Preventive Healthcare
Male Reproductive System: Understanding Structure & Function
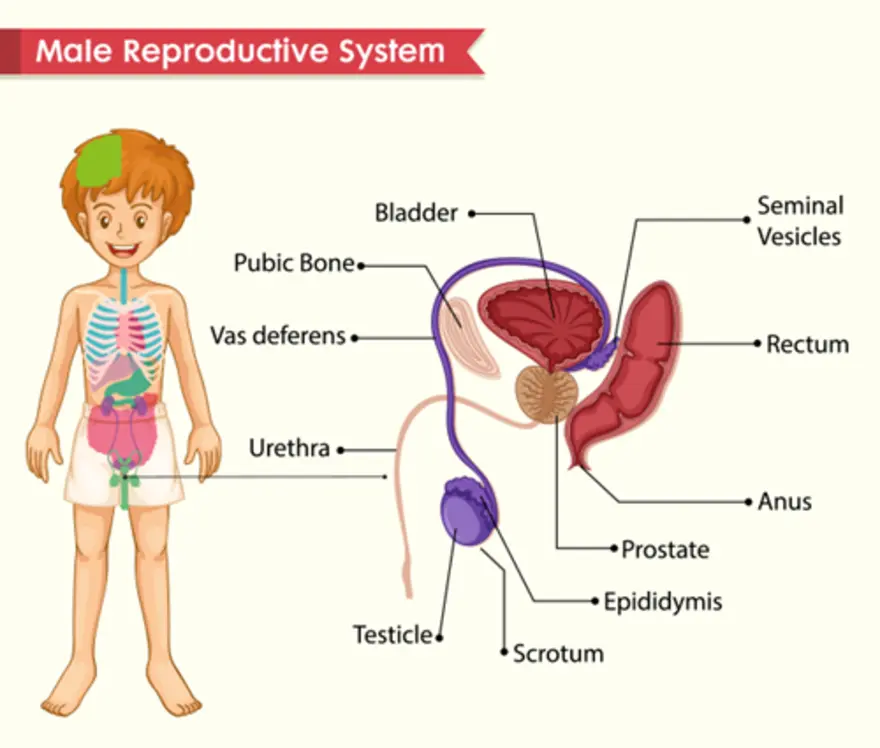
Table of Contents
- What is the Male Reproductive System?
- Anatomy of the Male Reproductive System
- Male Reproductive Health: Common Conditions and Disorders
- Impact of Age on Male Reproductive Health
- Male Reproductive System and Fertility
- Diagnostic Tests for Male Reproductive Health
- Healthy Lifestyle and Male Reproductive Health
- Conclusion
- FAQs
- References
What is the Male Reproductive System?
The male reproductive system consists of both external and internal organs that work together to produce, store, and transport sperm while manufacturing essential hormones like testosterone. This intricate system enables reproduction, supports sexual function, and influences the development of male characteristics throughout life.
The reproductive system begins developing before birth and continues maturing through puberty. During adolescence, hormonal changes activate sperm production and trigger the development of secondary sexual characteristics such as facial hair, a deeper voice, and increased muscle mass. Throughout adulthood, the male reproductive system functions continuously, producing millions of sperm daily and maintaining hormone levels essential for health and vitality.
Anatomy of the Male Reproductive System
External structures:
- Testes (testicles)
- Scrotum
- Penis
Internal structures:
- Epididymis
- Vas deferens
- Seminal vesicles
- Prostate gland
- Bulbourethral glands
- Urethra
The Male Reproductive Organs: Roles and Structure
Each component of the male reproductive system serves specific functions essential to reproduction and hormone production. The testes serve as the primary reproductive organs, producing sperm and the hormone testosterone. Meanwhile, the duct system transports sperm from the testes during arousal, while accessory glands contribute vital fluids that nourish and protect sperm during their journey.
The external positioning of the testes within the scrotum maintains optimal temperature for sperm production, approximately 2-3°C below normal body temperature. This intricate design ensures maximum fertility potential while protecting these delicate organs from injury.
Testes: The Core of Male Reproduction
The testes are oval-shaped glands housed within the scrotum, serving as the primary organs of the male reproductive system. They perform two vital male reproductive system functions: producing sperm through a process called spermatogenesis and manufacturing testosterone, the primary male hormone. Each testis contains hundreds of tightly coiled seminiferous tubules where sperm develop over approximately 74 days.
Within the testes, specialized cells called Leydig cells produce testosterone, which influences everything from muscle development to mood regulation. The testes also contain Sertoli cells that nourish developing sperm and help regulate their maturation. The testes respond to hormonal signals from the brain, adjusting sperm and hormone production according to the body's needs and external factors such as stress, nutrition, and sleep.
Scrotum: Temperature Control and Protection
- Temperature regulation: Contracts in cold conditions to bring the testes closer to the body for warmth
- Heat dissipation: Relaxes in warm conditions to move testes away from body heat
- Physical protection: Provides cushioning and shock absorption during daily activities
- Muscle coordination: Contains cremaster and dartos muscles that automatically adjust positioning
The Penis: Pathway for Sperm and Sexual Function
- Sperm delivery: Deposits sperm into the female reproductive system during intercourse
- Urinary function: Allows urine passage from the bladder through the urethra
- Erectile capability: Contains three columns of erectile tissue, enabling sexual function
- Sensory function: Houses nerve endings that contribute to sexual pleasure and reproductive success
Prostate Gland: Support for Sperm and Seminal Fluid
- Fluid production: Manufactures approximately 30% of the seminal fluid volume
- Sperm nourishment: Provides nutrients and enzymes that support sperm survival
- pH regulation: Maintains an optimal alkaline environment for sperm mobility
- Ejaculation assistance: Contains smooth muscle fibres that aid in semen expulsion
Seminal Vesicles: Creating the Seminal Fluid
- Major fluid contributor: Produces up to 60-70% of total semen volume
- Energy provision: Secretes fructose-rich fluid that fuels sperm movement
- Chemical protection: Adds substances that neutralise the acidic vaginal environment
- Sperm activation: Contains proteins that enhance sperm motility and fertilization capacity
Hormonal Regulation of Male Reproduction
The male reproductive system operates under precise hormonal control, orchestrated by the hypothalamic-pituitary-gonadal axis. The hypothalamus releases gonadotropin-releasing hormone (GnRH), which stimulates the pituitary gland to secrete luteinizing hormone (LH) and follicle-stimulating hormone (FSH). LH triggers testosterone production in the testes, while FSH promotes sperm development.
This hormonal feedback system maintains a delicate balance, adjusting hormone levels in response to the body's needs. Disruptions to this system can significantly impact male reproductive system functions, affecting fertility, sexual function, and overall masculine health.
Male Reproductive Health: Common Conditions and Disorders
- Erectile dysfunction: Difficulty achieving or maintaining erections
- Male infertility: Reduced ability to father children naturally
- Low testosterone: Decreased hormone production affecting multiple body systems
- Prostate disorders: Including enlargement, inflammation, and cancer
- Testicular problems: Such as cancer, torsion, or undescended testes
- Sexually transmitted infections: Affecting various parts of the reproductive system
- Varicocele: Enlarged veins within the scrotum affecting blood flow
Erectile Dysfunction: Causes and Treatment
Erectile dysfunction affects millions of men worldwide and can significantly impact quality of life. This condition can result from physical factors like cardiovascular disease, diabetes, or neurological disorders, as well as psychological factors including stress, anxiety, or depression. Physical causes often involve blood flow problems, nerve damage, or hormonal imbalances that affect the complex process of achieving an erection.
Treatment approaches vary depending on underlying causes but may include lifestyle modifications, oral medications, hormone therapy, or psychological counselling. Many men find that addressing underlying health conditions like diabetes or high blood pressure improves erectile function.
Male Infertility: Causes, Diagnosis, and Treatment
Causes:
- Low sperm count or poor sperm motility and morphology
- Blockages in the reproductive tract (e.g., vas deferens obstruction)
- Hormonal imbalances (e.g., low testosterone, thyroid issues)
- Genetic conditions (e.g., Klinefelter syndrome, Y chromosome microdeletions)
- Environmental exposures (e.g., toxins, radiation) and lifestyle factors (e.g., smoking, alcohol, obesity, stress)
- Chronic illnesses or infections affecting reproductive organs
Diagnosis:
- Comprehensive semen analysis to evaluate sperm count, motility, and morphology
- Hormone testing (e.g., Testosterone Free Test, Follicle-Stimulating Hormone (FSH) Test - Serum, FSH LH Testosterone Profile Test or FSH LH Prolactin Serum Test)
- Physical examination and detailed medical history
- Genetic screening if congenital or hereditary causes are suspected
- Imaging studies (e.g., scrotal ultrasound, MRI) to detect structural or anatomical issues
- Specialised tests for sperm function
Treatment:
- Lifestyle modifications (e.g., weight management, quitting smoking, reducing alcohol)
- Medications to correct hormonal imbalances or treat infections
- Surgical interventions to remove blockages or repair varicoceles
- Use of donor sperm in cases of severe male factor infertility
- Counselling and support for emotional and psychological aspects of infertility
Low Testosterone: Symptoms and Management
Common symptoms:
- Persistent fatigue and reduced energy levels
- Decreased libido and sexual function
- Loss of muscle mass and increased body fat
- Mood changes, including depression and irritability
- Difficulty concentrating and memory problems
Management strategies:
- Testosterone replacement therapy when appropriate
- Treatment of underlying medical conditions
- Regular exercise and strength training
- Healthy diet and weight management
- Adequate sleep and stress reduction
Impact of Age on Male Reproductive Health
Aging gradually affects the male reproductive system, though men can remain fertile much longer than women. According to the NHS, testosterone levels typically begin declining around age 30 to 40, dropping approximately 1% annually. This gradual decrease can affect energy, muscle mass, bone density, and sexual function over time.
Sperm quality also changes with age, with older men showing decreased sperm concentration and motility and increased DNA fragmentation. Research indicates that while men can father children into their 80s, advanced paternal age is associated with increased risks of genetic abnormalities and pregnancy complications.
Male Reproductive System and Fertility
- Sperm production: Healthy testes producing adequate numbers of viable sperm
- Sperm transport: Unobstructed pathways allowing sperm movement through the reproductive system
- Sperm quality: Normal sperm concentration, motility, and morphology
- Hormonal balance: Optimal testosterone and other hormone levels supporting reproduction
- Sexual function: Ability to achieve an erection and ejaculation for successful conception
Diagnostic Tests for Male Reproductive Health
- Semen analysis: Evaluates sperm count, motility, morphology, and volume
- Hormone testing: Measures testosterone, FSH, LH, and other reproductive hormones
- Physical examination: Assesses external reproductive organs for abnormalities
- Ultrasound imaging: visualizes internal structures and identifies blockages or masses
- Genetic testing: Identifies chromosomal abnormalities affecting fertility
- Specialised tests: Including sperm DNA fragmentation analysis and anti-sperm antibody testing
Healthy Lifestyle and Male Reproductive Health
- Balanced nutrition: Consuming antioxidant-rich foods, healthy fats, and adequate protein
- Regular exercise: Maintaining a healthy weight while avoiding excessive endurance training
- Stress management: Practicing practicing relaxation techniques and maintaining work-life balance
- Adequate sleep: Ensuring 7-9 hours of quality sleep nightly for optimal hormone production
- Avoiding toxins: Limiting exposure to chemicals, heavy metals, and environmental pollutants
- Substance avoidance: Limiting alcohol consumption and avoiding tobacco and recreational drugs
Preventing Male Reproductive Health Problems
Prevention remains the most effective approach to maintaining healthy male reproductive system functions throughout life. This includes attending regular medical check-ups, practicing safe sex to prevent sexually transmitted infections, and maintaining open communication with doctors about concerns or changes. Men should be aware of warning signs like changes in sexual function, testicular lumps or pain, urinary difficulties, or unusual discharge.
Maintaining a healthy lifestyle supports all aspects of reproductive function. This includes eating nutritious foods, exercising regularly, managing stress effectively, and avoiding harmful substances. Men working in environments with chemical exposure or extreme temperatures should take appropriate precautions to protect their reproductive health.
Male Reproductive Health and Mental Well-Being
Mental health significantly impacts reproductive function, creating connections between psychological and physical well-being. Chronic stress elevates cortisol levels, which can suppress testosterone production and reduce sperm quality. Depression and anxiety often correlate with decreased libido and sexual dysfunction, creating cycles where reproductive concerns worsen mental health symptoms.
Addressing mental health concerns through stress management techniques, counselling, and appropriate treatment for anxiety or depression can improve both psychological and physical aspects of reproductive health.
Conclusion
Understanding the male reproductive system empowers men to take charge of their health and make informed decisions about their well-being. From the intricate anatomy of male reproductive system components to the complex hormonal processes that regulate function, each element plays a vital role in overall health. The key to reproductive wellness lies in combining healthy lifestyle choices with regular medical care. By maintaining a healthy diet, exercising regularly, managing stress, and avoiding harmful substances, you can support your reproductive system throughout life.
At Metropolis Healthcare, we understand the importance of a comprehensive reproductive health assessment. Our extensive portfolio of over 4,000 advanced diagnostic tests includes specialised panels for hormone evaluation, fertility assessment, and reproductive health screening. Through our network of 220+ laboratories and 10,000+ touchpoints across India, we provide convenient at-home sample collection services, ensuring comfort and privacy for your health concerns.
FAQs
What are the main functions of the male reproductive system?
The primary male reproductive system functions include producing and storing sperm, manufacturing hormones like testosterone, enabling sexual intercourse, and facilitating reproduction through sperm delivery to the female reproductive system.
What are the common health issues in the male reproductive system?
Common issues include erectile dysfunction, infertility, low testosterone, prostate problems, testicular disorders, sexually transmitted infections, and age-related changes affecting reproductive function and overall health.
How does age affect male fertility?
Ageing gradually reduces testosterone production, decreases sperm quality and quantity, increases genetic abnormalities in sperm, and may cause erectile dysfunction, though fertility typically continues throughout life.
What hormones are involved in the male reproductive system?
Key hormones include testosterone (primary male hormone), luteinizing hormone (LH), follicle-stimulating hormone (FSH), and gonadotropin-releasing hormone (GnRH), all working together to regulate reproductive function.
Can male infertility be treated?
Yes, many causes of male infertility respond well to treatment through lifestyle changes, medications, surgical procedures, or assisted reproductive technologies, depending on underlying causes.
What lifestyle changes can improve male reproductive health?
- Maintain a healthy weight through balanced nutrition and regular exercise
- Avoid smoking, excessive alcohol, and recreational drugs
- Manage stress through practicing relaxation techniques and adequate sleep
- Limit exposure to environmental toxins and excessive heat
- Practice safe sex and maintain good hygiene
When should I see a doctor for male reproductive issues?
Consult a doctor for persistent erectile dysfunction, fertility concerns, testicular pain or lumps, urinary symptoms, hormonal changes, or any reproductive health concerns affecting your well-being.
References
- https://www.ncbi.nlm.nih.gov/books/NBK562253/
- https://www.urologyhealth.org/urology-a-z/e/erectile-dysfunction-(ed)
- https://www.nhs.uk/conditions/male-menopause/
- https://www.niddk.nih.gov/health-information/urologic-diseases/erectile-dysfunction/symptoms-causes




























