Preventive Healthcare
Brain MRI: What It Detects, Procedure and Report Terms

Table of Contents
- What Is a Brain MRI?
- What Can a Brain MRI Detect?
- When Is a Head MRI Recommended?
- Head MRI vs CT Scan: What Is the Difference?
- Head MRI With Contrast: What It Means
- How to Prepare for a Head MRI
- What Happens During the Scan?
- After the Scan: What to Expect
- Common Head MRI Report Terms and What They Usually Mean
- MRI Safety and Risks
- Frequently Asked Questions
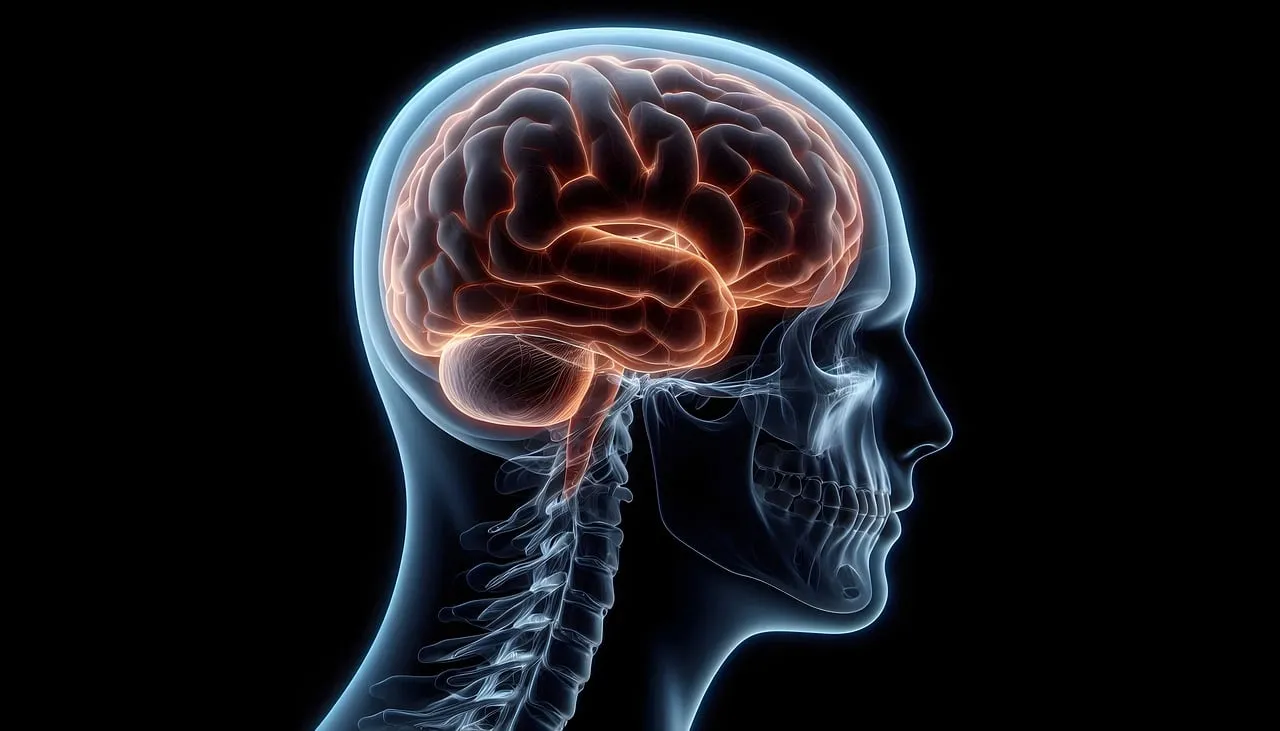
A head MRI, also called a brain MRI, is one of the most common scans used to look closely at the brain and nearby structures. People often search for “MRI head” when they have symptoms like headaches that will not settle, dizziness, seizures, changes in vision, memory concerns, or unexplained weakness. The idea of lying inside a scanner can feel intimidating, especially if you have never had imaging before.
The good news is that a head MRI is painless and does not use radiation. It uses a strong magnet and radio waves to create detailed pictures of soft tissues, which helps clinicians understand what is happening and what to do next.
This guide explains what a head MRI can detect, how to prepare, what happens during the scan, what “contrast” means, and how to make sense of common MRI report terms.
Medical note: This article is for general education and does not replace medical advice. Always discuss your results and next steps with your clinician.
What Is a Brain MRI?
A head MRI (Magnetic Resonance Imaging) is a scan that creates detailed images of the brain and surrounding tissues using a powerful magnet, radio waves, and a computer. It is often called a brain MRI, and in day-to-day practice the terms are usually used interchangeably.
Unlike X-rays and CT scans, an MRI does not use ionizing radiation. That makes it a preferred option in many situations where detailed soft-tissue imaging is important.
What Can a Brain MRI Detect?
A head MRI can help clinicians look for changes in the brain’s structure, blood flow patterns, and surrounding tissues. It may be used to detect or assess:
- Stroke-related changes, including early stroke changes in certain MRI sequences
- Bleeding, swelling, or fluid build-up
- Tumours or other masses
- Inflammation and some infections
- Conditions that affect the brain’s white matter, including demyelinating disorders such as multiple sclerosis
- Structural abnormalities, including developmental changes
- Pituitary gland issues and nearby structures (in dedicated pituitary MRI studies)
- Causes of seizures, depending on the clinical context
- Inner ear and eye-related structures (in some protocols), plus cranial nerves
A head MRI can also be used to monitor known conditions over time, such as changes after treatment, stability of lesions, or follow-up for ongoing symptoms.
When Is a Head MRI Recommended?
A clinician may suggest an MRI head scan when symptoms need deeper evaluation, for example:
- Persistent or unusual headaches, especially with additional symptoms
- Seizures or unexplained fainting episodes
- Dizziness or balance problems that are ongoing or severe
- Sudden changes in vision, hearing, or speech
- New weakness, numbness, or coordination changes
- Memory or thinking changes that need further assessment
- Symptoms after head injury, depending on the situation and timing
- Hormonal symptoms when pituitary involvement is suspected
In emergencies, CT is sometimes used first because it is faster and widely available. MRI is often used next, or when more detail is needed.
Head MRI vs CT Scan: What Is the Difference?
Both CT and MRI can image the brain, but they do it differently.
- CT scans use X-rays. They are fast and helpful in many emergency settings.
- MRI scans use magnets and radio waves. They usually take longer but provide more detailed views of brain soft tissue.
Your clinician chooses the test based on symptoms, urgency, and the question they are trying to answer.
Head MRI With Contrast: What It Means
Some brain MRI exams are done “with contrast.” This means a contrast agent, commonly a gadolinium-based dye, is injected into a vein during the scan to help certain tissues show up more clearly.
Contrast can improve the visibility of:
- Some tumours and patterns of inflammation
- Certain infections
- Blood vessels and areas of abnormal blood supply
- Specific changes after stroke (depending on timing and protocol)
Not every MRI needs contrast. Many are done without it, and your clinician or radiology team decides based on your symptoms and the best imaging approach.
Important safety note: If you have kidney disease, have had a previous reaction to contrast, or are pregnant or might be pregnant, tell your clinician and the MRI staff before the scan. They can decide what is safest for you.
How to Prepare for a Head MRI
Preparation is usually simple, but the safety checklist matters.
Before You Arrive
- Follow instructions from the imaging centre, especially if contrast is planned. Some centres may ask you to avoid eating for a few hours beforehand.
- Take your regular medications unless your clinician advises otherwise.
- Wear comfortable clothing. You may be asked to change into a gown.
Remove Metal and Mention Implants
MRI magnets are strong, so you must remove metal items such as:
- Jewellery, watches, hairpins, and belts
- Credit cards and phones (they can be damaged)
- Removable dental items, hearing aids, and some wearable devices
Tell the team if you have any implants or metal in your body, such as:
- Pacemaker or implanted defibrillator
- Cochlear implant
- Aneurysm clip
- Metal fragments from past injuries or work exposures
- Implanted pumps or stimulators
- Some types of surgical hardware
Many implants are MRI-safe or MRI-conditional, but the team needs details to confirm safety.
If You Have Claustrophobia
If enclosed spaces make you anxious, you are not alone. Options may include:
- A mild sedative prescribed in advance
- A wide-bore or open MRI machine if available
- Practical tips like closing your eyes, focusing on breathing, or listening to music through headphones
If sedation is used, you may need someone to accompany you home.
What Happens During the Scan?
A head MRI is usually painless, but it requires stillness and patience.
Step by Step
- You lie on a table that slides into the MRI scanner.
- A “head coil” is positioned around your head, like a helmet frame, to help capture clear images.
- The scan begins. You will hear loud tapping, knocking, or humming sounds in short sequences. Earplugs or headphones are provided.
- You must stay very still. Even small movements can blur images.
- If contrast is needed, an IV is used to inject it during the scan.
How Long It Takes
Most brain MRI scans take about 30 to 60 minutes, sometimes longer depending on the protocol and whether contrast is used.
What You Might Feel
- No pain from the scan itself
- The table may feel firm or cool (you can request a blanket in many centres)
- Some people feel warm in the scanned area
- If contrast is given, a brief cool sensation in the arm is common, and some people notice a temporary metallic taste
After the Scan: What to Expect
If you did not receive sedation, you can usually:
- Eat and drink normally
- Resume normal activities right away
If you received a sedative, you may need:
- A short recovery period
- Someone to drive you home
- Instructions about resting for the remainder of the day
A radiologist reviews the images and sends a report to the clinician who ordered the scan. The timeline varies, but many reports are available within a day or two.
Common Head MRI Report Terms and What They Usually Mean
MRI reports are written for clinicians, so the wording can sound alarming even when findings are minor or expected. Below are common terms and plain-language explanations. These are general explanations, not a diagnosis.
“No Acute Intracranial Abnormality”
This often means there is no clear evidence of a recent major problem, such as a large bleed, a significant mass, or a major acute stroke pattern on the sequences reviewed.
“Incidental Finding”
An incidental finding is something seen on the scan that was not the main reason for the MRI. Many incidental findings are harmless, but some require monitoring.
“Lesion”
A lesion is a general word for an area that looks different from surrounding tissue. It does not automatically mean cancer. Context and pattern matter.
“White Matter Changes” or “White Matter Hyperintensities”
White matter refers to the brain’s communication pathways. “Changes” can be seen for many reasons, including age-related changes, migraine-associated patterns in some people, vascular risk factors, and inflammatory conditions. The significance depends on your age, symptoms, and health history.
“FLAIR Hyperintensity”
FLAIR is a type of MRI sequence. A “hyperintensity” means an area appears brighter on that sequence. It is a description, not a diagnosis.
“Restricted Diffusion” or “DWI”
Diffusion-weighted imaging (DWI) looks at how water moves in tissue. “Restricted diffusion” can be seen in certain acute processes such as early stroke, but it can also appear in other conditions. It must be interpreted with the full scan and your symptoms.
“Enhancement”
If contrast is used, “enhancement” means an area takes up contrast and appears brighter. This can occur with inflammation, infection, some tumours, and other processes. The pattern of enhancement is important.
“Edema”
Edema means swelling, often due to fluid in tissue. MRI can show edema around tumours, after injury, or with inflammation.
“Mass Effect” and “Midline Shift”
“Mass effect” means something is pressing on nearby structures. “Midline shift” means pressure has moved structures away from the centre line. These terms are taken seriously and usually require urgent clinical correlation.
“Atrophy” or “Volume Loss”
Atrophy refers to reduced brain volume. Some degree can occur with aging. The report often describes where it is seen and whether it appears more than expected for age.
“Ventricles”
Ventricles are fluid-filled spaces in the brain. The report may describe them as normal, prominent, enlarged, or compressed, depending on what is seen.
“Sinus Mucosal Thickening”
This usually refers to inflammation in the sinus lining. It can be related to sinus congestion and is commonly incidental on head imaging.
“Artifact”
An artifact is image distortion, often from movement, dental work, or metal. It does not mean disease, it means image quality was affected.
Tip: If a report worries you, ask your clinician two simple questions:
- What findings matter for my symptoms?
- What happens next, if anything?
MRI Safety and Risks
A head MRI is considered very safe for most people, but there are a few important safety points:
- The magnet can interact with certain implants or metal fragments, so screening is essential.
- Contrast reactions are uncommon, and serious allergic reactions are rare.
- Gadolinium contrast is handled carefully in people with significant kidney disease.
- Pregnancy considerations vary by trimester and urgency, so always inform your clinician if you are pregnant or might be pregnant.
- The radiology team’s screening questions may feel repetitive, but they are there to keep you safe.
Frequently Asked Questions
Is a head MRI the same as a brain MRI?
In most cases, yes. Both terms are commonly used for the same scan of the brain and structures in the head. Some protocols focus on specific areas, such as the pituitary gland.
Does an MRI head scan use radiation?
No. MRI uses magnets and radio waves, not ionizing radiation.
How long does a brain MRI take?
Commonly 30 to 60 minutes, sometimes longer depending on the protocol and whether contrast is used.
What is contrast and do I need it?
Contrast is a dye injected through an IV to improve visibility of certain tissues. Not all MRIs need it. The decision depends on symptoms and what the clinician is looking for.
What if I have claustrophobia?
Many centres offer options such as headphones, mirrors, calming techniques, wide-bore scanners, or sedation when appropriate. Tell the team in advance.
Can I eat before a head MRI?
Often yes, but instructions can vary, especially if contrast or sedation is planned. Follow the imaging centre’s guidance.
When will I get results?
A radiologist reviews the scan and sends a report to your clinician. Many reports are available within a day or two, but timelines vary.
What should I do if my MRI report has scary terms?
Do not panic based on wording alone. Reports use technical descriptions. Discuss what the findings mean in your situation with your clinician.