Preventive Healthcare
Von Willebrand Disease: Causes, Symptoms, and Treatment
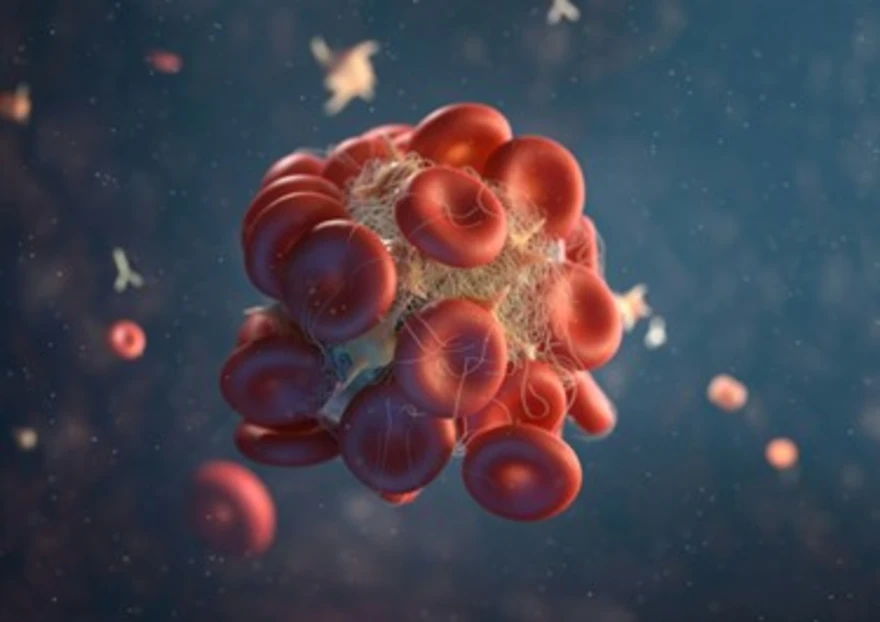
Table of Contents
- What Is Von Willebrand Disease?
- Von Willebrand Disease Types
- Von Willebrand Disease Causes & Risk Factors
- Symptoms of Von Willebrand Disease
- How Von Willebrand Disease Affects the Body
- Complications
- Diagnosis of Von Willebrand Disease
- Tests for Von Willebrand Disease
- Treatment Options
- Lifestyle & Home Care Tips
- Living With Von Willebrand Disease
- When to Seek Medical Help
- Conclusion
- FAQs
- References
What Is Von Willebrand Disease?
Von Willebrand Disease (VWD) is an inherited bleeding disorder in which the body produces insufficient or defective Von Willebrand factor (VWF), a protein essential for blood clotting. This protein is vital in helping blood platelets stick together to form clots and stop bleeding. When VWF is deficient or defective, blood clotting is delayed, causing prolonged bleeding even from minor injuries or medical procedures.
It is among the most common inherited bleeding disorders, affecting approximately 1 in 100 people worldwide. While many people have mild symptoms that go unnoticed, others experience significant bleeding episodes requiring lifelong care. Both men and women can be affected equally, although women may notice symptoms more due to menstrual and postpartum bleeding.
Von Willebrand Disease Types
VWD is categorised into three major types based on the level and functionality of the VWF protein:
- Type 1:
The most common and usually mild form is one in which individuals have lower-than-normal levels of VWF, but it functions correctly. Bleeding tends to be mild to moderate. - Type 2:
Here, the VWF is present but doesn’t work as it should. This type has four subtypes — 2A, 2B, 2M, and 2N — depending on how the protein’s function is affected. - Type 3:
The rarest and most severe form. People with this type have very little or no VWF, leading to severe bleeding episodes that can occur spontaneously or after minor trauma.
Understanding your VWD type is critical for accurate diagnosis and treatment, as therapies differ for each.
Von Willebrand Disease Causes & Risk Factors
The primary cause of Von Willebrand Disease is a genetic mutation in the VWF gene. This mutation affects the body’s ability to produce enough Von Willebrand factor or alters its structure, impairing its function.
However, in some cases, people can acquire the disease later in life — known as acquired VWD — due to other health conditions or external factors.
Common causes and risk factors include:
- Inherited mutation in the VWF gene, transmitted in an autosomal dominant or recessive pattern
- Family history of abnormal bleeding tendencies
- Autoimmune diseases that produce antibodies against VWF
- Certain cancers, like lymphomas or leukaemias
- Medications such as valproic acid or ciprofloxacin
- Conditions like hypothyroidism or heart valve defects that affect blood proteins
Having one parent with the disease increases the risk of passing it to children, although symptom severity may vary even within families.
Symptoms of Von Willebrand Disease
The symptoms depend on the type and severity of the disease, but generally involve excessive or prolonged bleeding.
Common symptoms include:
- Frequent or prolonged nosebleeds that last over 10 minutes
- Easy bruising, often with large or raised bruises
- Prolonged bleeding after surgery, dental procedures, or injury
- Heavy menstrual bleeding (menorrhagia) in women, sometimes leading to anaemia
- Bleeding from gums during brushing or dental work
- Blood in stool or urine in severe cases
- Bleeding into joints or muscles, leading to pain, swelling, and restricted movement (more common in severe Type 3 cases)
Because symptoms can mimic other bleeding conditions, a proper laboratory diagnosis is essential.
How Von Willebrand Disease Affects the Body
In a healthy person, the Von Willebrand factor acts like a bridge — helping platelets stick to damaged blood vessel walls and to each other to form a stable blood clot. It also protects another clotting protein called Factor VIII, which is crucial for clot stability.
In VWD, either due to deficiency or dysfunction of this factor:
- Blood platelets cannot adhere properly to the injury site.
- Factor VIII levels drop, slowing the entire clotting process.
- This results in delayed, prolonged, or recurrent bleeding, even from minor wounds.
If left untreated, VWD can lead to complications such as chronic anaemia, internal bleeding, or delayed recovery after surgery.
Complications
If Von Willebrand Disease (VWD) is left untreated or not adequately managed, it can lead to several short-term and long-term complications affecting overall health and quality of life. These complications vary depending on the severity of the disease and the extent to which it is controlled through treatment and preventive care.
- Chronic anaemia due to long-term blood loss: Repeated or prolonged bleeding, particularly from the gastrointestinal tract or heavy menstrual cycles, can result in iron deficiency and chronic fatigue.
- Joint or muscle bleeding leading to stiffness and pain: In severe cases (especially Type 3 VWD), bleeding into joints or muscles may occur, causing swelling, restricted movement, and pain similar to that seen in haemophilia.
- Severe postpartum haemorrhage in women: Women with VWD are at higher risk of excessive bleeding during childbirth or after delivery. Without preventive care, this can become a life-threatening emergency.
- Internal bleeding during or after surgery or injury: Surgical or accidental trauma can cause uncontrolled internal bleeding, especially if the condition is undiagnosed or VWF levels are not managed before the procedure.
- Reduced quality of life due to frequent hospital visits or bleeding anxiety: Recurrent bleeding episodes, prolonged recovery time, and fear of injury may affect daily routines, emotional well-being, and participation in normal activities.
Diagnosis of Von Willebrand Disease
Since symptoms often overlap with those of other conditions, such as haemophilia, accurate diagnosis requires a combination of history, physical examination, and specialised laboratory tests.
Diagnostic steps include:
- Detailed medical and family history – assessing for frequent nosebleeds, heavy periods, or prolonged bleeding after procedures.
- Physical examination – to check for bruises, gum bleeding, or signs of anaemia.
- Basic screening tests – such as Complete Blood Count (CBC), Prothrombin Time (PT), and Activated Partial Thromboplastin Time (aPTT).
- Specialised coagulation tests – measuring the amount and activity of Von Willebrand factor and Factor VIII levels.
- Genetic testing – for identifying specific mutations and differentiating inherited from acquired forms.
Testing may need to be repeated because factors like stress, infection, or hormonal changes can temporarily alter VWF levels.
Tests for Von Willebrand Disease
A comprehensive range of advanced laboratory tests is available to diagnose and monitor Von Willebrand Disease (VWD) accurately:
- VW – Von Willebrand Antigen, Citrated Plasma: Measures the quantity of Von Willebrand Factor (VWF) protein in the blood to detect any deficiency.
- Ristocetin Cofactor Activity (VWF: RCo): Assesses the functional activity of VWF by evaluating its ability to help platelets clump together and form clots.
- Factor VIII Activity Test: Determines the level of Factor VIII, a clotting protein that works in conjunction with VWF to stop bleeding.
- VWF Multimer Analysis: Examines the structural features of VWF molecules to identify abnormalities and distinguish among VWD subtypes.
- Von Willebrand Disease Gene Panel by NGS, EDTA Blood: According to the National Institutes of Health (NIH), next-generation sequencing (NGS) of the VWF gene helps confirm inherited or acquired forms of the disorder.
These tests, performed with high-precision technology, enable accurate diagnosis, subtype classification, and effective disease management.
Treatment Options
Although Von Willebrand Disease cannot be cured, treatment can effectively control bleeding and prevent complications. The approach depends on the type and severity of the disease.
Medications & Therapies
- Desmopressin (DDAVP): A synthetic hormone that stimulates the release of stored VWF and Factor VIII from blood vessel walls. Often used before dental or minor surgical procedures.
- VWF or Factor VIII concentrates: Used in moderate to severe cases, especially when desmopressin is ineffective or contraindicated.
- Antifibrinolytic drugs (e.g., Tranexamic Acid): Help prevent clots from breaking down, particularly useful during menstruation or dental work.
- Hormonal therapy or oral contraceptives: Used in women to control heavy menstrual bleeding.
- Topical hemostatic agents: Such as thrombin sprays or fibrin sealants to manage localised bleeding.
Treatment plans are individualised and regularly reviewed by a haematologist.
Lifestyle & Home Care Tips
Living with Von Willebrand Disease (VWD) requires daily awareness and careful preventive habits to minimise bleeding risks and maintain overall well-being. Adopting a few mindful practices can make a significant difference in managing the condition effectively:
- Avoid aspirin and NSAIDs (such as ibuprofen): These medications can interfere with platelet function and worsen bleeding tendencies. Always consult your doctor before taking pain relievers.
- Practice gentle oral hygiene: Use a soft-bristle toothbrush and maintain good dental care to prevent gum bleeding and infections.
- Inform healthcare providers in advance: Always notify your dentist, surgeon, or gynaecologist about your VWD diagnosis before undergoing any medical or dental procedures.
- Track menstrual health: Women should monitor menstrual flow and seek medical advice for heavy or prolonged periods to prevent anaemia.
- Follow an iron-rich diet: Include leafy greens, lean meats, lentils, and fortified cereals to help maintain healthy haemoglobin levels and compensate for blood loss.
- Carry medical identification: Wear a medical alert bracelet or carry a card, indicating your diagnosis and treatment details to assist healthcare providers in emergencies.
- Encourage safe physical activity: Children with VWD should avoid contact sports but can participate in non-contact activities like swimming or walking to stay healthy and confident.
Living With Von Willebrand Disease
People with VWD can live whole, active, and healthy lives with the right care plan. Regular medical checkups, adherence to treatment, and family education on emergency management are essential.
In women, planning pregnancies under medical supervision ensures safe delivery and recovery. Emotional well-being also matters — joining support groups or speaking with a counsellor can reduce anxiety related to chronic illness.
When to Seek Medical Help
Contact your doctor immediately if you experience:
- Frequent or uncontrolled nosebleeds
- Heavy menstrual bleeding causing fatigue or pallor
- Blood in urine or stool
- Joint pain or swelling from suspected internal bleeding
- Prolonged bleeding after surgery or dental extraction
Prompt intervention can prevent severe complications and ensure safety.
Conclusion
Von Willebrand Disease, though uncommon, is one of the most manageable bleeding disorders when identified early and monitored consistently. Understanding your specific type, adhering to prescribed medication, and scheduling periodic follow-ups with your healthcare provider can significantly reduce bleeding risks and help you lead a healthy, active life.
At Metropolis Healthcare, we support your journey toward better health with over 4000 specialised tests, including advanced coagulation and genetic testing panels for accurate diagnosis. Our comprehensive testing, home collection service, and quick reporting ensure both accuracy and convenience at every step. With 10,000+ home-collection touchpoints, seamless booking via website, phone, app, or WhatsApp, and a reputation for precision and trust, we make preventive care simple and accessible.
FAQs
Is Von Willebrand Disease hereditary?
Yes. Most cases are inherited from a parent carrying a defective VWF gene. It follows an autosomal pattern, meaning both males and females are equally affected.
Can Von Willebrand Disease be cured?
There is no permanent cure, but medications and preventive measures can effectively control symptoms and reduce bleeding risks.
What is the life expectancy with Von Willebrand Disease?
With timely diagnosis and appropriate treatment, individuals with VWD generally enjoy a normal life expectancy.
How is Von Willebrand Disease diagnosed?
- Evaluation of personal and family bleeding history
- VWF antigen and activity testing
- Factor VIII assay
- Genetic testing to confirm hereditary forms
Can women with Von Willebrand Disease have normal pregnancies?
Yes, most women can have safe pregnancies with careful monitoring and preventive care to avoid excessive bleeding during childbirth and postpartum recovery.
References
https://pmc.ncbi.nlm.nih.gov/articles/PMC9086814/
https://www.mayoclinic.org/diseases-conditions/von-willebrand-disease/symptoms-causes/syc-20354978
https://my.clevelandclinic.org/health/diseases/17709-von-willebrand-disease
https://emedicine.medscape.com/article/206996-overview




























