete break in bone continuity X-ray Visibility Often invisible on standard X-rays Clearly visible crack or break Severity Less severe; allows some weight-bearing activities More severe; requires immobilisation Healing Time 1-3 months typically 6-12 weeks with proper care Treatment Conservative management with rest and pain relief May require casting, surgery, or immobilisation Types of Bone Bruises • Subperiosteal hematoma: This type occurs when blood accumulates under the periosteum, the outer membrane covering bones. Direct, high-force trauma typically causes this injury, such as being struck by a cricket bat or falling onto a hard surface. • Intraosseous bruise: This involves bleeding and swelling within the bone marrow cavity itself. Repetitive compressive forces, like those experienced by runners or basketball players, commonly cause this type of bone contusion. • Subchondral lesion: This type affects the area just beneath the joint cartilage. Compressive or twisting forces that separate cartilage from the underlying bone cause these injuries, often seen in knee and ankle injuries. Common Areas Where Bone Bruises Occur • Knees: The most common site for bone contusions in athletes, particularly those involved in contact sports or activities requiring sudden direction changes • Ankles: Ankle bone bruise injuries frequently occur during sprains, falls, or awkward landings from jumps • Hips and pelvis: Often result from falls, especially in older adults, or high-impact collisions in sports • Wrists and forearms: Common after falls onto outstretched hands (FOOSH injuries) • Shins and lower legs: Frequently affected by direct blows or repetitive impact activities • Shoulder and upper arm: May occur during contact sports or falls onto the shoulder Symptoms of a Bone Bruise • Deep, aching pain: The hallmark symptom that feels different from muscle or skin pain, often described as coming from within the bone itself • Persistent tenderness: Pain that worsens when pressure is applied to the affected area; even light touch can be uncomfortable • Localised swelling: Inflammation in the area that may extend to surrounding soft tissues • Skin discolouration: While not always present, some people notice colour changes similar to surface bruising • Joint stiffness: When near joints, bone bruises can significantly limit the range of motion and cause inflammation • Hard lump formation: Occasionally, a firm area may develop beneath the skin at the injury site due to localized swelling or fibrosis • Pain that worsens with activity: Unlike improving with movement, bone bruise pain typically increases with weight-bearing or use Causes of Bone Bruises • Direct impact trauma: Falls, sports collisions, car accidents, or being struck by objects can cause immediate bone contusions • Twisting or rotational forces: Sudden direction changes that pull ligaments and cartilage away from bone, common in sports like football or basketball • Repetitive stress: Ongoing pressure from activities like running on hard surfaces or jumping can gradually damage bone tissue • Bone-on-bone contact: Occurs when adjacent bones impact during joint movement, especially in unstable or arthritic joints • Degenerative conditions: Arthritis can lead to bone bruises as protective cartilage wears away, allowing bones to grind against each other • Inadequate recovery: Returning to activity too soon after an injury can convert minor damage into a full bone contusion Risk Factors for Bone Bruising • High-impact sports participation: Football, basketball, rugby, and skiing carry elevated risks due to their physical nature • Frequent running or jumping: Activities that repeatedly stress bones, especially on hard surfaces like concrete • Pre-existing arthritis: Joint degeneration increases vulnerability to bone bruises as protective cartilage diminishes • Previous injuries: Areas with prior trauma may be more susceptible to bone contusions • Age-related changes: Older adults face higher risks due to decreased bone density and slower healing • Inadequate protective equipment: Failing to use appropriate padding or safety gear during sports activities • Poor conditioning: Insufficient muscle strength and flexibility can increase injury risk during physical activities • Certain medical conditions: Bleeding disorders or conditions affecting bone health may predispose individuals to bone bruises Complications of Bone Bruises • Chronic pain syndrome: Persistent discomfort lasting months beyond the expected healing time • Joint stiffness and reduced mobility: Prolonged inflammation can lead to permanent movement limitations • Secondary arthritis development: Particularly with subchondral bone bruises, where cartilage damage increases arthritis risk • Progression to stress fracture: Continued stress on a healing bone contusion can lead to complete fractures • Functional impairment: Ongoing pain and stiffness may prevent return to previous activity levels • Psychological impact: Chronic pain can affect mental health and quality of life How are Bone Bruises Diagnosed? Diagnosing a bone contusion requires a comprehensive approach, as these injuries often don't appear on standard X-rays: • Detailed medical history: Your doctor will ask about the injury mechanism, symptom onset, and pain characteristics • Physical examination: Assessment of tenderness, swelling, range of motion, and functional limitations • Symptom evaluation: Discussion of pain patterns, activities that worsen symptoms, and impact on daily life • Ruling out other conditions: Ensuring no fractures, ligament tears, or other injuries are present • Response to initial treatment: Monitoring how symptoms change with rest and basic interventions Tests for Bone Bruises • MRI scan: The gold standard for diagnosing bone bruises, as it clearly shows bone marrow oedema and internal bleeding that other tests miss • X-ray imaging: While bone bruises typically don't show on X-rays, these tests help rule out fractures and other bone injuries • CT scans: Occasionally used when an MRI isn't available or when detailed bone structure assessment is needed • Ultrasound: May help assess soft tissue involvement and swelling around the injury site Treatment Options for Bone Bruises Effective bone bruise treatment focuses on managing pain, reducing inflammation, and supporting natural healing: • RICE protocol implementation: Rest, ice application, compression, and elevation help control initial swelling and pain • Pain management medications: Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen help reduce both pain and inflammation • Activity modification: Avoiding aggravating activities while maintaining gentle movement to prevent stiffness • Physical therapy: Once acute pain subsides, guided exercises help restore strength and mobility • Weight-bearing restrictions: Using crutches or supportive devices to reduce stress on healing bone tissue • Heat therapy: Applied after initial inflammation subsides, heat can improve circulation and reduce stiffness • Gradual return to activity: Slowly increasing activity levels as symptoms improve and healing progresses Bone Bruise Recovery Time: What to Expect Most bone bruises heal within 1-3 months, though this can vary considerably based on the injury's severity and location. During the first 1-2 weeks, you'll likely experience the most intense pain and swelling. This acute phase requires careful management with rest, ice, and pain medication as needed. Weeks 2–6 typically show gradual improvement in pain, swelling, and joint function. You might notice that daily activities become more manageable, though intense or high-impact activities may still cause discomfort. This is when physical therapy often begins, focusing on gentle range-of-motion and strengthening exercises. The final phase, spanning weeks 6-12, involves continued healing of the bone marrow and return to normal activities. Most mild bone bruises resolve by 6–8 weeks, while others may need the whole 3 months for complete healing. Factors affecting healing time include age, overall health, injury severity, and adherence to treatment recommendations. Severe Bone Bruises & When Surgery Is Needed Surgery may be required for extensive bone marrow injury, significant cartilage damage, or associated ligament tears compromising joint stability, or when associated ligament tears compromise joint stability. Arthroscopic surgery may be recommended for severe subchondral bone bruises, particularly in the knee, where damaged cartilage and bone tissue can be addressed directly. This minimally invasive approach allows surgeons to remove damaged tissue and stimulate healing through techniques like microfracture repair. Surgery might also be considered if conservative bone bruise treatment fails after 3 months or if the injury shows signs of progressing to a complete fracture. The decision for surgery involves careful consideration of the injury's impact on your quality of life, activity goals, and response to non-surgical treatments. Bone Bruise in Children vs Adults Children and adults experience bone bruises differently, with several essential distinctions in presentation and healing. Children typically heal faster than adults because of richer bone blood supply and active bone remodelling. A bone contusion that might take 3 months to heal in an adult could resolve in 6-8 weeks in a child. However, children face unique challenges with bone bruises. They may struggle to articulate the deep, aching pain characteristic of these injuries, sometimes leading to delayed diagnosis. Additionally, bone bruise symptoms in children can mimic growth plate issues, making careful evaluation essential. Early recognition and appropriate treatment help ensure complete healing and prevent long-term complications. Do Bone Bruises Lead to Arthritis? The relationship between bone bruises and the development of arthritis is a significant concern, particularly for subchondral bone contusions. Research suggests that severe or recurrent bone bruises may increase the long-term risk of developing osteoarthritis. When a bone contusion damages the subchondral bone layer that supports joint cartilage, it can alter the normal mechanical stress distribution across the joint surface. This disruption may lead to accelerated cartilage breakdown and eventual development of arthritis. According to a study published in the American Journal of Roentgenology, knee bone bruises that are left untreated or inadequately managed may contribute to the earlier development of osteoarthritis. The risk is greatest when bruises affect weight-bearing joint surfaces or when multiple sites are injured simultaneously. However, proper treatment and rehabilitation for a bone bruise can significantly reduce the risk of arthritis. How to Prevent Bone Bruises • Use appropriate protective equipment: Wear proper padding, helmets, and guards during sports activities • Maintain proper conditioning: Strong muscles and good flexibility help protect bones during physical activities • Practice proper techniques: Learn correct form for sports and exercise activities to reduce injury risk • Choose appropriate footwear: Use shoes with adequate cushioning and support for your activities • Gradually increase activity intensity: Avoid sudden increases in training volume or intensity • Strengthen supporting muscles: Focus on building strength around vulnerable joints like knees and ankles • Address underlying conditions: Manage arthritis and other conditions that increase bone bruise risk • Create safe environments: Remove hazards that could cause falls or impacts in your home and workspace When to See a Doctor? • Severe pain that doesn't improve with rest and basic pain management • Inability to bear weight on the affected limb • Visible deformity or suspected fracture • Signs of infection such as fever, increasing redness, or warmth • Numbness or tingling suggesting nerve involvement • Persistent pain lasting more than a few days without improvement • Swelling that doesn't respond to rest and elevation • Limited range of motion or joint stiffness Conclusion Understanding bone bruises empowers you to recognise symptoms, seek appropriate care, and actively participate in your recovery process. These injuries, whilst often overlooked compared to fractures, require proper attention and management to prevent complications and ensure optimal healing. The distinction between a bone bruise and a fracture emphasises why proper diagnosis via MRI becomes crucial when X-rays appear normal, but pain persists. Bone bruise treatment focuses on conservative management, with surgery reserved for severe cases involving associated structural damage. Prevention through protective equipment, physical conditioning, and safe activity practices significantly reduces injury risk. When bone bruises do occur, early recognition and appropriate medical care help prevent complications such as prolonged pain or the development of arthritis. At Metropolis Healthcare, we support your health journey through comprehensive diagnostic services that help identify and monitor bone and joint injuries. With over 4,000 advanced tests and profiles available through our network of 220+ laboratories, we provide the precise diagnostic tools your doctor needs for accurate assessment. FAQs How long does a bone bruise take to heal? • Mild bone bruises: 2-6 weeks for initial improvement • Moderate contusions: 6-12 weeks for significant recovery • Severe subchondral bruises: 3-6 months or longer for complete healing • Healing time depends on age, injury location, associated injuries, and overall health status What does a bone bruise feel like? A bone bruise typically causes deep, aching pain that worsens with movement or weight-bearing, often accompanied by swelling and tenderness. Is a bone bruise serious? Whilst not as severe as fractures, bone bruises can be serious, potentially leading to prolonged pain and complications if not adequately treated. Can you walk with a bone bruise? Walking ability depends on location and severity; some bone bruises allow limited walking, whilst others require crutches or complete rest. Do bone bruises show up on an X-ray? No, bone bruises don't appear on standard X-rays because they involve internal bone marrow damage rather than structural breaks visible on conventional imaging. Can a bone bruise turn into a fracture? Bone bruises rarely progress to fractures; however, severe trauma may cause associated microfractures that require monitoring. What is the best treatment for a bone bruise? • Rest and activity modification to allow healing • Ice application and elevation to reduce swelling • Pain management with appropriate medications • Gradual return to activity through physical therapy • Protection through bracing when necessary How do you know if a bone bruise is getting worse? • Increasing pain intensity despite rest and treatment • Progressive swelling or new areas of tenderness • Decreased ability to bear weight or move the joint • Development of fever or signs of infection • Persistent symptoms beyond expected healing timeframes Can a bone bruise cause swelling? Yes, bone bruises commonly cause swelling due to fluid accumulation and inflammation within the bone and surrounding tissues. Does heat help a bone bruise? Heat therapy may help after the initial acute phase (48-72 hours), but ice is preferred initially to reduce inflammation and pain effectively.
What is a Dental Bone Graft? Procedure, Benefits, and Recovery
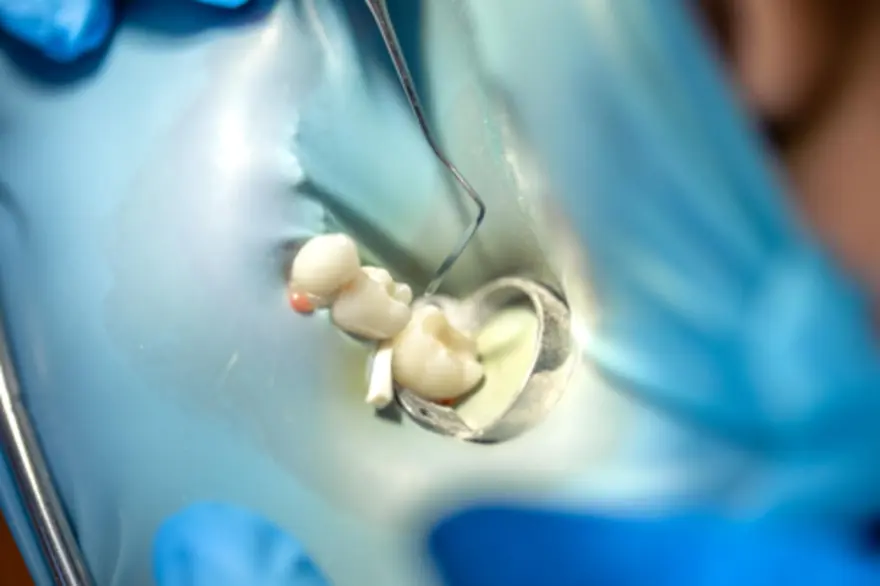
What Is a Dental Bone Graft? A dental bone graft involves placing bone or bone-like material into areas of your jaw where natural bone has been lost or is too thin to support dental implants or restorations. During this procedure, your dentist or oral surgeon adds bone graft material that stimulates your body to regenerate new, healthy bone tissue over time. The dental bone graft procedure works through a natural process called bone remodelling, where your body gradually replaces the graft material with your own living bone tissue. This treatment is commonly used to prepare sites for dental implants, restore bone lost after tooth extraction, or repair bone damage caused by periodontal (gum) disease. Why Is a Dental Bone Graft Needed? • Preparing for dental implants when the jawbone lacks sufficient thickness or density • Restoring bone lost after tooth extraction or long-term tooth absence • Treating bone loss from advanced gum disease that has destroyed the surrounding bone • Repairing bone defects from trauma, injury, or cyst removal • Supporting loose teeth by rebuilding bone around them • Preserving the socket after tooth removal through socket preservation techniques • Preparing the upper jaw for sinus lift procedures when planning back upper implants • Improving denture fit by increasing jawbone height or width • Maintaining facial shape and preventing a sunken appearance from bone loss How Does Bone Loss Occur in the Jaw? Your jawbone stays strong when regularly stimulated by chewing forces transmitted through your teeth or dental implants. When teeth are missing, this stimulation decreases, and the bone begins to shrink through a process called disuse atrophy, where lack of stimulation leads to gradual bone resorption. After tooth removal, the surrounding bone can narrow and shorten rapidly in the first few months. Bone loss may continue for years, particularly under removable dentures. Advanced gum disease also destroys bone around teeth through chronic inflammation, whilst trauma, infection, or cysts can remove sections of bone entirely, leaving defects that weaken the jaw and affect chewing, speech, and facial appearance. Types of Dental Bone Grafts • Socket preservation graft: Placed immediately after tooth extraction to maintain bone volume for future implants • Ridge augmentation graft: Rebuilds width or height in areas where bone has already shrunk significantly • Sinus lift procedure: Adds bone material in the upper jaw when the sinus cavity limits implant placement • Periodontal grafts: Target bone defects around existing teeth caused by gum disease • Block bone grafts: Use larger pieces of bone secured with screws for major reconstruction • Guided tissue regeneration: Combines grafts with barrier membranes to direct bone growth What Materials are Used in Dental Bone Grafts? • Autograft: Your own bone from the chin, jaw, or hip; considered the gold standard • Allograft: Processed, sterilized donor bone obtained from accredited human tissue banks • Xenograft: Highly processed animal bone that acts as a scaffold • Alloplast: Synthetic materials like calcium phosphate or hydroxyapatite • Enhanced grafts: Combined with platelet-rich fibrin (PRF) or bioactive growth factors to accelerate bone regeneration When Do You Need a Dental Bone Graft? • Planning a dental implant with insufficient bone height, width, or density • Having a long-missing tooth with a thin or collapsed ridge • Experiencing advanced gum disease with bone loss around teeth • Requiring socket preservation at extraction time • Needing implants in the upper back jaw near the sinus • Wearing loose or ill-fitting dentures caused by jawbone shrinkage (ridge resorption) • Having bone defects from infection, cysts, or injury • Experiencing facial changes from long-term tooth and bone loss How Does a Dental Bone Graft Procedure Work? Comprehensive evaluation, including medical history review and detailed imaging to assess bone volume Treatment planning to determine the appropriate dental bone graft types and materials for your needs Administration of local anesthesia and, if needed, sedation to ensure comfort during surgery Site preparation is done by gently opening the gum tissue and cleaning the area of any damaged tissue Graft placement where bone material is carefully positioned and secured in the treatment area Placement of a barrier membrane may be required to protect the graft and guide proper bone regeneration Tissue closure with sutures to cover and protect the grafted area during initial healing Recovery monitoring with follow-up visits to track healing progress and integration How Long Does a Dental Bone Graft Take to Heal? The healing time for dental bone grafts varies significantly depending on the size and complexity of your procedure. Initial soft tissue (gum) healing usually occurs within one to two weeks, but the grafted bone requires much longer to integrate with your existing bone structure fully. Most dental bone grafts require at least three months for initial bone integration. In comparison, larger or more complex grafts may require six to twelve months before the area is ready for implant placement or other restorative work. Recovery After Dental Bone Graft • Take prescribed medications exactly as directed for pain control and infection prevention • Apply ice packs for the first 24-48 hours to reduce swelling and discomfort • Rest adequately and avoid strenuous physical activities for at least 3–5 days after surgery • Maintain gentle oral hygiene without disturbing the surgical site • Attend all follow-up appointments for professional monitoring of healing progress • Watch for warning signs like severe pain, excessive bleeding, or signs of infection What to Expect in the First Week • Mild to moderate discomfort that improves daily with pain medication • Some swelling and bruising that peaks around day three • Minor bleeding or oozing for the first 24 hours • Difficulty chewing hard or crunchy foods • Temporary dietary restrictions to protect the healing site Foods to Eat and Avoid After a Bone Graft Foods to eat: • Soft foods like yoghurt, smoothies, and mashed potatoes • Protein-rich options such as eggs, fish, tofu, and tender chicken • Nutritious soups and broths • Cooked vegetables and soft fruits Foods to avoid: • Hard, crunchy, or sticky foods • Spicy or acidic foods that may irritate • Very hot foods and beverages • Small seeds or nuts that could get trapped Dental Bone Graft Success Rate Research shows that dental bone graft procedures have excellent success rates, with studies reporting success rates between 85-95% when performed by experienced oral surgeons. The success of your dental bone graft depends on several factors, including the type of graft material used, the size and location of the defect, and your overall health status. Socket preservation procedures usually show the highest success rates, while larger reconstruction grafts may have slightly lower but still very favourable outcomes. Risks & Complications of Dental Bone Grafts • Infection at the graft site requiring antibiotic treatment • Graft failure where the material doesn't integrate properly • Temporary or, rarely, permanent numbness due to nerve irritation or injury • Sinus complications during upper jaw procedures • Excessive bleeding or swelling beyond expected healing levels • Allergic reactions to graft materials (extremely rare) How Painful is a Dental Bone Graft? Most patients report mild to moderate discomfort rather than severe pain after a dental bone graft. Your oral surgeon will prescribe appropriate pain medication to keep you comfortable during the healing process. The discomfort typically peaks within the first 48-72 hours and gradually decreases. Proper pain management and adherence to post-operative instructions help ensure a more comfortable recovery. Factors That Affect Bone Graft Success • Overall health status and any underlying medical conditions that affect healing • Smoking significantly reduces blood flow and impairs bone formation, according to NHS guidance • Age and bone quality, as younger patients typically heal faster • Oral hygiene practices both before and after the procedure • Compliance with post-operative instructions, including medication use and activity restrictions • Graft material selection and surgical technique used by your doctor Can You Get a Dental Implant Without a Bone Graft? The need for a dental bone graft before implant placement depends on your specific bone volume and density. The oral surgeon will use detailed imaging to measure your bone dimensions and determine whether additional bone is needed. In some cases, smaller grafts can be placed at the same time as implant surgery, while larger defects require separate grafting procedures with a healing time before implant placement. When to See a Dentist or Oral Surgeon? • Severe pain that doesn't improve with prescribed medication • Signs of infection such as fever, excessive swelling, or pus • Persistent bleeding beyond the first 24 hours • Numbness or tingling that doesn't resolve • Exposure of graft material through the gum tissue Conclusion Understanding the benefits, procedures, and recovery of dental bone grafts helps you make confident decisions about your oral health. Whether you need socket preservation after tooth extraction, a sinus lift for upper implants, or ridge augmentation for denture support, modern bone grafting techniques offer predictable results with excellent success rates. The healing time for dental bone grafts varies, but most patients find that the investment in a stronger jawbone structure significantly improves their quality of life. Consistent post-operative care and patience during healing maximise the long-term benefits of your dental bone graft and lay the foundation for successful long-term outcomes. At Metropolis Healthcare, we support your health journey with comprehensive diagnostic services that help monitor your overall wellness. Our extensive network of over 4,000 tests and profiles includes specialised assessments that can evaluate your healing progress and overall health status. With convenient home sample collection services spanning 10,000+ touchpoints across India, we make healthcare accessible when you need it most. FAQs How long does a dental bone graft take to heal? • Soft tissue healing: 1-2 weeks for gum healing • Initial bone integration: 3-4 months for basic healing • Complete maturation: 6-12 months for full bone formation • Implant readiness: 3-9 months, depending on graft complexity Is a dental bone graft painful? Most patients report mild to moderate discomfort rather than severe pain. Prescribed pain medication effectively manages any discomfort during the initial healing period. What is the success rate of a bone graft for teeth? Dental bone grafts show success rates of 85–95% when performed by experienced oral surgeons and accompanied by good aftercare and with proper post-operative care. Can a dental bone graft fail? Yes, though rare, bone grafts can fail due to infection, poor healing, smoking, or inadequate post-operative care compliance. How do I know if my dental bone graft is healing? • Decreasing pain and swelling over the first week • No signs of infection such as fever or excessive discharge • Stable graft material without exposure through the gums • Normal tissue colour returning to the surgical site Can you eat normally after a bone graft? You'll need to follow a soft food diet initially, gradually returning to normal eating as healing progresses over several weeks. How long after a bone graft can you get an implant? Most patients can receive implants 3-6 months after bone grafting, depending on graft size and individual healing rates assessed through imaging. Do bone grafts dissolve? Some graft materials gradually dissolve as your natural bone grows, while others provide permanent scaffolding that integrates with your existing bone structure. What happens if a bone graft doesn't take? Failed grafts may require removal and replacement, with your surgeon determining the best approach based on the specific cause of failure. Is a dental bone graft safe? Yes, dental bone grafts are considered very safe procedures with low complication rates when performed by qualified oral surgeons.
What is the Tailbone? Causes of Pain, Injury, and Treatment
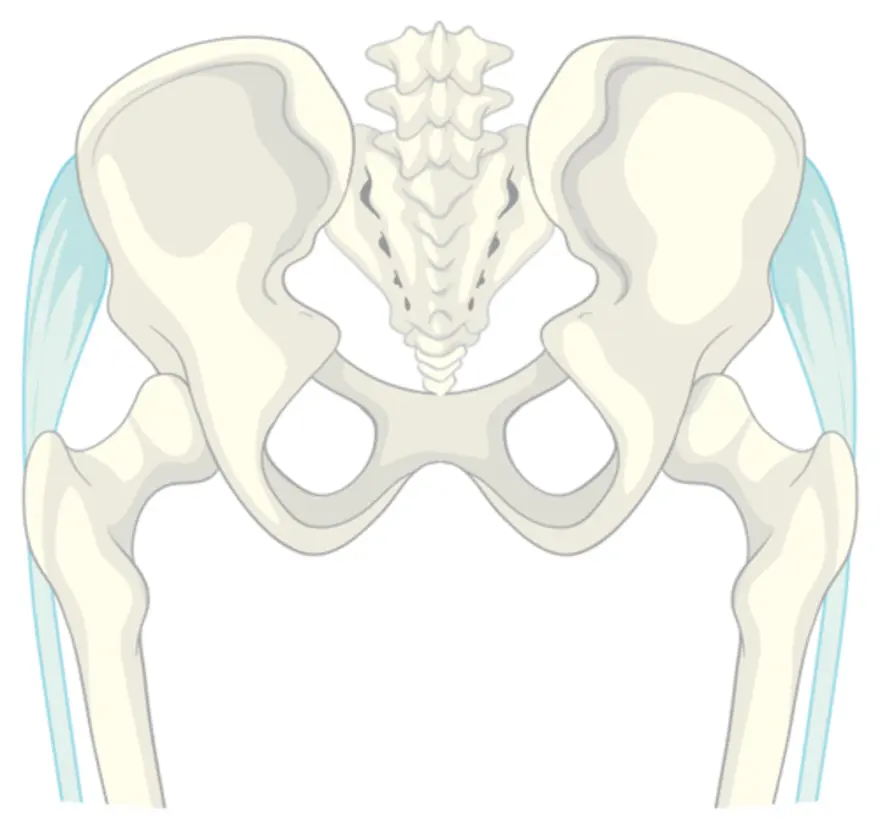
What Is the Coccyx (Tailbone)? The coccyx is the final segment of your spine, positioned at the base of the vertebral column below the sacrum. According to MedlinePlus, it consists of two to four tiny, partially fused vertebrae and is commonly called the tailbone. The coccyx is about 4–10 centimetres long and curves slightly forward toward the pelvis. This positioning allows the coccyx bone to work alongside other pelvic structures to support your body weight when sitting. Where Is the Coccyx Located? Your coccyx sits at the very bottom of your spine, forming the lowest part of your vertebral column. Located directly behind your rectum and above your anus, the tailbone occupies a critical position within your pelvic structure. When sitting and leaning slightly backward, your coccyx helps form a tripod of support with the two sitting bones (ischial tuberosities). Coccyx Anatomy: Structure & Segments • Shape and structure: A small, triangular bone measuring 4–10 cm in adults • Vertebral segments: Composed of 3-5 coccygeal vertebrae, with four segments being most common • Fusion pattern: These segments may be partially or completely fused, varying between individuals • Base connection: The upper portion articulates with the sacrum through the sacrococcygeal joint • Apex termination: The pointed lower end curves forward and provides muscle attachment points • Surface features: The front surface is slightly concave, whilst the back surface appears convex with small tubercles Functions of the Coccyx • Weight distribution: Helps bear body weight when sitting, forming a stable base with your pelvic bones • Muscle attachment: Anchors pelvic floor muscles, including the levator ani and coccygeus muscles • Sphincter support: Provides attachment points for ligaments supporting the external anal sphincter • Pelvic stability: Serves as an anchor for sacrotuberous and sacrospinous ligaments • Postural support: Contributes to spinal alignment and balance during position changes • Anatomical completion: Forms the terminal end of your vertebral column Common Coccyx (Tailbone) Problems • Coccydynia: A general term for tailbone pain that typically worsens when sitting or rising from a seated position • Contusion: Soft tissue bruising around the coccyx from direct trauma or falls • Fracture: A break in one or more coccygeal segments, usually caused by direct trauma such as a fall • Dislocation: Abnormal movement at the sacrococcygeal joint following trauma • Degenerative changes: Wear-and-tear or arthritic changes affecting joint function • Bony abnormalities: Excessive curvature or bone spurs irritating surrounding tissues • Infections: Rare cases of osteomyelitis or soft tissue infections near the tailbone • Tumours: Uncommon primary or metastatic growths affecting the coccygeal region Risk Factors for Coccyx Pain • Direct trauma: Falls onto buttocks, sports injuries, or motor vehicle accidents • Childbirth complications: Difficult vaginal deliveries or instrumental deliveries • Gender factors: Women experience coccydynia more frequently than men • Weight extremes: Both obesity and being significantly underweight increase risk • Prolonged sitting: Especially on hard or poorly cushioned surfaces • Anatomical variations: Unusual coccyx shape or positioning • Degenerative conditions: Osteoarthritis affecting the sacrococcygeal joint • Repetitive activities: Cycling, rowing, or horseback riding • Previous surgery: Spinal or pelvic procedures altering normal biomechanics How are Coccyx Injuries Diagnosed? • Medical history: Detailed discussion of symptom onset, trauma history, and aggravating factors • Physical examination: Palpation of the coccyx area and assessment of surrounding structures • Movement testing: Evaluation of pain with sitting, standing, and position changes • Neurological assessment: Evaluating for nerve irritation, referred pain, or lower spinal involvement • Imaging studies: X-rays, CT scans, or MRI when indicated • Specialised tests: Dynamic imaging during sitting or standing positions Test for Tailbone Injuries X-rays: Standard imaging to detect fractures, dislocations, or bony abnormalities CT scans: Detailed bone imaging for complex fractures or structural problems MRI scans: Soft tissue evaluation including ligaments, muscles, and surrounding structures Dynamic X-rays: Taken in sitting and standing positions to evaluate coccyx movement Bone scans: Nuclear medicine studies to detect infections or tumours Complete Blood Count (CBC): Detects infection or anaemia C-reactive protein (CRP) and Erythrocyte Sedimentation Rate (ESR): Indicators of inflammation or infection How Long Does Coccyx Pain Last? The duration of tailbone pain varies significantly depending on the underlying cause and treatment approach. Acute injuries usually heal within 4–6 weeks, whereas chronic coccydynia may persist for months or even years without appropriate treatment. Factors affecting recovery time include the severity of the initial injury, your age and overall health, adherence to treatment recommendations, and the development of complications. Early intervention with appropriate treatment for tailbone pain typically leads to faster recovery and better long-term outcomes. When Is Surgery Needed for Coccyx Problems? Surgical intervention for coccyx problems is rarely necessary and typically considered only after conservative treatments have failed. Coccygectomy, the surgical removal of the tailbone, may be recommended for severe, persistent pain that significantly impacts quality of life despite months of appropriate treatment. Candidates for surgery usually have documented structural abnormalities, failed conservative management for at least six months, and significant functional impairment. The surgery carries risks such as infection, nerve injury, and persistent pain, so careful patient selection is essential. Complications of Untreated Coccyx Pain • Chronic pain syndrome: Long-term discomfort affecting daily activities and sleep • Postural problems: Compensatory sitting and standing positions causing secondary issues • Muscle dysfunction: Weakness or spasm in pelvic floor muscles • Psychological impact: Depression, anxiety, or reduced quality of life • Social limitations: Avoidance of activities involving sitting or movement • Work disability: Difficulty performing job duties requiring prolonged sitting When to See a Doctor for Tailbone Pain? • Severe pain: Intense discomfort that interferes with daily activities • Persistent symptoms: Pain lasting more than a few weeks despite home treatment • Trauma history: Recent fall or injury to the tailbone area • Neurological symptoms: Numbness, tingling, or weakness in legs or feet • Bowel or bladder changes: New difficulty with urination, constipation, or incontinence • Signs of infection: Fever, redness, or swelling around the tailbone • Progressive worsening: Symptoms that continue to deteriorate over time Conclusion Understanding your coccyx and recognising the signs of tailbone problems empowers you to seek appropriate care when needed. Whether you're dealing with an acute tailbone injury or chronic coccydynia, effective treatment options are available to restore your comfort and mobility. Successful management depends on accurate diagnosis, tailored treatment, and patient understanding of coccyx anatomy and care. Most people with tailbone pain experience significant improvement with conservative measures, though some cases may require more specialised interventions. At Metropolis Healthcare, we understand the importance of accurate diagnosis in effectively managing tailbone pain. Our comprehensive portfolio of more than 4,000 tests includes advanced imaging and laboratory studies that help identify the underlying causes of your symptoms. With our extensive network of over 220 laboratories and 10,000+ touchpoints across India, we bring reliable diagnostic services directly to your doorstep through convenient home sample collection. FAQs What is the primary function of the coccyx? • Supports body weight when sitting by forming a tripod with the sitting bones • Anchors pelvic floor muscles that control bowel and bladder function • Provides attachment points for ligaments, maintaining pelvic stability • Contributes to overall spinal alignment and postural support Why does my tailbone hurt when I sit? Sitting places direct pressure on your coccyx, which can aggravate inflamed tissues, muscle tension, or structural abnormalities in the tailbone area. How long does coccyx pain take to heal? Most acute tailbone pain resolves within 4-8 weeks with proper treatment, though chronic cases may take months. Can the coccyx break easily? The coccyx can fracture from significant trauma, such as hard falls, but it's relatively well-protected by surrounding soft tissues. How do I relieve coccyx pain quickly? • Use cushioned seating or doughnut pillows to reduce pressure • Apply ice packs for 15-20 minutes several times daily • Take anti-inflammatory medications as directed by your doctor • Avoid prolonged sitting and take frequent standing breaks • Practice gentle stretching exercises for the surrounding muscles What causes tailbone pain without injury? Prolonged sitting, pregnancy, childbirth, degenerative changes, infections, or referred pain from other pelvic structures can cause tailbone discomfort. Is walking good for tailbone pain? Gentle walking often helps tailbone pain by promoting blood flow and preventing stiffness, but avoid activities that worsen symptoms. How do I know if my coccyx is dislocated? Severe pain, visible deformity, inability to sit comfortably, and pain with bowel movements may indicate coccyx dislocation requiring medical evaluation. Can tailbone pain be serious? Whilst usually benign, persistent tailbone pain may indicate fractures, infections, or other serious conditions requiring medical assessment and treatment. Which cushion is best for tailbone pain? Doughnut-shaped or wedge cushions with coccyx cutouts work best by reducing direct pressure on the tailbone while maintaining support.
What You Need To Know About Kidney Donation: Process, Risks, And Benefits
What Is Kidney Donation? Kidney donation involves the surgical removal of a healthy kidney from one person for transplantation into another whose kidneys have failed. Your kidneys filter waste products and excess fluid from your blood, producing urine. When kidneys stop working properly due to chronic kidney disease or acute kidney failure, patients need either lifelong dialysis or a kidney transplant surgery to survive. The human body can function normally with just one healthy kidney, which makes living kidney donation possible. A single donated kidney can restore normal kidney function in the recipient, often providing better outcomes than dialysis. The kidney donor typically experiences no long-term health complications, as the remaining kidney adapts to handle the full workload. This remarkable procedure offers hope to thousands of patients suffering from end-stage kidney disease. The donated organ begins filtering the recipient's blood immediately after successful transplantation, often dramatically improving their quality of life and extending their survival. Types of Kidney Donation • Living kidney donation: A healthy person undergoes surgery to donate one kidney. • Deceased kidney donation: Kidneys recovered from individuals who have died and consented to organ donation. • Kidney paired donation (kidney swap): Compatible exchanges between incompatible donor-recipient pairs. • Non-directed altruistic living donation: Generous individuals donate to unknown recipients, often triggering donation chains. Living Kidney Donation Living kidney donation involves a healthy individual voluntarily undergoing surgery to remove one kidney for transplantation into a person with kidney failure. These transplants can be scheduled at medically optimal times, reducing the recipient's time on dialysis waiting lists. Living donor kidneys typically begin functioning immediately after kidney transplant surgery, providing recipients with better long-term outcomes and improved quality of life. Most kidney donors return to normal activities within weeks of surgery and can live completely normal lives with one functioning kidney. Deceased Kidney Donation Deceased kidney donation occurs when kidneys are recovered from individuals who have died and are either registered as organ donors or whose families consent to donation. These kidneys are carefully matched and allocated to people with kidney failure according to medical urgency, compatibility factors, and established allocation policies. While deceased donor kidneys are life-saving, they may require more time to begin functioning after transplant compared to living donor transplants. Kidney Paired Donation (Swap Transplant) Kidney paired donation, commonly called a "kidney swap", provides options when willing living donors are incompatible with their intended recipients due to blood type or tissue matching issues. This innovative kidney donation process involves two or more donor-recipient pairs who exchange kidneys, allowing all compatible transplants to proceed successfully. Why Kidney Donation Is Needed Chronic kidney disease affects millions of people worldwide, with diabetes and high blood pressure being the leading causes. When kidneys fail completely, patients face limited treatment options: lifelong dialysis or kidney transplant surgery. Dialysis, while life-sustaining, significantly impacts quality of life and carries ongoing health risks. The demand for donor kidneys far exceeds the available supply. In India, the kidney donation rate lags significantly behind countries with established organ donation programs. Cultural factors, lack of awareness, and inadequate infrastructure contribute to this shortage. Eligibility Criteria for Kidney Donation • Age requirements: Typically 18–65 years, with some centres accepting carefully selected older adults. • Excellent overall health: Good physical and mental health with normal kidney function. • Adequate kidney function: Normal estimated glomerular filtration rate (eGFR) and healthy urine studies. • Blood pressure control: Normal or well-controlled blood pressure and no evidence of kidney damage. • Healthy body weight: No severe obesity; some centres require weight loss before donation. • No diabetes: Absence of diabetes or high-risk pre-diabetes in younger donors. • Cardiovascular health: No significant heart disease, previous heart attacks, or heart failure. • Cancer-free status: No active cancer or recent high-risk cancer history. • Mental health stability: No untreated psychiatric disorders, substance misuse, or addiction. • Voluntary consent: Informed and pressure-free decision verified by an independent donor advocate. • Compatible matching: Appropriate blood type and tissue compatibility, or willingness to participate in paired donation. Medical Conditions That Disqualify Donation • Uncontrolled high blood pressure that has already caused kidney damage. • Diabetes mellitus (Type 1 or Type 2) in most donor candidates. • Significant chronic kidney disease with low eGFR or abnormal urine protein. • Recurrent kidney stones with high risk of recurrence or structural abnormalities. • Cardiovascular disease, including coronary artery disease or serious arrhythmias. • Active malignancy or recent high-risk cancer requiring ongoing treatment. • Psychiatric illness that impairs decision-making capacity or treatment compliance. • Genetic kidney diseases, such as polycystic kidney disease or a strong family history of inherited kidney disease. • Uncontrolled infections, including certain chronic viral infections, depending on recipient risk. Benefits of Kidney Donation For Recipients: • Improved survival and quality of life compared to remaining on dialysis. • Reduced dialysis dependence, with many avoiding dialysis entirely. • Better organ function, as living donor kidneys typically start working immediately. • Longer-lasting transplants with living donor kidneys generally last longer than deceased donor organs. For Donors: • Profound psychological satisfaction from potentially saving someone's life. • Normal life expectancy with kidney function comparable to that of healthy individuals. • No long-term medications required (unlike recipients who need anti-rejection drugs). For Healthcare Systems: • Reduced healthcare costs by decreasing the need for expensive long-term dialysis. • Increased transplant availability, helping reduce waiting list times for all patients. Risks & Potential Complications of Kidney Donation • Anesthesia-related complications are similar to those seen with other major surgical procedures. • Bleeding requiring transfusion or, rarely, additional surgery. • Infections, including wound, urinary tract, or respiratory infections. • Blood clots in legs or lungs requiring anticoagulation treatment. • Organ injury to nearby structures, hernias, or nerve damage. • Pain and fatigue that may persist for several weeks after surgery. • Limited mobility and restrictions on heavy lifting or strenuous activities. • Digestive issues, including constipation, bloating, and appetite changes. • Reduced kidney function. • Slightly increased blood pressure risk and protein in urine over time. • Small increased lifetime kidney failure risk compared to equally healthy non-donors. • Pregnancy complications such as a slightly higher risk of gestational hypertension and preeclampsia. Long-Term Health After Kidney Donation Long-term health outcomes for kidney donors remain generally positive when proper selection criteria are followed. Most donors maintain normal life expectancy and kidney function comparable to similar healthy individuals. However, regular monitoring becomes essential to detect any changes in kidney function, blood pressure, or overall health status. How to Prepare for Kidney Donation • Complete medical evaluation, including comprehensive health assessment and compatibility testing. • Psychological counseling to ensure informed decision-making and emotional readiness. • Financial planning for time off work and potential medical expenses. • Support system arrangement for post-operative care and recovery assistance. • Lifestyle modifications such as maintaining a healthy weight and avoiding harmful substances. • Education about the procedure, including understanding risks, benefits, and recovery expectations. • Legal consultation, if needed, for living donor arrangements and documentation. Kidney Donation Evaluation Process Initial screening through a phone interview or an online questionnaire. Medical history review, including detailed health assessment and family medical history. Physical examination by transplant team physicians and specialists. Laboratory testing, including blood work, urine studies, and kidney function assessment. Imaging studies, such as CT scans or MRIs, are used to evaluate kidney anatomy. Cardiovascular evaluation, including stress tests and heart function assessment. Psychological evaluation to assess mental health and decision-making capacity. Final approval by the transplant team after reviewing all evaluation results. Tests Done Before Kidney Donation • Blood tests including CBC (Complete Blood Count) Test, Kidney Function Test (KFT), and Liver Function Test (LFT). • Urine Routine Test (Urine R/M Test) to check for protein, blood, or other abnormalities. • Imaging studies such as CT angiography to assess kidney anatomy and blood vessels. • Cardiovascular tests, including electrocardiograms, echocardiograms, and stress testing. • Cancer screening appropriate for age and gender, including mammograms and colonoscopies. • Compatibility testing with the recipient using a Pre-Transplant Workup Panel, including HLA (Lymphocyte) Crossmatch – Total (T + B) Cells and Tacrolimus levels. • Psychological assessment to evaluate mental health and coping abilities. The Kidney Donation Surgery: Step-by-Step Preoperative preparation includes fasting, intravenous line placement, and anesthesia administration. Surgical positioning with the patient placed on the side to access the kidney. Incision creation is either through a minimally invasive laparoscopic approach or open surgery. Kidney mobilization is performed by carefully separating the kidney from surrounding tissues. Blood vessel preparation, including isolation of the renal artery, vein, and ureter. Kidney removal through careful dissection while preserving organ integrity. Wound closure using sutures or staples, depending on the surgical approach. Recovery monitoring in the post-anaesthesia care unit before transfer to the regular ward. Laparoscopic vs. Open Nephrectomy Aspect Laparoscopic Open Surgery Incision size Small keyhole incisions Large single incision Recovery time 2–4 weeks 4–6 weeks Pain level Less post-operative pain More significant pain Hospital stay 1–2 days 3–5 days Cosmetic result Minimal scarring Larger visible scar Complications Lower risk Slightly higher risk Recovery After Kidney Donation Most donors experience significant improvement within the first few weeks, with complete recovery typically occurring within 6–8 weeks. Effective pain control, gradual activity increase, and proper wound care form the foundation for successful recovery. During the initial recovery period, donors should expect some discomfort, fatigue, and temporary limitations on lifting and physical activities. Recovery Timeline Time Period Expected Recovery Milestones Days 1-3 Hospital stay, pain management, basic mobility Week 1 Home recovery, wound care, light activities Weeks 2-4 Gradual activity increase, possible return to desk work Weeks 4-6 Increased physical activity, lifting restrictions lifted Weeks 6-8 Full activity resumption, complete recovery for most 3-6 months Complete healing, normal kidney function established Kidney Donation Costs & Insurance Coverage Kidney donation costs vary depending on location, hospital, and insurance coverage. In India, the kidney donation process typically costs between ₹5-15 lakhs, including evaluation, surgery, and follow-up care. Many insurance policies cover living donor expenses when donation occurs for family members, but coverage varies by provider and policy terms. Can You Get Pregnant After Donating a Kidney? According to the National Kidney Foundation, women can become pregnant after donating a kidney. However, they should wait 6–12 months so the body can recover from surgery and adjust to living with one kidney. Donors should consult their doctor, as risks such as high blood pressure increase slightly after donation. Donors face slightly higher risks of gestational hypertension, preeclampsia, and gestational diabetes compared to non-donors. Kidney Donation in Older Adults Age alone doesn't disqualify kidney donation, as many healthy adults over 60 successfully donate kidneys with excellent outcomes. However, kidney donation eligibility for older adults require comprehensive medical evaluation, including detailed cardiovascular and cancer screening. Older kidney donors may experience slightly longer recovery times than younger donors. Risks of Donation for People with Genetic Conditions A family history of inherited kidney diseases, such as polycystic kidney disease or hereditary nephritis, may disqualify potential donors due to increased risk of future kidney problems. Some genetic conditions that don't directly affect the kidneys may still influence surgical risks or long-term health outcomes. Conclusion Living kidney donation can dramatically improve or save another person's life, with most kidney donors recovering well and returning to normal activities within weeks. However, kidney donation represents a major surgery with real short-term risks, including pain, bleeding, infection, and blood clots. There's also a small lifetime risk of high blood pressure and chronic kidney disease, especially in people with underlying risk factors. The kidney donation process requires thorough medical and psychological screening, clear counseling about financial and lifestyle considerations, and ongoing follow-up to ensure donor safety. Anyone considering kidney donation should engage in open discussions with the transplant team about the entire process, associated risks, potential benefits, and long-term implications. At Metropolis Healthcare, we support your health journey through comprehensive diagnostic services. Our extensive network of over 220 laboratories and 4,600+ service centres provides access to more than 4,000 tests, including specialised kidney function assessments essential for monitoring donor health. Through our convenient home sample collection service spanning 10,000+ touchpoints across India, you can access precise diagnostics designed to support informed healthcare decisions. FAQs Who can donate a kidney? • Healthy adults aged 18-65 with excellent kidney function. • No history of diabetes, high blood pressure, or heart disease. • Compatible blood type or participation in paired exchange programmes. • Passes comprehensive medical, psychological, and social evaluations. • Strong motivation and understanding of lifelong commitment required. Is kidney donation safe? Kidney donation risks are minimal when performed in carefully selected, healthy individuals. Modern surgical techniques and comprehensive preoperative screening significantly reduce complications, making it generally safe. How long is the kidney donation recovery time? Most kidney donors return to normal activities within 4-6 weeks, though complete recovery may take 3-4 months. Hospital stays typically last 1-3 days with gradual activity resumption. What disqualifies you from donating a kidney? • Active cancer, diabetes, or uncontrolled high blood pressure. • Significant heart, lung, or liver disease. • History of kidney stones, blood clots, or psychiatric illness. • Substance abuse, obesity, or incompatible blood type without exchange options. • Age under 18 or inability to provide informed consent. Do kidney donors live a normal life? Yes, kidney donors typically maintain normal, healthy lives with one kidney. Regular monitoring ensures optimal health, and most donors experience no long-term functional limitations. Can I drink alcohol after donating a kidney? Moderate alcohol consumption is generally acceptable after kidney donation recovery. However, excessive drinking can strain your remaining kidney, so moderation remains important for long-term health. Does donating a kidney shorten your lifespan? Research indicates that kidney donors have similar or slightly better life expectancy compared to the general population, likely due to careful health screening and ongoing medical care. Can you donate a kidney if your blood type doesn't match? Yes, through paired kidney exchange programmes or ABO-incompatible transplantation with special medications, blood type differences can often be overcome successfully. Can you donate a kidney more than once? No, you can only donate one kidney during your lifetime. After donation, your remaining kidney adapts to handle the increased workload effectively.