Web Stories
Latest Blogs
What Is A Penis? Function, Purpose & Health Facts
What Is a Penis? The penis is an external male genital organ that serves multiple essential functions in the human body. The penis enables urination by allowing urine to exit the body through the urethra, while also facilitating sexual reproduction by delivering sperm during intercourse. The penis consists of specialised tissues designed to perform these dual functions effectively. Its unique structure allows it to change from a soft, relaxed state to a firm, erect condition when blood flow increases to the erectile tissues. The penis is essentially a complex structure containing blood vessels, nerves, and specialised tissues that work together to support both everyday bodily functions and reproductive health. Penis Anatomy Overview The penile structure comprises three main anatomical regions: the root, shaft, and glans. The root anchors the penis to the pelvic bones and provides stability, and the shaft forms the main body containing the erectile tissues. The glans, or head, represents the sensitive tip where the urethra opens to allow the passage of urine and semen. The penile structure includes both external features you can see and internal components that enable function. Externally, you’ll notice the shaft, glans, and, in uncircumcised men, the foreskin. Internally, the penis contains three cylindrical chambers of erectile tissue, blood vessels, nerves, and the urethra that runs through the centre. External Anatomy of the Penis • Glans (head): The rounded, sensitive tip containing the urethral opening where urine and semen exit the body. • Shaft (body): The cylindrical main portion extending from the root to the glans, housing the erectile tissues. • Foreskin (prepuce): The retractable skin covering the glans in uncircumcised males, providing protection and sensitivity. • Coronal ridge: The prominent rim where the glans meets the shaft, containing numerous nerve endings. • Urethral opening (meatus): The small opening at the tip of the glans through which bodily fluids pass. • Frenulum: The sensitive band of tissue connecting the foreskin to the underside of the glans. These external structures work together to facilitate sexual function and urinary elimination, providing protective covering for sensitive internal tissues. Internal Anatomy of the Penis • Corpora cavernosa: Two parallel cylinders of erectile tissue running along the top of the shaft that fill with blood during arousal. • Corpus spongiosum: The central column of erectile tissue surrounding the urethra and forming the glans. • Urethra: The tube carrying urine from the bladder and semen from the male reproductive system out of the body. • Tunica albuginea: The tough fibrous layer surrounding the erectile tissues, essential for maintaining rigidity during erection. • Buck's fascia: The deep layer of tissue providing structural support to the penis. • Root structures: The crura and bulb that anchor the penis to the pelvic bones and perineum. This complex internal architecture enables the penis to transform from a flaccid state to a rigid erection through coordinated blood flow changes. Blood Supply & Nerves of the Penis The penis receives blood through a sophisticated vascular network primarily supplied by the internal pudendal arteries. These vessels branch into dorsal, deep, and bulbourethral arteries, each serving specific penile structures. During erection, arterial blood flow increases dramatically while venous drainage decreases, creating the hydraulic mechanism enabling rigidity. Penile nerve supply involves both sensory and autonomic components essential for normal function. The pudendal nerve provides sensation to the glans and shaft, whereas autonomic nerves from spinal segments S2-S4 control the erection and ejaculation processes. This intricate nervous system coordination ensures proper sexual response and urinary control. Diabetes, cardiovascular disease, and neurological disorders can disrupt these systems, leading to erectile dysfunction or other complications requiring medical attention. Penis Shape, Size & Types Penis types vary naturally among men, with significant differences in size, shape, and appearance being completely normal. The average penis measures approximately 13–14 cm in length (when erect) and 8–9 cm (when flaccid), though this varies considerably from person to person. Natural variations in penis anatomy include differences in: • Length: Ranging from shorter to longer than average, all within normal parameters. • Girth: Some penises are naturally thicker or thinner than others. • Shape: Cylindrical forms with varying degrees of natural curvature. • Glans size: The head may be proportionally larger, smaller, or similar in size to the shaft. • Foreskin presence: Circumcised versus uncircumcised appearances. • Colour variation: Natural pigmentation differences along the shaft and glans. Different Penis Shapes (Naturally Occurring Variations) • Straight: Minimal curvature in any direction, representing the most common configuration. • Upward curve: Natural bend towards the abdomen, often enhancing sensation during certain positions. • Downward curve: Bend away from the body, which may be more noticeable when erect. • Left or right curve: Lateral curvature to either side, usually present since development. • Slight twist: Mild rotation along the shaft's length, generally not problematic. • Tapered shape: Gradual narrowing from base to tip or vice versa. Functions of the Penis • Urination: Enables the elimination of waste products and excess water from the body through the urine system. • Sexual reproduction: Facilitates sperm delivery into the female reproductive tract during intercourse. • Erectile function: Allows for penetration during sexual activity through blood engorgement of erectile tissues. • Ejaculation: Expels semen containing sperm during orgasm, essential for reproduction. • Sexual pleasure: Provides sensory experiences through numerous nerve endings, particularly in the glans. • Hormonal response: Influenced by testosterone and other hormones that regulate sexual development and function. Common Conditions Affecting the Penis • Erectile dysfunction: Persistent difficulty achieving or maintaining erections sufficient for sexual activity. • Peyronie’s disease: Development of fibrous scar tissue in the tunica albuginea causing abnormal penile curvature and pain. • Phimosis: Inability to fully retract the foreskin over the glans, potentially causing discomfort or hygiene issues. • Paraphimosis: Foreskin trapped behind the glans, requiring immediate medical attention to prevent complications. • Balanitis: Inflammation of the glans often caused by bacterial or fungal infections. • Priapism: Prolonged, painful erections unrelated to sexual stimulation requiring emergency treatment. • Penile cancer: A rare malignancy that may present as lumps, sores, or unusual growths. • Urethral stricture: Narrowing of the urethra that can impede urine flow. When Penis Shape or Curve Is Considered Normal Most natural variations in penis anatomy fall within normal parameters and don't require medical intervention. Mild curvature present since puberty is typically considered a normal variant of penile structure. The key factors determining whether curvature is normal include its presence since development, absence of pain, and lack of functional impairment. It’s normal for many men to have a slight bend or curve in their penis. Curves of about 30 degrees or less are usually harmless and simply reflect natural differences that occur during development. Unless the curvature causes pain or difficulty during sexual activity, it’s considered completely normal. It's important to distinguish between congenital curvature (present since development) and acquired curvature (developing later in life). Congenital variations are almost always benign, while sudden changes in penis shape may indicate underlying conditions requiring medical evaluation. When Penis Curvature Needs Medical Attention Sudden onset curvature in adulthood often indicates Peyronie's disease or other pathological conditions, requiring professional treatment. Warning signs requiring medical consultation include: • Sudden onset of curvature in adulthood, particularly if accompanied by pain or lumps. • Progressive worsening of existing curvature over time. • Pain during erections or sexual activity related to the curvature. • Difficulty with penetration during intercourse due to the degree of bend. • Palpable plaques or hard areas under the penile skin. • Associated erectile dysfunction or changes in rigidity. • Emotional distress or relationship difficulties related to penile appearance. How Penis Disorders Are Diagnosed Medical history: Comprehensive assessment of symptoms, sexual history, medical conditions, medications, and lifestyle factors that might contribute to penile problems. Physical examination: Thorough visual and tactile examination of the penis, including assessment of size, shape, skin condition, and any abnormalities. Imaging tests: Ultrasound examinations to assess blood flow, tissue structure, or detect plaques in cases of curvature disorders. Laboratory tests: Blood work to evaluate hormone levels, including: Free Testosterone Test, FSH–LH–Testosterone Profile, FSH–LH–Prolactin–Testosterone Profile, and Comprehensive Thyroid Panel. Glucose control: Tests such as HbA1c and Fasting Blood Sugar (FBS) evaluate blood glucose regulation Markers of systemic conditions: Complete Blood Count (CBC), Lipid Profile Test, Liver Function Test (LFT), and Kidney Function Test (KFT) Nocturnal penile tumescence (NPT) testing: Specialized evaluation to determine whether erectile dysfunction is physical or psychological. This comprehensive approach ensures accurate diagnosis and enables the development of targeted treatment strategies for optimal outcomes. Treatments for Common Penis Conditions Treatment approaches for penile conditions vary depending on the specific diagnosis, severity, and impact on quality of life. • Oral medications: PDE5 inhibitors for erectile dysfunction, antibiotics for infections, or anti-inflammatory drugs for certain conditions. • Topical treatments: Creams or gels for skin conditions, infections, or localized inflammatory processes. • Injection therapy: Direct medication injection into penile tissues for erectile dysfunction or Peyronie's disease. • Surgical procedures: Corrective surgery for severe curvature, circumcision for phimosis, or cancer treatment. • Mechanical devices: Vacuum erection devices, penile implants, or traction therapy for specific conditions. • Lifestyle modifications: Diet changes, exercise programs, smoking cessation, or stress management techniques. • Psychological support: Counselling or therapy for conditions with psychological components or emotional impacts. • Combination approaches: Often, the most effective treatment involves multiple interventions working together. Daily Penis Care & Hygiene Tips Proper penile hygiene prevents infections, reduces odour, and maintains overall genital health throughout life. Daily cleaning routines should be gentle yet thorough, focusing on removing accumulated debris and avoiding harsh chemicals that might irritate. Essential hygiene practices include: • Daily washing with warm water and mild soap, paying special attention to the glans area. • Thorough cleaning under the foreskin for uncircumcised men to prevent smegma accumulation. • Complete drying after washing to prevent moisture-related bacterial or fungal growth. • Wearing clean, breathable cotton underwear that allows adequate air circulation. • Urinating after sexual activity to flush bacteria from the urethral opening. • Avoiding harsh chemicals, perfumed products, or aggressive scrubbing that might irritate. These simple practices significantly reduce infection risk and maintain optimal penile health throughout life. Lifestyle Tips for Better Penis Health Supporting overall penile health requires attention to factors that influence circulation, hormone levels, and general well-being. Key lifestyle recommendations include: • Regular cardiovascular exercise to maintain healthy blood flow is essential for erectile function. • Maintaining a healthy weight to reduce pressure on blood vessels and support hormone balance. • Avoiding tobacco products that can damage blood vessels and impair erectile capability. • Limiting alcohol consumption, which can affect both sexual performance and long-term health. • Managing stress through healthy coping mechanisms, as chronic stress can impact sexual function. • Following a balanced diet rich in nutrients that support vascular health and hormone production. • Getting adequate sleep to support hormone regulation and overall health. • Safe sexual practices, including condom use and regular STI screening. • Regular medical checkups to monitor for diabetes, hypertension, and other conditions affecting sexual health. When to See a Doctor or Urologist • Persistent pain, unusual lumps, or sores that don't heal within a reasonable timeframe. • Changes in urination patterns, including difficulty starting, weak stream, or burning sensations. • Erectile dysfunction that persists or worsens over time. • Sudden onset or worsening of penile curvature. • Unusual discharge, persistent swelling, or significant colour changes. • Signs of infection, such as fever, severe pain, or foul-smelling discharge. • Any concerns about sexual function, sensation, or appearance that affect your quality of life. Don't hesitate to seek professional advice when you notice concerning changes. Early consultation often leads to simpler, more effective treatments than delayed intervention. Conclusion Understanding penis anatomy, function, and overall health is an essential part of men’s healthcare that deserves thoughtful attention. The penis plays key roles in both urinary and reproductive systems, so having clear knowledge about its structure and normal variations helps you maintain confidence and well-being. Good hygiene, healthy habits, and staying alert to changes in your body form the foundation of proper penile care. Most issues involving anatomy, function, or sexual health can be effectively treated when addressed early. Never let embarrassment prevent you from seeking help, as doctors handle these topics with respect, expertise, and compassion, ensuring you receive the support you need. At Metropolis Healthcare, we understand the importance of comprehensive health monitoring for men's well-being. Our extensive portfolio of over 4,000 diagnostic tests includes specialized panels for hormonal and metabolic assessment, infection screening, and overall health evaluation that support male reproductive health. Through our network of more than 220 laboratories and 10,000+ touchpoints across India, we provide convenient at-home sample collection services, ensuring comfort and privacy for sensitive health concerns. FAQs What is the normal size and shape of a penis? Penis size and shape vary widely among healthy men. The average penis measures approximately 13–14 cm in length (when erect) and 8–9 cm (when flaccid). A slight curve is common and normal, provided it doesn't cause pain or functional problems. Why does my penis curve? A slight curve during erection is typical and often results from natural differences in tissue elasticity within the penile structure. However, significant or painful bending may indicate Peyronie's disease, involving scar tissue development requiring medical evaluation. Can penis size increase naturally? No scientifically proven methods exist to significantly increase penis size naturally. Most advertised supplements, exercises, or devices lack evidence and may cause harm. Penis size typically doesn't impact sexual satisfaction or functional ability. What causes pain in the penis? Penile pain may result from infections, injuries, inflammation like balanitis, curvature disorders such as Peyronie's disease, priapism, or trauma. Persistent or severe pain should always be evaluated by healthcare providers promptly. Is it normal for the foreskin not to retract? In young children, non-retractable foreskin is normal. In adults, persistent inability to retract the foreskin may indicate phimosis, which sometimes requires treatment if causing symptoms, infections, or hygiene problems. How often should I clean my penis? Gently wash the penis with warm water daily, including careful cleaning under the foreskin if uncircumcised. Avoid harsh soaps and ensure complete drying before dressing to prevent infections. Can stress affect erections? Yes, stress and anxiety commonly cause temporary erectile difficulties by disrupting hormonal balance and blood flow to the penis. Managing stress through relaxation techniques, exercise, and counselling often improves sexual function significantly. References https://my.clevelandclinic.org/health/body/penis https://www.ncbi.nlm.nih.gov/books/NBK482236/ https://academic.oup.com/jsm/article/22/2/225/7921439?login=false https://www.niddk.nih.gov/health-information/urologic-diseases/penile-curvature-peyronies-disease https://uroweb.org/guidelines/sexual-and-reproductive-health/chapter/penile-curvature https://www.mayoclinic.org/healthy-lifestyle/mens-health/in-depth/penis-health/art-20046175
Neuroblastoma: A Childhood Cancer Explained – Symptoms, Treatment & Outlook
What is Neuroblastoma? Neuroblastoma is a childhood cancer that begins in immature nerve cells (neuroblasts), which grow and divide uncontrollably instead of maturing into normal nerve cells. It usually develops before birth or in early childhood, most often in the abdomen, and accounts for approximately 8–10% of all childhood cancers. The encouraging news is that, with modern treatments and early diagnosis, many children with neuroblastoma now have much better outcomes than in the past. Who Gets Neuroblastoma? Neuroblastoma mainly affects very young children, with most cases diagnosed before the age of five and mostly occurring in children under ten; the median age at diagnosis is about 17 months. Uniquely, in some infants under one year, neuroblastoma can even regress spontaneously, disappearing without treatment. According to StatPearls, neuroblastoma is the most common tumour of the sympathetic nervous system. It is classified as an embryonal neuroendocrine tumour that arises from neural crest progenitor cells along the sympathetic chain, most commonly in the adrenal glands, and accounts for about 10.2 cases per million children and is responsible for roughly 15% of childhood cancer–related deaths. Where Neuroblastoma Develops in the Body Neuroblastoma can develop wherever sympathetic nerve tissue is found throughout the body. The most common locations include: Adrenal glands (above the kidneys) – Approximately 40% of neuroblastoma cases originate here, often appearing as an adrenal gland tumour. Abdomen – Including areas around the spine and major blood vessels. Chest – Particularly in the area behind the lungs. Neck – Along the cervical sympathetic chain. Pelvis – Near the tailbone and lower spine. Bone marrow – Where the cancer may spread from its original location. Causes & Risk Factors Understanding neuroblastoma causes can help families process their child's diagnosis, though it's important to know that in most cases, there's nothing parents could have done to prevent it. The main factors include: Genetic mutations – Random changes in nerve cell DNA that occur during development. Hereditary factors – Very rare inherited gene mutations (less than 2% of cases). Developmental timing – Problems during foetal nerve cell development. Unknown environmental factors – Most causes remain unclear. Age – Being under five years old significantly increases risk. Family history – Extremely rare, though some families may carry inherited gene mutations. How Neuroblastoma Develops (Pathophysiology) Neuroblastoma develops when immature nerve cells (neuroblasts) acquire genetic mutations, fail to mature, and instead grow uncontrollably into tumours that can spread through the blood or lymph. In some young children, these tumours may grow slowly or even shrink on their own. In contrast, others are highly aggressive, so each case is biologically distinct and requires individualised treatment. Types of Neuroblastoma Doctors classify neuroblastoma into several types based on how the cancer cells look under a microscope and how they behave: Ganglioneuroblastoma – Contains both immature and more mature nerve cells, often less aggressive. Poorly differentiated neuroblastoma – Cells look very different from normal nerve cells. Undifferentiated neuroblastoma – Cells show no signs of nerve cell development. Differentiating neuroblastoma – Shows some signs of maturing into nerve cells. Stages of Neuroblastoma (INRG/INSS) Neuroblastoma stages help doctors understand how far the cancer has spread and plan treatment accordingly. The International Neuroblastoma Staging System includes: Stage 1 – Localised tumour that can be completely removed surgically. Stage 2A – Localised tumour that cannot be completely removed, but nearby lymph nodes are cancer-free. Stage 2B – Localised tumour with cancer in nearby lymph nodes on the same side. Stage 3 – Tumour that has spread across the midline of the body or to lymph nodes on the opposite side. Stage 4 – Cancer that has spread to distant parts of the body. Stage 4S – A special category for infants younger than one year, with limited spread to liver, skin, or bone marrow. Common Symptoms of Neuroblastoma Recognising neuroblastoma symptoms early can lead to faster diagnosis and treatment. However, these symptoms can be subtle and may resemble common childhood illnesses. General neuroblastoma symptoms include: Persistent abdominal pain or swelling Unexplained lumps or masses that parents can feel Chronic fatigue or weakness Loss of appetite and weight loss Fever without an obvious cause Bone pain, especially at night Dark circles around the eyes Bruising or bleeding easily Changes in bowel or bladder habits Difficulty breathing or a persistent cough Symptoms Based on Tumour Location The location where neuroblastoma develops significantly influences the symptoms your child might experience: Abdominal tumours – Swelling, pain, constipation, difficulty eating. Chest tumours – Breathing problems, persistent cough, chest pain. Neck tumours – Swelling, difficulty swallowing, voice changes. Spinal tumours – Back pain, weakness in arms or legs, walking difficulties. Bone marrow involvement – Fatigue, pale skin, easy bruising, frequent infections. How Neuroblastoma is Diagnosed Diagnosing neuroblastoma involves several steps that help doctors confirm the presence of cancer and determine its extent: Complete medical history and physical examination – Your doctor will ask about symptoms and examine your child carefully. Blood and urine tests – To check for substances produced by neuroblastoma cells. Imaging studies – Various scans to locate tumours and assess their size. Biopsy – Taking a small tissue sample to confirm the diagnosis. Bone marrow examination – To check if cancer has spread to the bone marrow. Additional staging tests – To determine the exact stage and plan treatment. Diagnostic Tests For Neuroblastoma Several specific tests help doctors diagnose and stage neuroblastoma effectively: Ultrasound – Uses sound waves to create images of internal organs. CT (computed tomography) scan – Detailed cross-sectional images of the body. MRI (magnetic resonance imaging) – High-resolution images using magnetic fields. MIBG scan – A Special nuclear medicine test that highlights neuroblastoma cells. PET scan – Shows areas of high metabolic activity that may indicate cancer. Bone scan – Detects cancer spread to bones. Catecholamines in urine – Measures substances produced by neuroblastoma cells. Catecholamines in Plasma - Measures stress hormones, often raised in neuroblastoma. MYCN (N-MYC) gene amplification test – Tumour genetic test for MYCN amplification, key for prognosis and treatment intensity. Homovanillic acid (HVA), urine – Measures dopamine breakdown products often elevated in neuroblastoma. Vanillylmandelic acid (VMA), 24-hour urine – Measures adrenaline breakdown products often elevated in neuroblastoma. Prognostic Indicators Several factors help doctors predict how well a child with neuroblastoma might respond to treatment: Age at diagnosis – Younger children, especially infants, often have better outcomes. Stage of disease – Earlier stages typically have more favourable prognoses. MYCN gene status – Tumours without MYCN amplification generally respond better to treatment. Tumour histology – How the cancer cells look under a microscope. Chromosome abnormalities – Certain genetic changes affect treatment response. Location of primary tumour – Some locations are associated with better outcomes. Treatment Options for Neuroblastoma Modern neuroblastoma treatment combines multiple approaches tailored to each child's specific situation. Treatment options include: Surgery – To remove tumours and obtain tissue samples Chemotherapy – Powerful medicines that destroy cancer cells throughout the body Radiation therapy – High-energy beams that target cancer cells Immunotherapy – Treatments that help the immune system fight cancer Stem cell transplant – For high-risk cases requiring intensive treatment Targeted therapy – Drugs that attack specific features of cancer cells Supportive care – Managing side effects and maintaining quality of life Low-Risk vs High-Risk Treatment Approaches Treatment intensity depends on the child’s risk group. Low-risk neuroblastoma may need only observation or surgery, as some tumours, especially in infants, can regress on their own. On the other hand, intermediate-risk cases usually receive moderate chemotherapy plus surgery. High-risk neuroblastoma needs intensive multimodal therapy (high-dose chemotherapy, surgery, radiation, stem cell transplant, and immunotherapy), which is demanding but has significantly improved survival in aggressive disease. Stem Cell Transplantation for High-Risk Neuroblastoma For children with high-risk neuroblastoma, stem cell transplant represents a crucial treatment component. This procedure allows doctors to give very high doses of chemotherapy that would otherwise be too toxic for the bone marrow. Before treatment, doctors collect the child's healthy stem cells. After intensive chemotherapy destroys both cancer cells and bone marrow, the stored stem cells are returned to restore the child's ability to produce blood cells. Immunotherapy for Neuroblastoma Immunotherapy has revolutionised neuroblastoma treatment, particularly for high-risk cases. These treatments help the child's immune system recognise and destroy neuroblastoma cells more effectively. Monoclonal antibodies—such as anti-GD2—target specific proteins found on neuroblastoma cells, specifically target proteins found on neuroblastoma cells. This targeted approach has improved survival rates while potentially reducing some side effects compared to traditional chemotherapy alone. Potential Complications & Long-Term Effects While neuroblastoma treatment saves lives, it can sometimes cause long-term effects that require ongoing attention: Growth and development delays – Some treatments may affect normal growth patterns. Hearing problems – Certain chemotherapy drugs can damage hearing. Heart function changes – Some treatments may affect heart health. Kidney function issues – Monitoring kidney health throughout and after treatment. Learning difficulties – Some children may experience cognitive changes. Secondary cancers – Very rare, but there is a slightly increased risk of developing other cancers later in life. Fertility concerns – Some treatments may affect future reproductive health. Living With and Managing Neuroblastoma Managing life during and after neuroblastoma treatment requires comprehensive support and planning: Regular medical follow-up – Ongoing monitoring for recurrence and late effects Educational support – Helping children maintain or catch up with schooling Nutritional guidance – Ensuring proper nutrition during treatment and recovery Physical therapy – Maintaining strength and mobility throughout treatment Psychological support – Counselling for children and families Peer support groups – Connecting with other families facing similar challenges Sibling support – Helping brothers and sisters cope with the family’s experience Survival Rates & Prognosis The outlook for children with neuroblastoma has improved greatly in recent decades. Five-year survival rates exceed 95% for low-risk cases and 90–95% for intermediate-risk disease. Even in high-risk neuroblastoma, modern intensive treatments have raised five-year survival to around 50–60%, from much lower levels earlier. Many survivors go on to live normal, healthy lives, though some need long-term follow-up for late effects of treatment. When to See a Doctor Parents should consult their child's doctor if they notice any concerning symptoms that persist or worsen: Persistent abdominal pain or swelling that doesn't resolve with time Unexplained lumps or masses anywhere on the child's body Chronic fatigue or weakness that interferes with normal activities Persistent fever without an obvious cause Unexplained bone pain, especially at night or with activity Changes in appetite, weight loss, or failure to thrive Unusual bruising or bleeding that seems excessive Any neurological symptoms, like weakness, balance problems, or changes in reflexes. Conclusion When a child is facing a serious condition like neuroblastoma, timely and accurate diagnosis becomes the foundation of effective care. Timely diagnosis helps precise staging, and close monitoring during and after treatment, giving doctors the information they need to plan the best possible way forward. Early diagnosis and regular monitoring are easier when quality diagnostics are within reach. With 4,000+ tests, full body checkups, and a wide range of speciality testing, you get comprehensive care under one roof with Metropolis Healthcare. Our home sample collection network with 10,000+ touchpoints ensures comfort and accessibility, while quick turnaround times and a strong focus on accurate results support timely treatment decisions. You can book tests through our website, phone, app, or WhatsApp, making it simple to choose the option that best fits your routine. FAQs What causes neuroblastoma? Neuroblastoma usually develops due to random genetic changes in immature nerve cells during early development. In most children, it is not inherited, and there is no clear environmental cause. Rarely, inherited mutations in genes like ALK or PHOX2B can run in families and increase risk. Is neuroblastoma curable? Yes. Many children, especially those with low- or intermediate-risk neuroblastoma, are cured and live normal lives. Cure is more challenging in high-risk disease, but survival continues to improve with modern multimodal treatment, immunotherapy and clinical trials. How is neuroblastoma detected early? There is no universal screening test for neuroblastoma. Early detection relies on: Parents and caregivers notice persistent, unusual symptoms Regular pediatric checkups Prompt evaluation of signs like abdominal lumps, bone pain, unexplained fevers or neurological symptoms Imaging (ultrasound, CT/MRI) and lab tests are done once a doctor suspects a tumour. At what age is neuroblastoma most commonly diagnosed? Neuroblastoma primarily affects infants and young children under five years of age, with the highest number of cases in the first year of life. Only a small percentage of cases occur in older children, teenagers or adults. What is the survival rate of neuroblastoma? Survival depends on the risk group: Low-risk: around 95–98% five-year survival Intermediate-risk: roughly 90–95% High-risk: around 50–60%, though this varies and is improving with newer therapies Your child’s oncology team will explain the individual prognosis based on stage, biology and treatment response. Can neuroblastoma come back after treatment? Yes. Relapse can occur, especially in children with high-risk disease. Recurrent or relapsed neuroblastoma can be more difficult to treat and may require additional chemotherapy, radiation, stem cell transplant, targeted therapy, immunotherapy or clinical trials, so long-term follow-up remains essential. References https://www.mayoclinic.org/diseases-conditions/neuroblastoma/symptoms-causes/syc-20351017 https://my.clevelandclinic.org/health/diseases/14390-neuroblastoma https://emedicine.medscape.com/article/988284-overview https://www.ncbi.nlm.nih.gov/books/NBK448111/
Mononucleosis: 'Mono' Explained – Causes, Symptoms & Recovery Tips
What is Mononucleosis? Mononucleosis (‘mono’ or the ‘kissing disease’) is a contagious viral infection, most commonly caused by the Epstein-Barr virus (EBV). It spreads through saliva and primarily affects the lymphatic system, leading to extreme fatigue, fever, and swollen lymph nodes. It develops gradually over several weeks and is often more severe in people aged 15–25, though anyone can be affected. Most people recover in 2–4 weeks, though tiredness may linger for months, and the infection usually provides lifelong immunity, making repeat infections very rare. What Causes Mononucleosis? Understanding mono causes helps you take preventive measures and recognise risk factors. The primary causes include: Epstein-Barr virus (EBV) - According to the National Library of Medicine (NIH) and the Centers for Disease Control and Prevention (CDC), up to 95% of adults worldwide are EBV-seropositive, and at least 1 in 4 (≈25%) teenagers and young adults infected with EBV go on to develop clinical mono. Cytomegalovirus (CMV) - A less common cause that can produce a mono-like illness, especially in adults. Human herpesvirus 6 – Occasionally triggers a mono-like illness. Adenovirus - a rare cause of mononucleosis symptoms. Toxoplasma gondii - parasitic infection mimicking mononucleosis. How Mononucleosis Spreads Mononucleosis spreads primarily through contact with infected saliva hence the nickname ‘kissing disease’ but it can also spread through sharing drinks, utensils, toothbrushes, or food, and through respiratory droplets in close-contact settings like schools or dormitories. The virus may survive for some time on surfaces and, though rare, can be transmitted via blood transfusions or organ transplants. Infected people can spread the virus before they feel sick and for weeks or months after recovery, making prevention difficult and leading to outbreaks in close-knit groups. Symptoms of Mononucleosis Recognising mono symptoms early enables prompt medical attention and appropriate self-care measures. Common symptoms include: Extreme fatigue lasting weeks or months High fever reaching 38-39°C (100-102°F) Severe sore throat, often mistaken for strep throat. Swollen lymph nodes, particularly in the neck and armpits Swollen tonsils with a white or yellow coating Headache and body aches Loss of appetite and nausea Skin rash appearing as small red spots Enlarged spleen causing abdominal tenderness Enlarged liver (hepatomegaly), which can cause jaundice in severe cases When Do Mononucleosis Symptoms Appear? Symptoms of mononucleosis usually appear four to seven weeks after infection, with younger children tending to have a shorter incubation and milder illness, and teens/adults experiencing a longer delay and more severe symptoms. Unlike sudden infections like flu, mono starts gradually with mild fatigue and sore throat that worsen over 1–2 weeks before peaking, then improve slowly over the next few weeks. Complications of Mononucleosis While most people recover completely from mononucleosis, serious complications can occur, particularly in severe cases: Splenic rupture – A life-threatening emergency that requires immediate medical attention Severe airway obstruction from massively swollen tonsils Secondary bacterial infections, including strep throat or pneumonia Hepatitis with elevated liver enzymes and jaundice Severe anaemia from decreased red blood cell production Thrombocytopenia – A condition that causes easy bruising and bleeding Neurological complications, including meningitis or encephalitis Chronic fatigue syndrome, persisting months after an acute infection How Mononucleosis is Diagnosed Detailed medical history: Doctors focus on symptoms and potential exposures and take a detailed history. Physical examination: They check for swollen lymph nodes, the spleen, and the liver, and may suggest certain diagnostic tests based on these findings. Mononucleosis Test – Detects antibodies against the Epstein-Barr virus (EBV). Common tests include the Monospot test, EBV DNA detection by PCR, or an Infectious Mononucleosis Profile (IFA), you may have to take an Infectious Mononucleosis Profile by IFA - Serum test or an EBV DNA Detection by PCR test. Complete Blood Count (CBC) – Identifies elevated lymphocytes and atypical white blood cells often seen in mono Liver Function Test (LFT): For assessing potential hepatic involvement EBV-specific antibody tests: Tests like EBV VCA IgM Antibody or EBV VCA IgG Antibody help confirm active or past infection. Mononucleosis Treatment Options There’s no specific antiviral cure for mononucleosis, so treatment focuses on rest, fluids, and relieving symptoms while your immune system clears the infection. Adequate rest and hydration are essential, and over-the-counter pain relievers like paracetamol or ibuprofen can ease fever, headache, and throat pain. Antibiotics aren’t useful unless there’s a bacterial infection, and corticosteroids are reserved only for severe throat swelling that threatens breathing. Home Care Tips for Mononucleosis Recovery Effective home management accelerates recovery and reduces symptom severity: Prioritise rest – Aim for 10–12 hours of sleep per night, and nap when fatigued. Stay hydrated - drink water, herbal teas, and clear broths regularly. Eat nutritious foods - focus on easily digestible, nutrient-rich options. Gargle salt water - mix 1 teaspoon salt in warm water for sore throat relief. Use throat lozenges - choose varieties with anaesthetic properties. Apply warm compresses - reduce lymph node discomfort. Avoid alcohol – It helps protect your liver, which may be temporarily inflamed. Practice good hygiene - prevent spreading infection to others. How Long Does Mononucleosis Last? Mononucleosis usually causes acute symptoms for 2–4 weeks, but full recovery often takes 2–3 months, with fatigue lasting the longest. In some people—especially those who don’t rest enough—tiredness can persist for 6 months or more. Teens and young adults tend to recover more slowly than children, and factors such as overall health, stress, and returning to normal activities too soon can further delay recovery and increase the risk of complications. Mononucleosis in Teenagers and Young Adults Teenagers and young adults (especially ages 15–24) have the highest risk of severe mononucleosis, with more intense symptoms and longer recovery than other age groups. College students and school pupils are particularly vulnerable due to close living spaces and frequent social contact. Their busy academic and social schedules often clash with the need for extended rest, making it harder to recover fully and potentially prolonging illness. Understanding these challenges helps families and students adjust routines to allow proper healing. Is Mononucleosis Contagious? Mononucleosis remains highly contagious throughout the illness and for weeks afterwards. You can transmit the virus before symptoms appear, during the acute illness phase, and for months following recovery. The prolonged shedding period makes complete prevention challenging, even with careful precautions. Because mononucleosis is contagious, individuals should avoid close contact with others—especially those with weakened immune systems—until symptoms subside from vulnerable individuals, particularly those with compromised immune systems. However, mononucleosis isn't as easily transmitted as common respiratory viruses, so it requires closer contact for infection to occur. How to Prevent Mononucleosis? While complete prevention isn't always possible, these strategies significantly reduce your infection risk: Avoid sharing personal items - don't share drinks, utensils, or toothbrushes. Practice good hand hygiene - wash hands frequently with soap and water. Avoid close contact with known infected individuals. Don't share food - avoid eating from others' plates or sharing snacks. Maintain a healthy lifestyle - adequate sleep and nutrition support immune function. Avoid kissing infected individuals or those with unknown status. Clean surfaces regularly - disinfect commonly touched areas. Stay home when ill – Helps prevent spreading infection to others. When to See a Doctor? Seek immediate medical attention if you experience these warning signs: Severe abdominal pain - may indicate splenic rupture. Difficulty breathing or swallowing from throat swelling. High fever persists despite treatment. Signs of dehydration - decreased urination, dizziness, or confusion. Yellowing skin or eyes - indicates liver involvement. Severe headache with neck stiffness. Unusual bleeding or extensive bruising. Worsening symptoms after initial improvement. Conclusion Mononucleosis can be exhausting, but it’s usually temporary and manageable that improves with rest, hydration, good nutrition, and timely medical care. Thus, it is important to seek professional medical consultation and have diagnostic tests done at the right time for a quick recovery. At Metropolis Healthcare, our more than 4,000 test profiles, including specialised viral panels and full-body checkups, along with fast, accurate results, make diagnosis and follow-up easy. You can book tests with our strong home sample collection network (10,000+ touchpoints) conveniently via our website, call, app, or WhatsApp, so you get the support you need right from home. FAQs What does mononucleosis feel like? Mononucleosis feels like a severe, prolonged flu combined with overwhelming exhaustion that makes even simple tasks feel difficult. The sore throat often feels like swallowing glass, while the fatigue can be so profound that climbing stairs becomes challenging. Many people describe feeling completely drained, as if their energy has been completely depleted. Can you get mononucleosis twice? You typically cannot get mononucleosis twice from the same virus, as infection provides lifelong immunity. However, different viruses can cause mono-like symptoms, so you might experience similar illness from cytomegalovirus or other pathogens. Reactivation of dormant Epstein-Barr virus rarely causes symptomatic illness in healthy individuals. Is mono dangerous? Mononucleosis is generally not dangerous for healthy individuals, though serious complications can occur. The greatest risks include splenic rupture from an enlarged spleen and airway obstruction from severely swollen tonsils. Most people recover completely without lasting effects, making mononucleosis more disruptive than dangerous. How is mono different from the flu? Mononucleosis develops gradually over weeks, while influenza typically begins suddenly within days. The extreme fatigue and swollen lymph nodes characteristic of mononucleosis distinguish it from flu symptoms. Additionally, mononucleosis lasts much longer than typical influenza, often requiring weeks or months for complete recovery. How long should you avoid sports after mononucleosis? You should avoid contact sports and strenuous physical activity for at least 3-4 weeks after mononucleosis diagnosis, or until your doctor confirms your spleen has returned to normal size. This precaution prevents potentially life-threatening splenic rupture from physical trauma during sports participation. References https://www.ncbi.nlm.nih.gov/books/NBK470387/ https://www.mayoclinic.org/diseases-conditions/mononucleosis/symptoms-causes/syc-20350328 https://my.clevelandclinic.org/health/diseases/13974-mononucleosis https://www.cdc.gov/epstein-barr/about/mononucleosis.html https://www.who.int/news-room/questions-and-answers/item/mononucleosis-(glandular-fever) https://www.healthline.com/health/mononucleosis
Kidney Cysts: What They Are, When They're Harmful & What to Do
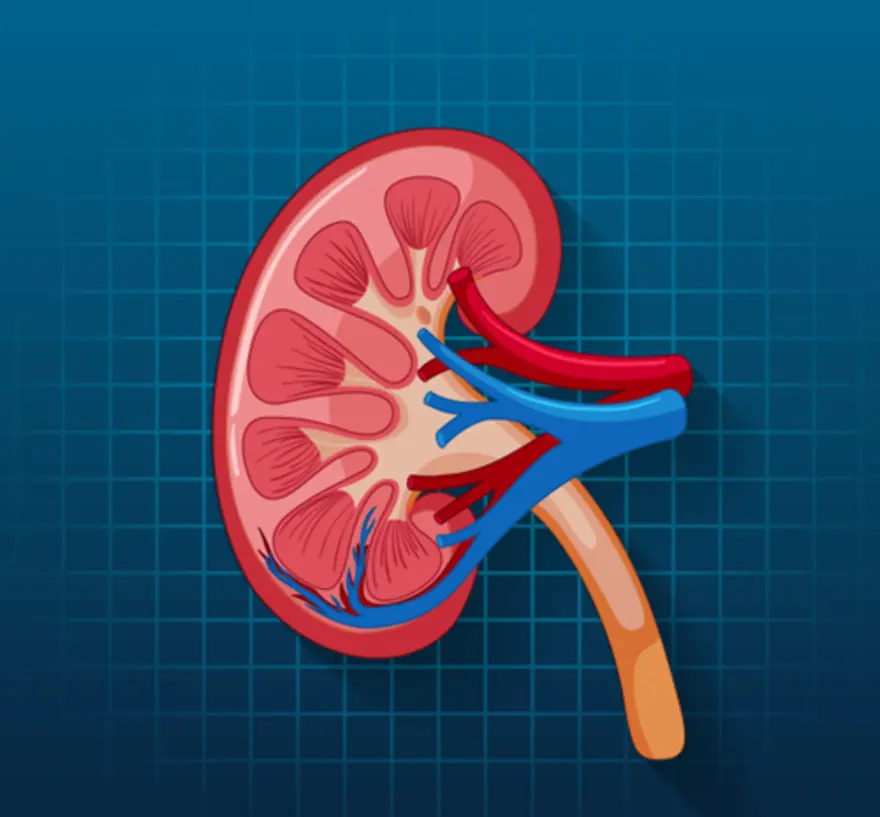
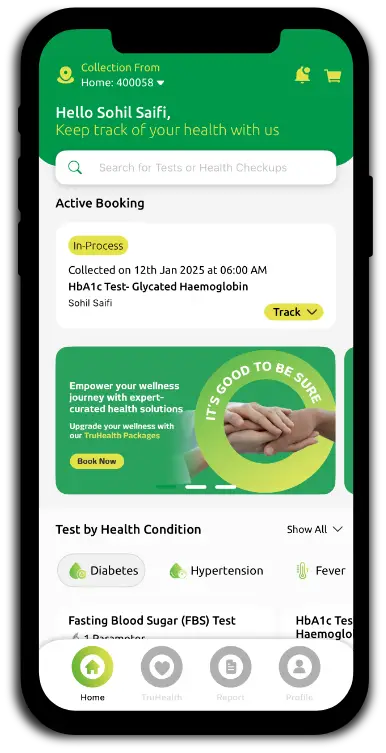
What are Kidney Cysts? A kidney cyst is a round, fluid-filled sac that forms on or within the kidney. It becomes increasingly common with age, affecting nearly half of adults over 50. Most are simple cysts with thin walls and clear fluid, which are benign and rarely cause problems. In contrast, complex cysts have thicker walls, internal septations, or solid components and may require closer monitoring or treatment depending on their size, location, and imaging features. Types of Kidney Cysts Understanding different kidney cyst types helps you recognise which ones might need medical attention: Simple kidney cysts: According to StatPearls (2023), simple renal cysts are the most common type, simple renal cysts are the most common type of kidney cyst, usually acquired rather than inherited. They affect about 25% of adults over 40 and nearly 50% over 50 and are typically asymptomatic. They are detected in imaging and require treatment if they grow large or become infected. Complex kidney cysts: These have thicker walls, internal separations, or solid areas. Complex cysts are classified using the Bosniak classification system, which stratifies cancer risk and guides management. Polycystic kidney disease (PKD) cysts: Multiple cysts caused by inherited genetic mutations. PKD can significantly impact kidney function and may lead to kidney disease over time. Acquired cystic kidney disease (ACKD) cysts: These develop in people with chronic kidney disease, particularly those on long-term dialysis treatment. What Causes Kidney Cysts? Understanding kidney cyst causes can help you better comprehend this condition, though many cases have no identifiable trigger: Age-related changes: The most common cause of kidney cysts is natural ageing. As you get older, your kidney tissue undergoes changes that may lead to cyst formation. Genetic factors: Inherited conditions, such as polycystic kidney disease, result from specific gene mutations that are passed down through families. Kidney disease complications: Chronic kidney disease and long-term dialysis can trigger acquired cystic kidney disease. Unknown factors: Many simple kidney cysts develop without any identifiable cause, making prevention challenging. Possible tubular blockage: Some researchers suggest that blockage of renal tubules may play a role in cyst formation, although this remains unproven. Symptoms of Kidney Cysts Most kidney cysts produce no symptoms, which is why they're often discovered accidentally during imaging tests for other conditions. However, when kidney cyst symptoms do occur, they typically include: Dull, aching pain: Persistent discomfort in your back, side, or upper abdomen may occur if cysts grow large enough to press against surrounding tissues or organs. Blood in urine: Also called haematuria, this symptom may indicate cyst rupture, infection, or other complications requiring immediate medical attention. Fever and chills: These signs suggest possible cyst infection, which needs prompt antibiotic treatment to prevent serious complications. Abdominal swelling: Large or multiple cysts can cause noticeable abdominal enlargement or tenderness when touched. High blood pressure: Rarely, kidney cysts can interfere with normal kidney function, leading to elevated blood pressure readings. When Kidney Cysts Are Usually Asymptomatic The vast majority of kidney cysts remain completely asymptomatic throughout a person's lifetime. Small, simple kidney cysts typically cause no discomfort, functional impairment, or health concerns. They're often discovered incidentally during imaging tests such as CT scans or ultrasounds performed for unrelated medical issues. Because most kidney cysts are asymptomatic, many people live with them for years without realising they exist. Only when cysts grow significantly large, become infected, rupture, or press against surrounding structures do they typically produce noticeable symptoms requiring medical intervention. Complications of Kidney Cysts While most kidney cysts remain harmless, several complications can occur: Cyst infection: Bacteria can infect kidney cysts, causing fever, pain, and requiring antibiotic treatment. Infected cysts may need drainage procedures. Cyst rupture: Large cysts can burst, causing sudden, severe pain and potential internal bleeding that might require emergency medical care. Pressure effects: Large cysts can compress nearby organs, blood vessels, or kidney tissue, potentially impairing kidney function. Urine flow obstruction: Strategically located cysts might block normal urine drainage, leading to kidney swelling and functional impairment. Blood pressure elevation: Some kidney cysts can interfere with blood pressure regulation, contributing to hypertension development. Cancer concerns: Though rare, complex kidney cysts may indicate or develop into kidney cancer, requiring careful monitoring and evaluation. How Kidney Cysts Are Diagnosed Healthcare providers use several diagnostic approaches to identify and evaluate kidney cysts: Medical history and physical examination: The doctor assesses symptoms and family history and performs a physical exam to check for abdominal tenderness or palpable masses. Ultrasound imaging: This painless, non-invasive test uses sound waves to create detailed kidney images, easily identifying cyst presence, size, and basic characteristics. CT scan: Computed tomography provides more detailed cross-sectional images, helping distinguish between simple and complex cysts while assessing internal structures. MRI scan: Magnetic resonance imaging provides exceptional soft-tissue detail, particularly useful for evaluating complex cysts or when CT results are unclear. Blood and urine tests: Laboratory tests assess overall kidney function and check for signs of infection, kidney disease, or other complications. Kidney Cyst Size and What It Means Kidney cysts vary dramatically in size, from microscopic formations to large masses several centimetres across. Small cysts under two centimetres rarely cause problems and typically require only periodic monitoring. Medium-sized cysts measuring 2-4 centimetres may cause occasional discomfort but are usually manageable with observation. Large cysts exceeding 4 centimetres are more likely to produce symptoms like abdominal pain, especially if they press against surrounding organs. However, size alone doesn't determine treatment necessity—your symptoms, cyst characteristics, and overall health status are equally important considerations in developing your management plan. Treatment for Kidney Cysts Most kidney cysts, especially simple and asymptomatic ones, don’t need treatment and are just monitored over time. Treatment is considered when cysts are complex or cause symptoms, with the approach tailored to factors like cyst type, size, your overall health, and long-term goals. Management of Simple Kidney Cysts Regular monitoring: Periodic ultrasound or CT scans track cyst growth and detect any concerning changes over time. Symptom management: Pain relievers and supportive care address occasional discomfort when it occurs. Watchful waiting: Most simple cysts remain stable for years, requiring no active treatment beyond routine observation. Lifestyle modifications: Maintaining good kidney health through proper hydration and healthy habits supports overall kidney function. Treatment for Complex Kidney Cysts Complex kidney cysts require more intensive evaluation and management: Detailed evaluation: Complex cysts are assessed with CT or MRI (using the Bosniak classification), along with kidney function tests such as serum Cystatin C, estimated GFR with creatinine, and a Kidney Function Test (KFT). Specialist review: Urologists decide on surveillance vs. intervention (cyst excision, partial nephrectomy, ablation) based on cancer risk, cyst size, and symptoms. Biopsy and pathology: When malignancy or another serious condition is suspected, kidney biopsy and histopathological evaluation (including immunofluorescence, if indicated) help confirm the diagnosis. Genetic testing (when indicated): In multiple cysts or a strong family history, genetic testing may be advised. Lifestyle Tips for Kidney Health Stay well-hydrated: Drink sufficient water daily to support kidney function and promote the elimination of waste products. Follow a balanced diet: Choose foods low in salt and processed ingredients, and avoid excessive protein intake to reduce kidney workload. Manage chronic conditions: Keep blood pressure and blood sugar levels within healthy ranges to prevent kidney damage. Avoid nephrotoxic substances: Limit overuse of nonsteroidal anti-inflammatory drugs (NSAIDs) and avoid excessive alcohol consumption, both of which can harm kidney tissue. Exercise regularly: Physical activity supports cardiovascular health and helps maintain healthy blood pressure levels. Avoid smoking: Tobacco use damages blood vessels and can worsen existing kidney problems. Kidney Cysts vs. Polycystic Kidney Disease (PKD) It's important to distinguish between simple kidney cysts and polycystic kidney disease. Simple kidney cysts are usually isolated, harmless formations that don't run in families or cause significant health problems. They typically remain stable throughout your lifetime without affecting kidney function. Polycystic kidney disease (PKD), however, is an inherited genetic disorder that causes multiple cysts in both kidneys. PKD can lead to kidney enlargement, reduced kidney function, and eventually kidney failure requiring dialysis or transplantation. PKD may also cause cysts in other organs such as the liver and is associated with complications including hypertension, chronic pain, and recurrent urinary tract infections. If you have a family history of PKD or multiple kidney cysts, genetic counselling and specialised testing may be recommended to determine your risk and develop appropriate monitoring strategies. When to See a Doctor Persistent abdominal pain: Ongoing discomfort in your back, side, or upper abdomen, especially if it worsens over time. Blood in urine: Any amount of visible blood in your urine requires prompt medical evaluation to rule out serious complications. Signs of infection: Fever, chills, or tenderness over your kidney area may indicate cyst infection requiring antibiotic treatment. Urination difficulties: Problems with urination, including decreased output or difficulty passing urine, need immediate assessment. Unexplained high blood pressure: New or worsening hypertension might be related to kidney cyst complications. Family history concerns: If you have relatives with polycystic kidney disease and develop symptoms, seek genetic counselling and screening. Conclusion Understanding kidney cysts empowers you to make informed decisions about your health. Most simple cysts are harmless and only require monitoring, whereas complex or symptomatic cysts need timely evaluation and appropriate care. Regular checkups, appropriate diagnostic tests, and a healthy lifestyle play a key role in protecting long-term kidney function. At Metropolis Healthcare, you can access 4,000+ tests, including specialised kidney profiles and full-body checkups, supported by accurate results, quick turnaround times, and strong home sample collection services across 4,600+ centres and 10,000+ touchpoints in India. With easy booking via website, call, app, or WhatsApp, Metropolis makes it convenient to stay proactive about your kidney health in partnership with your doctor. FAQs Are kidney cysts dangerous? Most kidney cysts, particularly simple ones, are not dangerous and rarely cause health problems. They're commonly discovered accidentally during imaging tests and typically require only periodic monitoring. However, complex cysts, infected cysts, or those associated with polycystic kidney disease may have health implications requiring medical evaluation and treatment. Can kidney cysts go away on their own? Simple kidney cysts generally do not disappear spontaneously. They typically remain stable in size or grow slowly over time. While cyst rupture can occasionally cause a cyst to resolve, this is uncommon and usually associated with pain or other symptoms requiring medical attention. Do kidney cysts cause back or side pain? Most kidney cysts don't cause pain, especially smaller ones. However, larger cysts or those that become infected, rupture, or press against surrounding organs can cause dull, aching pain in your back, side, or upper abdomen. If you experience persistent pain, consult your healthcare provider for proper evaluation. How fast do kidney cysts grow? Kidney cyst growth rates vary significantly between individuals. Simple cysts typically grow slowly over years, with some studies suggesting they may double in size over a decade. Rapid cyst growth should be evaluated promptly, as it might indicate complications or the need for closer monitoring. Can you prevent kidney cysts? There's no known way to prevent simple kidney cysts because their exact cause remains unclear. Maintaining overall kidney health through proper hydration, a balanced diet, blood pressure control, and avoiding nephrotoxic substances may support kidney function, but doesn't specifically prevent cyst formation. Do kidney cysts affect kidney function? Most simple kidney cysts don't affect kidney function. However, large or numerous cysts, or those associated with polycystic kidney disease, can impair kidney function by compressing healthy tissue or obstructing urine flow. Regular monitoring helps detect functional changes that require intervention. References https://www.ncbi.nlm.nih.gov/books/NBK499900/ https://my.clevelandclinic.org/health/diseases/15471-kidney-cysts https://medlineplus.gov/kidneycysts.html https://www.niddk.nih.gov/health-information/kidney-disease/kidney-cysts https://www.kidney.org/atoz/content/kidneycysts https://radiologyinfo.org/en/info/kidneycyst
Vascular Dementia: Causes, Symptoms, and Care Tips
What is Vascular Dementia? Vascular dementia refers to a decline in thinking and reasoning abilities caused by impaired blood flow in the brain’s vascular system. The brain relies on a constant oxygen supply; when arteries are narrowed, blocked, or damaged, neurons begin to die, leading to cognitive impairment. This condition often develops after a stroke, multiple transient ischemic attacks (TIAs), or chronic conditions like hypertension and diabetes. The term vascular dementia encompasses a spectrum of disorders, from mild vascular cognitive impairment to severe dementia affecting daily activities. How Vascular Dementia Differs from Alzheimer’s Although both diseases affect memory and cognitive abilities, their causes and progression differ significantly. Cause: Alzheimer’s disease is linked to abnormal protein deposits (amyloid and tau), whereas vascular dementia arises from blood vessel damage that disrupts oxygen supply to brain regions. Progression: Alzheimer’s progresses gradually, while vascular dementia often shows stepwise deterioration — periods of stability interrupted by sudden declines after vascular events. Symptoms: Alzheimer’s disease typically begins with memory loss, while vascular dementia initially presents as slowed thinking, poor focus, and executive dysfunction. Diagnosis: Brain imaging, such as CT scans or MRI scans, is vital to detect small strokes and vessel damage that confirm vascular origins. Recognising these distinctions helps guide appropriate treatment and prognosis. Types of Vascular Dementia (Including Vascular Cognitive Impairment) Vascular dementia can take multiple forms depending on which blood vessels and brain regions are affected: Multi-Infarct Dementia: Occurs after a series of small strokes (infarcts) that cumulatively damage brain tissue. Subcortical Vascular Dementia (Binswanger’s Disease): Involves chronic damage to small arteries deep within the brain, often linked to long-term hypertension. Post-Stroke Dementia: Develops after a major stroke that interrupts blood flow to large brain areas. Mixed Dementia: Features both vascular and Alzheimer-type brain changes. Vascular Cognitive Impairment (VCI): A milder form of the condition where memory and reasoning are affected, but full-blown dementia has not yet developed. Understanding the type of vascular dementia helps clinicians customise management and rehabilitation plans. Vascular Dementia Causes The primary cause of vascular dementia is reduced or blocked blood flow in brain arteries, resulting in ischemic injury. A National Institutes of Health (NIH) study in Cerebral Circulation – Cognition and Behaviour found that around 40% of India’s 5.3 million dementia cases are due to vascular causes, with poor control of hypertension, diabetes, and stroke care driving the rise. Researchers noted that better vascular risk management could potentially reduce dementia rates by up to 40%. Contributing mechanisms include: Blood clot in the brain, leading to stroke and localized damage. Atherosclerosis is the buildup of fatty deposits in the arteries, which restricts blood flow. Hypertension (high blood pressure) causes vessel thickening and rupture. Diabetes mellitus damages small vessels and accelerates atherosclerosis. Heart conditions such as atrial fibrillation increase the risk of clots travelling to the brain. Vasculitis or inflammation of blood vessels that disrupts circulation. Learn more about blood clots in the brain and how early detection can prevent cognitive decline. Vascular Dementia Risk Factors Certain lifestyle and medical conditions increase susceptibility to vascular dementia: Advanced age (over 65 years) History of stroke or TIA High blood pressure and cholesterol levels Diabetes and obesity Smoking and heavy alcohol consumption Atrial fibrillation or heart rhythm irregularities Family history of vascular disease or dementia Sedentary lifestyle and poor diet Addressing these modifiable risks early is key to reducing brain damage and preventing progression. Early Signs and Common Vascular Dementia Symptoms The symptoms of vascular dementia vary depending on which brain areas are affected, but generally include: Slower thinking and reduced attention span Short-term memory loss Sudden confusion or disorientation, especially post-stroke Difficulty with planning, decision-making, or multitasking Emotional instability, irritability, or apathy Trouble walking, loss of balance, or coordination issues Speech and language difficulties Visual perception changes Early identification of these symptoms is vital, as prompt treatment can prevent further vascular events and slow cognitive decline. Vascular Dementia Stages and Progression Vascular dementia usually progresses in distinct stages rather than a steady decline. Patients may experience sudden worsening after each vascular episode, followed by periods of relative stability. Mild Stage: Subtle memory problems, reduced concentration, and mild disorganisation. Moderate Stage: Noticeable confusion, slowed reasoning, and difficulty managing finances or medications. Severe Stage: Significant cognitive impairment, dependence on others, personality changes, and physical difficulties, such as incontinence or immobility. With each vascular event, brain tissue loss accumulates, resulting in a compounded cognitive decline. Diagnostic Tests and Imaging Techniques for Vascular Dementia Diagnosis involves a combination of neurological evaluation, imaging, and laboratory testing to identify vascular causes: CT Scan: Detects evidence of past strokes, haemorrhages, or vessel narrowing. MRI: Provides high-resolution images of brain structure and small vessel disease. Blood tests: Measure cholesterol, sugar, and clotting factors to detect underlying vascular conditions. Lumbar puncture: May help rule out infections or inflammatory brain disorders. Cognitive assessments: Evaluate attention, memory, and executive functions. Early and accurate diagnosis allows doctors to differentiate vascular dementia from other neurodegenerative diseases and design targeted interventions. When to Seek Medical Care for Vascular Dementia Symptoms? Consult a healthcare professional immediately if you notice: Sudden confusion or speech difficulties Weakness or numbness on one side of the body Trouble walking or maintaining balance Frequent mini-strokes or TIAs Rapid mood or personality shifts Early medical evaluation is essential to prevent recurrent strokes and irreversible brain injury. Vascular Dementia Treatment Overview There is no single cure for vascular dementia; treatments focus on stabilising vascular health and supporting cognitive function. Medications Used in Vascular Dementia Antihypertensive medications (ACE inhibitors, beta-blockers, or diuretics) to control blood pressure. Antiplatelet agents like aspirin or clopidogrel are used to prevent clot formation. Statins help manage cholesterol levels and reduce atherosclerotic plaque formation. Antidiabetic drugs to regulate blood sugar levels. Cholinesterase inhibitors and memantine, sometimes used off-label, are used to enhance cognitive function. Rehabilitation and Supportive Therapies Physical therapy to improve strength and balance. Occupational therapy to adapt home environments for safety. Speech therapy for language and communication challenges. Cognitive training and memory exercises. Psychological counselling to manage anxiety, depression, and caregiver burnout. These interventions not only support brain function but also promote emotional and physical well-being. Lifestyle & Self-Care to Support Brain and Vascular Health Daily habits can make a remarkable difference in slowing the disease’s progression: Maintain healthy blood pressure and glucose levels. Follow a Mediterranean-style diet rich in fish, nuts, olive oil, and whole grains. Engage in regular aerobic exercise such as brisk walking or cycling. Quit smoking and limit alcohol intake. Ensure adequate sleep and stress management. Stay mentally and socially active through hobbies, reading, and engaging conversations. These actions not only benefit the brain but also protect the heart — both of which share the same vascular system. Preventing or Lowering Risk of Vascular Dementia Control blood pressure through routine monitoring and medication as prescribed. Manage diabetes with dietary control and consistent treatment. Exercise regularly to enhance blood flow and oxygen delivery. Adopt a low-fat, low-sodium diet to reduce plaque buildup. Avoid tobacco and moderate alcohol intake. Treat heart rhythm disorders, such as atrial fibrillation, promptly. Undergo periodic brain imaging and health check-ups for early detection. Proactive prevention remains the strongest defence against cognitive decline. Caring for Someone with Vascular Dementia Caring for someone with vascular dementia requires patience, structure, and empathy: Establish consistent daily routines to minimise confusion. Use labels, notes, and reminders to aid memory. Keep the environment calm and clutter-free. Encourage socialisation and light physical activity. Attend support groups for caregivers. Seek professional help for home safety modifications and palliative planning when needed. Caregiver well-being is equally vital, as emotional strain can impact the health of both parties. Vascular Dementia Complications and Safety Concerns Unchecked vascular dementia can lead to: Frequent falls and injuries due to coordination issues. Swallowing difficulties that increase aspiration risk. Severe behavioural or mood disorders, such as aggression or depression. Complete dependency in daily tasks in the late stages. Vascular Dementia vs. Post-Stroke Cognitive Impairment While both conditions affect cognition after vascular injury, post-stroke impairment appears immediately after a stroke, whereas vascular dementia develops gradually after multiple small events. Continuous monitoring helps distinguish between the two. Is Vascular Dementia Hereditary? Vascular dementia is generally not hereditary, meaning it does not usually pass directly from parent to child. However, genetic predispositions to certain health conditions such as high blood pressure, diabetes, or high cholesterol can increase the likelihood of developing it. Ultimately, lifestyle factors such as diet, exercise, and smoking habits play a much greater role in determining risk. Prognosis and Life Expectancy in Vascular Dementia Prognosis varies depending on age, stroke frequency, and underlying medical conditions. On average, life expectancy ranges from 5 to 10 years after diagnosis, although patients who manage risk factors may live longer with a better quality of life. Continuous medical supervision, rehabilitation, and adherence to a healthy lifestyle are crucial for maintaining stability. Conclusion Vascular dementia reflects the deep connection between heart and brain health. Managing blood pressure, diabetes, and cholesterol, while embracing an active lifestyle, can dramatically reduce the risk. Metropolis Healthcare offers advanced diagnostic tools — including CT, MRI, and blood testing — to detect vascular conditions early. With 4000+ tests, NABL & CAP-accredited labs, home sample collection, 10,000+ touchpoints, and quick, accurate reporting, we help you take charge of your health with confidence and care. FAQs Can vascular dementia be reversed? Brain damage caused by a lack of blood flow cannot be reversed, but treatments can halt or slow further deterioration. How fast does vascular dementia progress? The disease progresses in steps, worsening after each new vascular incident, with intermittent plateaus. How is vascular dementia diagnosed? Neurological assessment and cognitive testing. CT or MRI imaging. Blood tests for cholesterol, sugar, and clotting profile. Additional procedures like lumbar puncture or EEG, if required. Is vascular dementia hereditary? Vascular dementia is not directly hereditary, but genetic factors linked to conditions such as hypertension, diabetes, and high cholesterol can raise the risk. Can lifestyle changes reduce the risk of vascular dementia? Yes — maintaining vascular health through exercise, a balanced diet, smoking cessation, and stress management significantly lowers the risk. What complications occur in late-stage vascular dementia? Loss of independence Difficulty swallowing and eating Incontinence and immobility Heightened infection risk Emotional withdrawal or aggression
Dialectical Behavior Therapy (DBT): Benefits, Techniques & Uses
What is Dialectical Behavior Therapy (DBT)? Dialectical Behavior Therapy (DBT) is a specialized form of Cognitive Behavioral Therapy (CBT) designed to help individuals manage intense emotions, reduce self-destructive behaviors, and improve interpersonal effectiveness. The word "dialectical" means combining opposites — DBT helps people balance acceptance and change simultaneously. In simple terms, when you define dialectical behavior therapy, it’s a structured therapy that teaches emotional awareness, distress tolerance, and healthy communication skills to improve overall mental well-being. History of DBT and Its Development DBT was developed in the 1980s by Dr. Marsha Linehan, a psychologist who noticed that traditional CBT techniques were not fully effective for patients with chronic emotional instability, particularly those with Borderline Personality Disorder. To address this, she integrated mindfulness and acceptance principles from Buddhist philosophy into CBT. Over the years, DBT has been adapted for a range of conditions including depression, anxiety disorders, PTSD, and eating disorders, showing consistent success across diverse populations. How DBT Works: The Core Principles Dialectical Behavior Therapy (DBT) is built on the idea of achieving balance — helping individuals accept their emotions while learning to change unhelpful behaviors. It rests on four key principles that work together to promote emotional stability and self-awareness: Dialectics: Encourages finding a middle path between acceptance and change, teaching that two seemingly opposite truths can coexist. Behavioral Approach: Focuses on identifying problematic behaviors, understanding their triggers, and replacing them with healthier responses. Validation: Helps individuals acknowledge and accept their feelings without judgment, reducing guilt and emotional conflict. Mindfulness: Cultivates awareness of the present moment, allowing better control over impulsive reactions and clearer decision-making. These principles make DBT a structured, compassionate, and practical therapy for managing distress and building lasting emotional resilience. Key DBT Techniques for Managing Emotions Dialectical Behavior Therapy (DBT) uses a set of structured techniques known as core skill modules to help individuals understand, tolerate, and regulate their emotions effectively. These techniques are practical and can be applied in daily life to improve emotional control and relationships: Mindfulness: Builds awareness of the present moment by focusing attention on thoughts, emotions, and surroundings without judgment. It helps reduce impulsive reactions and enhances clarity in decision-making. Distress Tolerance: Teaches coping strategies for handling crises without resorting to harmful behaviors. Techniques like deep breathing, grounding exercises, or self-soothing help manage intense stress safely. Emotion Regulation: Enables individuals to recognize emotional patterns, understand triggers, and apply healthy coping mechanisms to prevent emotional overwhelm. Interpersonal Effectiveness: Strengthens communication and assertiveness skills, helping individuals set healthy boundaries, express needs clearly, and maintain balanced relationships. The Benefits of DBT: Improving Mental Health Dialectical Behavior Therapy (DBT) offers comprehensive benefits that go beyond managing emotions — it helps individuals build lasting psychological strength and balance. By teaching skills in mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness, DBT enables people to respond thoughtfully rather than react impulsively. Clinical studies have shown DBT to be highly effective for depression, anxiety, PTSD, eating disorders, and Borderline Personality Disorder (BPD). It reduces emotional volatility, self-harming behaviors, and suicidal thoughts while improving self-esteem and relationship satisfaction. Patients often experience greater resilience, stability, and a renewed sense of control over their mental health. How DBT Can Help with Borderline Personality Disorder (BPD) According to a study published by the National Institutes of Health (NIH), Dialectical Behavior Therapy (DBT) is the only empirically supported treatment for Borderline Personality Disorder, significantly reducing self-harm, hospitalizations, and impulsive behaviors while improving outcomes for depression, PTSD, and eating disorders. By teaching mindfulness and interpersonal effectiveness, DBT helps individuals manage intense emotions, avoid self-destructive actions, and maintain long-term emotional stability. Clinical trials have shown that DBT can cut hospitalization rates by nearly half and significantly improve overall functioning among BPD patients. Who Can Benefit from DBT? While DBT is most known for treating BPD, it’s beneficial for anyone struggling with: Persistent depression or anxiety PTSD symptoms Eating disorders such as binge eating or bulimia Bipolar disorder or chronic emotional dysregulation Self-harming behaviors or suicidal ideation DBT in Practice: What to Expect in a Session A typical DBT program includes four key components: Individual Therapy: One-on-one sessions focused on applying DBT skills to personal challenges. Group Skills Training: Participants learn and practice DBT techniques like mindfulness and emotion regulation. Phone Coaching: Provides real-time support when clients face emotional crises between sessions. Therapist Consultation Teams: Ensure therapists maintain fidelity to DBT principles and support client progress. DBT vs. CBT: Key Differences Aspect DBT CBT Philosophy Balances acceptance and change Focuses primarily on change Approach Mindfulness and emotion-focused Cognition and behavior-focused Best For BPD, emotional dysregulation, impulsivity Depression, anxiety, negative thinking Structure Individual + group skills training Mostly individual sessions How Long Does DBT Take? DBT typically runs for six months to one year, depending on the severity of symptoms and treatment goals. Some individuals continue maintenance therapy or skills groups beyond the initial program to reinforce learned behaviors. DBT Group Therapy vs. Individual Therapy Group Therapy: Focuses on learning and practicing DBT skills collectively. It offers community support and accountability. Individual Therapy: Personalized sessions that address deeper emotional patterns and tailor DBT skills to the client’s life. Most comprehensive DBT programs combine both for maximum effectiveness. DBT for Adolescents: Is It Effective for Teens? Adolescents often experience strong emotions and impulsive behaviors. DBT for teens (DBT-A) adapts traditional techniques to help them handle academic pressure, peer influence, and family conflict. It has shown measurable improvement in reducing self-harm, improving communication, and managing anxiety and depression among teens. What Are the Challenges of DBT? While DBT offers profound benefits, it requires dedication. Clients must commit to homework exercises, daily diary cards, and active participation in sessions. The process can feel demanding initially, but persistence leads to life-changing emotional stability and healthier coping mechanisms. DBT Techniques You Can Try at Home You can begin integrating DBT-inspired habits into your daily routine with simple exercises: Mindful Breathing: Spend five minutes observing your breath to anchor yourself in the present. The STOP Skill: Stop, Take a step back, Observe, and Proceed mindfully. Self-Soothing: Engage your senses—listen to calming music or hold something comforting. Emotion Journal: Track emotions, triggers, and coping responses to build self-awareness. Conclusion Dialectical Behavior Therapy (DBT) empowers individuals to manage emotions, build resilience, and achieve emotional balance—especially for conditions like depression, anxiety, PTSD, BPD, and eating disorders. By integrating acceptance and change, DBT helps individuals regain control over their thoughts, relationships, and overall mental health. At Metropolis Healthcare, we support your journey toward wellness with 4000+ tests, comprehensive full-body checkups, and specialty diagnostics you can trust. Enjoy home sample collection across 10,000+ touchpoints, quick turnaround times, and accurate results — all bookable easily through our website, app, call, or WhatsApp. Because at Metropolis, we believe better care begins with better diagnosis. FAQs What is DBT and How Does It Work? DBT combines cognitive-behavioral strategies with mindfulness and acceptance to help people manage emotions and develop constructive coping behaviors. Who is DBT Suitable For? DBT is effective for people dealing with BPD, PTSD, depression, anxiety, and eating disorders, or anyone struggling to regulate emotions. How Effective is DBT for BPD? Research shows DBT reduces suicidal behaviors by up to 50% and improves emotional regulation and interpersonal functioning. What is the DBT Skills Group? It’s a structured group setting where participants learn mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness. How Much Does DBT Therapy Cost? Costs vary based on location and therapist credentials. Some clinics offer sliding-scale fees or insurance coverage. Can I Do DBT Online? Yes. Many certified therapists and mental health platforms offer virtual DBT sessions that mirror in-person training. Is DBT Covered by Insurance? Coverage depends on individual insurance policies and the therapist’s network status. Always confirm before starting therapy.
Tricuspid Atresia: Causes, Symptoms & Treatment
What is Tricuspid Atresia? Tricuspid atresia is a congenital heart defect where the tricuspid valve, which controls blood flow between the right atrium and right ventricle, is either missing or undeveloped. This leads to inadequate oxygenation since blood cannot flow properly through the right side of the heart to the lungs. According to the National Institutes of Health (NIH), tricuspid atresia occurs in approximately 1.2 per 10,000 live births and is the third most common cyanotic heart defect. Without early surgery, it has a high mortality rate, though survival after treatment reaches over 80% at one year. Infants born with this condition depend on alternative pathways, such as a patent foramen ovale or ventricular septal defect (VSD), to circulate blood. Early detection and timely surgical intervention are crucial for survival. Causes of Tricuspid Atresia The exact cause of tricuspid atresia is not fully known, but it results from abnormal development of the tricuspid valve during early fetal growth, unrelated to maternal behavior or lifestyle. Genetic or chromosomal abnormalities: Certain mutations or chromosomal defects, such as Down syndrome or 22q11 deletion, may disrupt the genes responsible for heart valve formation, leading to structural defects. Maternal diabetes or rubella infection: Poorly controlled diabetes or rubella virus infection during early pregnancy can interfere with the normal development of the fetal heart and blood vessels. Exposure to certain medications or toxins: Some prescription drugs, alcohol, or environmental toxins during the first trimester may harm fetal cardiac tissue, increasing the risk of congenital defects. Family history of congenital heart disease: Parents or siblings with congenital heart defects slightly raise the likelihood of tricuspid atresia, though most cases occur sporadically without inheritance. Genetic Factors and Inheritance While most cases of tricuspid atresia occur sporadically, certain genetic factors may contribute to its development. Chromosomal anomalies: Conditions such as Down syndrome (trisomy 21) or 22q11 deletion syndrome have been occasionally associated with tricuspid atresia due to disruptions in cardiac morphogenesis. Single-gene mutations: Rare mutations in heart development genes like NKX2-5 and GATA4 can interfere with normal valve formation and chamber differentiation. Familial recurrence: Though uncommon, some families show an autosomal recessive pattern, suggesting a low but possible hereditary component. Genetic counseling: Families with a history of congenital heart disease may benefit from prenatal screening and counseling to evaluate recurrence risks and plan early intervention. Symptoms of Tricuspid Atresia Symptoms of tricuspid atresia usually appear soon after birth, as the defect prevents proper blood flow between the right atrium and ventricle, leading to low oxygen levels in the body. The severity and timing of symptoms depend on the degree of pulmonary obstruction and the presence of other associated heart defects. Early recognition of these signs is crucial, as timely diagnosis and medical intervention can significantly improve survival and quality of life. Common Symptoms in Infants and Children Bluish skin tone (cyanosis): Caused by low oxygen levels in the blood, often noticeable on lips and fingertips. Fatigue or shortness of breath: Infants tire easily during feeding or crying due to reduced oxygen delivery. Poor weight gain or delayed growth: Inadequate oxygen and energy cause slower physical development. Rapid breathing and fast heartbeat: The heart and lungs work harder to maintain oxygen supply. Clubbing of fingers: Long-term low oxygen levels cause thickened fingertips. In some cases, a heart murmur may be heard during a routine examination, leading to further diagnostic testing. Diagnosis of Tricuspid Atresia Diagnosing tricuspid atresia is vital for early detection and timely surgical intervention, as the condition can quickly lead to life-threatening oxygen deprivation in newborns. The process begins with clinical observation of symptoms such as cyanosis, rapid breathing, or poor feeding, which alert doctors to a possible congenital heart defect. Once suspected, non-invasive imaging tests like echocardiography are performed to confirm the absence or underdevelopment of the tricuspid valve and to assess how blood flows through the heart. Supporting investigations, including pulse oximetry, chest X-ray, MRI, CT scan, and occasionally cardiac catheterization, help determine the severity of the defect and guide treatment planning. Early and accurate diagnosis ensures better surgical outcomes and improved long-term survival for affected infants. Diagnostic Tests and Imaging Techniques for Tricuspid Atresia Accurate diagnosis relies on a combination of non-invasive and imaging tests to assess heart structure, blood flow, and oxygen levels. Echocardiogram: The key diagnostic test that confirms the absence or underdevelopment of the tricuspid valve and evaluates blood movement between heart chambers. Pulse oximetry: A simple bedside test that measures oxygen saturation; persistently low levels suggest cyanosis. Chest X-ray: Reveals heart enlargement or abnormal lung blood flow patterns indicative of congenital defects. MRI: Offers high-resolution images of heart anatomy and function, aiding in surgical and treatment planning. CT scan: Produces 3D visualizations of the heart and major vessels to map structural abnormalities before surgery. Electrocardiogram (ECG) and cardiac catheterization: Used when needed to measure electrical activity, pressure, and oxygen content inside heart chambers. Treatment Options for Tricuspid Atresia There is no definitive medical cure for tricuspid atresia; treatment focuses on surgical correction to ensure proper blood circulation and oxygen delivery. Before surgery, doctors may administer prostaglandin E1 to keep the ductus arteriosus open, allowing temporary blood flow to the lungs. Surgical Treatment: The Fontan Circulation The Fontan circulation is the definitive surgery for tricuspid atresia, performed in three stages to redirect blood flow and ensure oxygen-rich circulation. Stage 1 – Shunt procedure (newborn stage): A Blalock–Taussig shunt connects an artery to the lungs, improving oxygen supply. Stage 2 – Glenn procedure (around 4–6 months): The superior vena cava is connected to the pulmonary artery, sending upper body blood directly to the lungs. Stage 3 – Fontan Circulation (2–4 years): The inferior vena cava is routed to the pulmonary arteries, completing the separation of oxygen-poor and oxygen-rich blood. This staged approach allows the left ventricle to function as the main pumping chamber, improving oxygen levels and overall heart efficiency. Post-Surgery Care and Follow-Up After the Fontan circulation, patients need ongoing medical supervision to ensure the heart adapts well and complications are prevented. Hospital recovery: Continuous monitoring of oxygen levels, heart rhythm, and fluid balance is done immediately after surgery. Medications: Blood thinners, diuretics, or heart rhythm drugs may be prescribed to support circulation and prevent clots. Regular check-ups: Routine echocardiograms, MRIs, or pulse oximetry tests track heart function and oxygen flow. Infection prevention: Good hygiene and antibiotic prophylaxis before dental or surgical procedures help prevent endocarditis. Long-term follow-up: Lifelong care with a cardiologist specializing in congenital heart disease is essential for monitoring Fontan circulation and maintaining overall heart health. Lifestyle Adjustments and Prognosis With timely surgical treatment and regular medical follow-up, most children with tricuspid atresia can lead active and fulfilling lives. However, lifelong cardiac care is essential to monitor heart function and prevent complications. Physical activity: Light to moderate exercises are encouraged, but strenuous sports should be avoided to reduce heart strain. Diet and nutrition: A balanced, heart-healthy diet rich in fruits, vegetables, and lean proteins supports overall cardiovascular health. Regular follow-ups: Routine visits to a cardiologist help track heart rhythm, oxygen levels, and surgical outcomes through tests like echocardiograms or MRIs. Infection prevention: Good dental hygiene and antibiotic prophylaxis before certain procedures reduce the risk of endocarditis. Vaccinations: Staying up to date with influenza and pneumococcal vaccines protects against infections that could stress the heart. Living with Tricuspid Atresia: Long-Term Care People with tricuspid atresia need lifelong follow-up to maintain heart health and manage post-surgical outcomes effectively. Regular heart evaluations: Periodic echocardiograms, MRI, or CT scans monitor heart function and detect early issues. Medication management: Some patients require anticoagulants or diuretics to support blood flow and prevent complications. Symptom awareness: Persistent fatigue, swelling, or irregular heartbeat should be promptly reported to a cardiologist. Healthy lifestyle: A balanced diet, moderate physical activity, and emotional support improve overall well-being. Specialized care transition: Continued follow-up with an adult congenital heart disease specialist ensures long-term stability and quality of life. Conclusion Tricuspid atresia, though complex, is manageable with early diagnosis, modern imaging, and staged surgery. With continuous care and medical monitoring, children born with this condition can lead fulfilling lives. At Metropolis Healthcare, our advanced diagnostic infrastructure — including Echocardiogram, MRI, CT scans, Pulse Oximetry, and Chest X-ray — ensures accurate evaluation and reliable results. With 4000+ tests, home sample collection across 10,000 touchpoints, quick turnaround times, and expert cardiology support, we help you make timely, informed health decisions for your loved ones. FAQs What are the first signs of Tricuspid Atresia? Bluish skin, difficulty feeding, and poor growth soon after birth are early warning signs that warrant immediate medical evaluation. Can Tricuspid Atresia be treated without surgery? No. While medications stabilize oxygen levels, surgery is essential to restore effective circulation and prevent fatal complications. What is the life expectancy for someone with Tricuspid Atresia? With modern surgical care, over 80% of children survive into adulthood, though long-term complications may require lifelong monitoring. Is Tricuspid Atresia hereditary? Most cases are sporadic, but some involve genetic links. Families with a history of congenital heart disease should seek genetic counseling. Can Tricuspid Atresia be detected before birth? Yes. Fetal echocardiogram during pregnancy can detect structural heart defects like tricuspid atresia as early as the second trimester.