Preventive Healthcare
Hemangioblastoma: Causes, Symptoms & Latest Research
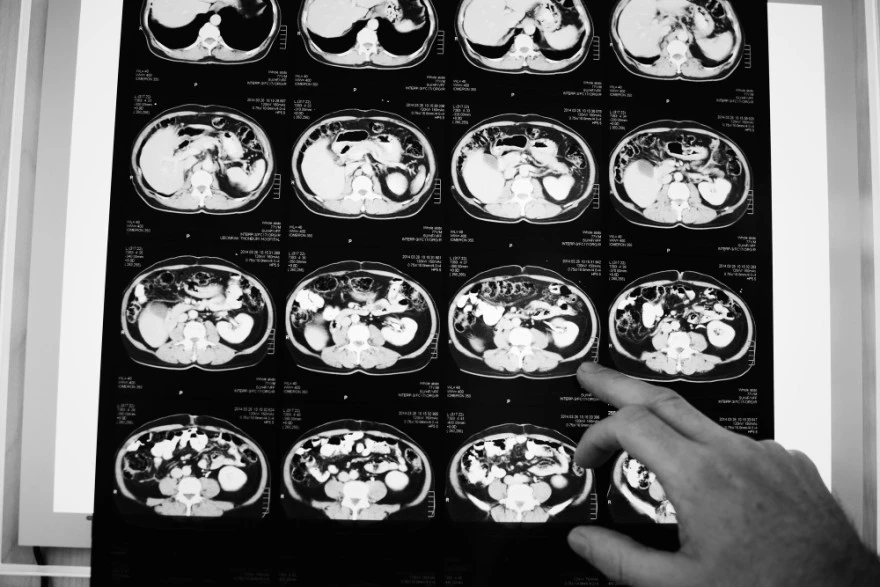
Table of Contents
- What is Hemangioblastoma?
- Hemangioblastoma Causes
- Symptoms of Hemangioblastoma
- How is Hemangioblastoma Diagnosed?
- Diagnostic and Imaging Methods for Hemangioblastoma
- Hemangioblastoma Treatment Options
- Latest Research on Hemangioblastoma
- Prognosis for Hemangioblastoma Patients
- Living with Hemangioblastoma
- Conclusion
- FAQs
What is Hemangioblastoma?
A Hemangioblastoma is a highly vascular, benign neoplasm arising from vascular stromal cells of the central nervous system. Most Hemangioblastomas occur in the cerebellum (about 70%), followed by the spinal cord and brainstem and, rarely, the temporal lobe cortex.
Hemangioblastomas are characterized by an exceptionally rich capillary network, differentiating them from other posterior fossa tumours such as medulloblastoma or metastasis. Studies indicate that around one-quarter of Hemangioblastomas are linked to inherited genetic conditions, most notably Von Hippel–Lindau (VHL) disease, which results from mutations in the VHL gene.
Hemangioblastoma Causes
• Sporadic occurrence: Most Hemangioblastomas develop randomly without known environmental or lifestyle factors
• Von Hippel-Lindau (VHL) disease: This inherited genetic syndrome accounts for 20-25% of cases and significantly increases tumour development risk
• Genetic predisposition: Individuals with VHL syndrome carry pathogenic variants in the VHL tumour suppressor gene, leading to abnormal angiogenesis and tumour formation
Symptoms of Hemangioblastoma
Hemangioblastoma brain symptoms vary depending on tumour location and size. Common presentations include:
• Persistent headaches: Often caused by increased pressure inside the skull
• Balance and coordination problems: Unsteady gait, intention tremor, or clumsiness due to cerebellar involvement, and impaired fine motor control
• Nausea and vomiting: Result from increased intracranial pressure
• Dizziness and vertigo: Particularly when tumours affect the cerebellum
• Weakness or numbness: In arms and legs, especially with spinal cord involvement
• Vision problems: Blurred vision or eye pain if affecting visual pathways
• Speech difficulties: When tumours impact language regions or temporal lobe cortex
• Cognitive changes: Memory or concentration problems in some cases
How is Hemangioblastoma Diagnosed?
- Clinical assessment: Healthcare providers evaluate neurological symptoms and medical history
- CT scan imaging: Useful for detecting hyperdense lesions or cystic components and for preoperative planning when MRI is not available
- MRI scan examination: Detailed imaging reveals precise tumour location, size, and characteristics
- Digital subtraction angiography: Demonstrates intense vascular blush and feeding arteries, aiding in surgical or embolization planning and tumour vascularity
- Genetic testing: Recommended for patients with multiple tumours or family history of Von Hippel-Lindau (VHL) disease
- Biopsy consideration: Biopsy is rarely indicated because Hemangioblastomas exhibit highly characteristic imaging findings; biopsy carries a significant bleeding risk
Diagnostic and Imaging Methods for Hemangioblastoma
• MRI scan technology: Primary imaging method providing detailed brain tissue visualisation
• CT scan assessment: Identifies tumour masses and detects acute or previous bleeding
• Contrast-enhanced imaging: Uses special dyes to highlight blood vessels and tumour characteristics
• Angiographic studies: Evaluate tumour blood supply for surgical planning
• Follow-up surveillance: Regular imaging monitors tumour growth in asymptomatic cases
• Advanced imaging protocols: T1 and T2-weighted sequences highlight different tissue properties
Hemangioblastoma Treatment Options
Hemangioblastoma treatment varies based on tumour size, location, and patient symptoms:
• Observation and monitoring: Small, asymptomatic tumours may require only regular imaging surveillance
• Surgical resection: Complete tumour removal remains the gold standard treatment
• Stereotactic radiosurgery: Precise radiation delivery for surgically challenging cases
• Antiangiogenic therapy (e.g., VEGF inhibitors): Represents an emerging adjunct, particularly in recurrent or unresectable VHL-associated lesions
• Combined approaches: Integration of multiple treatment modalities for optimal outcomes
Surgical Treatment for Hemangioblastoma
Gross total surgical resection remains the definitive treatment and is curative in most sporadic cases for Hemangioblastoma treatment. Neurosurgeons carefully remove the tumour whilst preserving surrounding healthy brain tissue. Their high vascularity necessitates meticulous microsurgical technique and sometimes preoperative embolization to minimize intraoperative bleeding to minimise bleeding complications. Complete surgical removal offers excellent long-term outcomes when total resection is achieved. However, surgery carries inherent risks, including bleeding, infection, and potential neurological deficits depending on tumour location.
Radiation Therapy for Hemangioblastoma
Focused radiation therapy serves as an important alternative when surgery isn't feasible or for recurrent tumours. Modern techniques like stereotactic radiosurgery deliver precise radiation doses whilst sparing healthy brain tissue. This approach proves particularly valuable for patients with multiple tumours associated with Von Hippel-Lindau (VHL) disease. Radiation therapy success rates continue improving with technological advances, though long-term effects require ongoing study.
Latest Research on Hemangioblastoma
• Complete surgical resection: Remains the gold standard, achieving high progression-free survival rates of 95.1% at 72 months in sporadic cases and 91.1% in VHL-associated spinal tumours, with early intervention optimising recovery outcomes
• Stereotactic radiosurgery advances: Stereotactic radiosurgery (SRS) achieves durable local control rates of 78–96% at 10 years, particularly valuable for small, deep-seated, or surgically inaccessible lesions for small, high-risk Hemangioblastomas, with rates of 78-96% at 10 years, particularly suitable for anatomically challenging or asymptomatic tumours
• Antiangiogenic therapy: Targets the vascular supply of Hemangioblastomas, showing promise as additional treatment options alongside surgery or radiation, with combined approaches enhancing safety and recovery
Prognosis for Hemangioblastoma Patients
The outlook for Hemangioblastoma patients is generally excellent when diagnosed early and treated appropriately. Factors influencing prognosis include tumour size, location, patient age, and presence of Von Hippel-Lindau (VHL) disease.
Sporadic Hemangioblastomas are typically solitary and cured with a single surgery, whereas VHL patients require lifelong imaging due to multifocal disease, whilst those with VHL syndrome need lifelong monitoring for new tumours. Regular follow-up with MRI scan surveillance ensures early detection of any recurrence or new lesions.
Hemangioblastoma in Children
Paediatric Hemangioblastoma is exceedingly rare; when present, it almost always occurs in the context of VHL disease but require specialised management approaches. Children with Von Hippel-Lindau (VHL) disease face higher risks of developing multiple tumours throughout their lives, necessitating regular surveillance and coordinated care. Treatment strategies must balance tumour control with preserving developing neurological function, often requiring multidisciplinary teams including paediatric neurosurgeons, oncologists, and rehabilitation specialists.
Living with Hemangioblastoma
Managing life with Hemangioblastoma involves regular medical follow-up, symptom monitoring, and lifestyle adaptations. Patients often wonder about activity restrictions, work capabilities, and long-term implications. Many individuals with successfully treated Hemangioblastomas return to normal activities, though some may require ongoing physical therapy or occupational support. Support groups and patient organisations provide valuable resources for navigating the emotional and practical challenges of living with a brain tumour diagnosis.
Conclusion
Understanding Hemangioblastoma empowers patients and families to make informed decisions about their health journey. These benign tumours, whilst concerning at diagnosis, often respond excellently to appropriate treatment. The key lies in early detection, comprehensive evaluation, and personalised treatment planning with experienced medical teams.
Modern diagnostic advances — especially in high-resolution MRI and angiographic imaging — enable precise localisation and surgical planning, enable precise tumour characterisation, whilst evolving treatment options, from surgical resection to stereotactic radiosurgery, offer hope for excellent outcomes.
At Metropolis Healthcare, we support your diagnostic journey with comprehensive testing services spanning our network of over 220 laboratories and 4,600 service centres. Our home sample collection service brings convenient, reliable diagnostics to your doorstep, ensuring you receive the accurate results needed for informed healthcare decisions. With more than 4,000 tests available, including specialised panels for genetic conditions, we're committed to empowering your health management.
FAQs
Can Hemangioblastoma be cured?
Yes, Hemangioblastoma can often be cured through complete surgical resection, with excellent long-term outcomes and minimal recurrence rates in most cases.
What are the early signs of Hemangioblastoma?
Early symptoms include persistent headaches, balance problems, dizziness, and coordination difficulties, particularly affecting fine motor skills and walking.
How is Hemangioblastoma different from other brain tumours?
Hemangioblastomas are benign, slow-growing tumours that don't spread, unlike aggressive tumours such as medulloblastoma or malignant brain cancers.
Is surgery always necessary for Hemangioblastoma?
No, small asymptomatic tumours may only require monitoring, whilst symptomatic or growing tumours typically benefit from surgical intervention.
References
1. https://my.clevelandclinic.org/health/diseases/22738-hemangioblastoma
2. https://www.cancerresearchuk.org/about-cancer/brain-tumours/types/Hemangioblastoma
3. https://www.ncbi.nlm.nih.gov/books/NBK606126/
4. https://pmc.ncbi.nlm.nih.gov/articles/PMC12309710/
5. https://pmc.ncbi.nlm.nih.gov/articles/PMC11276307/#sec4-curroncol-31-00293
6. https://www.explorationpub.com/Journals/en/Article/100631