Preventive Healthcare
Aortic Valve Disease: Causes, Symptoms, Diagnosis & Treatment
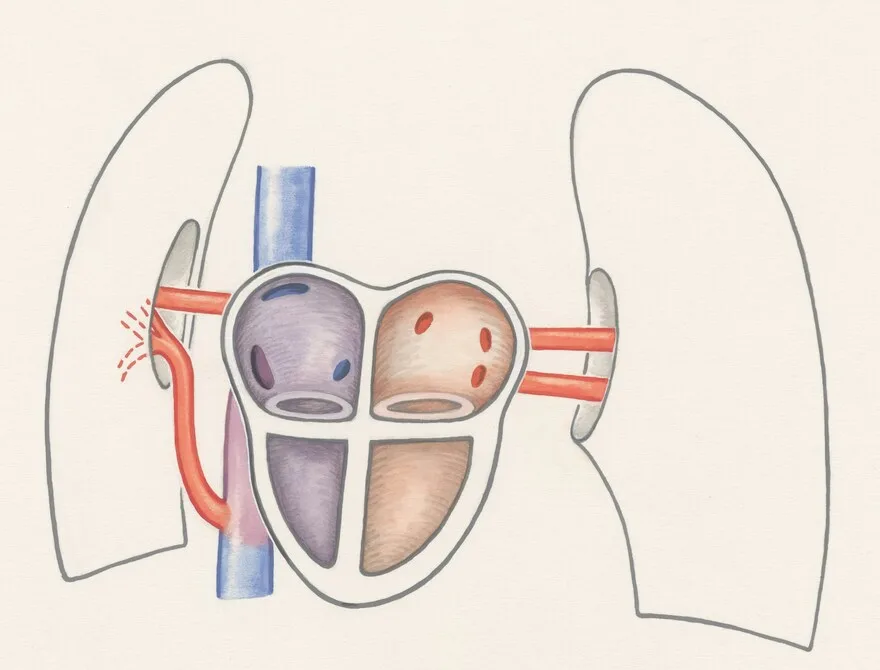
Table of Contents
- What is Aortic Valve Disease?
- Types of Aortic Valve Disease
- Causes & Risk Factors for Aortic Valve Disease
- Signs and Symptoms of Aortic Valve Disease
- Diagnostic and Imaging Tests for Aortic Valve Disease
- Treatment Options for Aortic Valve Disease
- Transcatheter Aortic Valve Replacement (TAVR)
- Lifestyle & Prevention Tips for Aortic Valve Disease
- Prognosis & Recovery
- Conclusion
- Frequently Asked Questions (FAQ)
- References
What is Aortic Valve Disease?
The heart has four valves that ensure blood flows in the right direction — one of them is the aortic valve. It connects the left ventricle (the heart’s main pumping chamber) to the aorta (the largest artery that supplies oxygen-rich blood to the body).
In aortic valve disease, this valve doesn’t open or close properly. When it becomes narrowed (aortic stenosis), blood flow from the left ventricle to the aorta is restricted. When it leaks (aortic regurgitation), some blood flows backward into the left ventricle. Both conditions force the heart to work harder to maintain circulation, which can eventually lead to heart muscle thickening, fatigue, and even heart failure if left untreated.
Aortic valve disease may develop gradually over many years or, in rare cases, appear suddenly due to infection (endocarditis) or trauma. Understanding its causes, symptoms, and treatment options is essential for early intervention and better outcomes.
Types of Aortic Valve Disease
Aortic valve disease can appear in several forms, depending on how the valve is affected:
- Aortic Stenosis: The valve opening becomes stiff or narrowed, making it harder for blood to flow from the left ventricle into the aorta. This is the most common form in older adults, primarily due to age-related calcium deposition on valve leaflets.
- Aortic Regurgitation (Aortic Insufficiency): The valve doesn’t close completely, allowing blood to leak backwards into the heart. This reduces the amount of oxygenated blood that reaches the body and can cause breathlessness and fatigue.
- Congenital Bicuspid Valve: Normally, the aortic valve has three flaps (cusps). Some people are born with only two (bicuspid valve), making it more prone to early wear, stenosis, or regurgitation.
- Mixed Aortic Valve Disease: A combination of stenosis and regurgitation, where the valve both narrows and leaks.
Each type affects heart function differently, but all require timely diagnosis and careful management to prevent complications.
Causes & Risk Factors for Aortic Valve Disease
Aortic valve disease can occur due to congenital defects, infections, age-related wear, or other heart conditions.
Common Causes:
- Congenital bicuspid valve: Present from birth and often discovered later in life.
- Rheumatic fever: A complication of untreated strep throat that causes inflammation and scarring of heart valves.
- Age-related (degenerative) changes: Calcium buildup on the valve leaflets causes stiffness, particularly in adults over 65.
- Endocarditis: Infection of the heart’s inner lining or valves caused by bacteria entering the bloodstream.
- Radiation therapy: Previous chest radiation can lead to delayed valve calcification or fibrosis years later.
- Connective tissue disorders: Conditions like Marfan or Ehlers-Danlos syndrome can weaken the valve structure.
Risk Factors:
- Increasing age (above 60 years)
- High blood pressure or high cholesterol
- History of rheumatic fever
- Smoking or excessive alcohol consumption
- Family history of heart valve problems or congenital defects
- Chronic kidney disease or autoimmune conditions
Addressing risk factors early through lifestyle management and routine heart health checkups can significantly lower disease progression.
Signs and Symptoms of Aortic Valve Disease
According to the National Institutes of Health (NIH), aortic valve disease may remain silent for years. As the condition worsens, symptoms gradually appear due to reduced blood flow or backflow.
Common symptoms include:
- Shortness of breath: Especially during physical activity or when lying down.
- Chest pain or tightness: Occurs when the heart struggles to pump blood efficiently.
- Fatigue or weakness: Caused by reduced cardiac output and oxygen delivery.
- Palpitations: A feeling of skipped or rapid heartbeats.
- Fainting or dizziness: Caused by limited blood flow to the brain.
- Swollen ankles or feet: A sign of fluid retention linked to heart failure.
- Heart murmur: Often detected by doctors during routine examination.
Ignoring early symptoms can be dangerous — if left untreated, severe aortic valve disease can lead to heart failure or arrhythmias.
Diagnostic and Imaging Tests for Aortic Valve Disease
Early diagnosis is critical to managing aortic valve disease effectively. Your doctor may recommend several tests to confirm the condition and determine its severity.
Common diagnostic tests include:
- Echocardiogram (Echo): Uses ultrasound to visualise valve structure and function — it’s the most reliable test to measure valve narrowing or leakage.
- Electrocardiogram (ECG): Records heart rhythm abnormalities or signs of left ventricular strain.
- Chest X-ray: Reveals heart enlargement (cardiomegaly) or fluid accumulation in the lungs (pulmonary congestion).
- Cardiac MRI/CT scan: Provides detailed images of heart anatomy and valve movement.
- Cardiac catheterisation: An invasive test used to measure pressure and flow within heart chambers.
- CK-MB Test: Measures a heart-specific enzyme fraction that helps differentiate cardiac from skeletal muscle injury.
- Troponin I Test: A highly specific cardiac biomarker used to detect myocardial infarction or significant cardiac strain.
- Troponin-T Test: Assesses the extent and severity of heart muscle damage following ischemia or infarction.
- NT-Pro BNP Test: Measures levels of a cardiac hormone released during heart failure to assess ventricular strain and fluid overload.
- Heart Failure Profile: A multi-marker panel used to evaluate cardiac function and monitor heart failure severity.
Treatment Options for Aortic Valve Disease
Treatment depends on disease type, severity, and overall health. While mild cases can be managed medically, advanced cases often require surgical intervention.
Medications to Manage Symptoms
Medication doesn’t cure the valve problem but helps manage related symptoms and prevent complications.
- Diuretics – Reduce fluid buildup and relieve breathlessness.
- Beta-blockers – Slow heart rate, improve oxygen efficiency.
- ACE inhibitors or ARBs – Lower blood pressure and ease heart strain.
- Anticoagulants (blood thinners) – Prevent clots, especially if you have an irregular heart rhythm or a mechanical valve.
- Vasodilators – Widen blood vessels and improve blood flow.
These drugs are prescribed based on individual conditions and must be regularly monitored by a cardiologist.
Surgical Valve Repair or Replacement
When the valve is severely damaged, surgery becomes necessary.
- Valve Repair: Involves reshaping or removing calcium deposits from the valve leaflets.
- Valve Replacement: The diseased valve is replaced with either a mechanical valve (durable but requires lifelong anticoagulants) or a biological valve (made from animal or human tissue, lasting 10–20 years).
Transcatheter Aortic Valve Replacement (TAVR)
Transcatheter Aortic Valve Replacement (TAVR) is a minimally invasive alternative to open-heart surgery, primarily for older patients or those at intermediate or high surgical risk.
A catheter is inserted through the leg artery, and a new valve is positioned inside the old, diseased one. Recovery is faster, hospital stay is shorter, and complications are fewer compared to traditional surgery.
Modern hospitals increasingly prefer TAVR for patients unsuitable for open procedures, making it one of the most significant breakthroughs in aortic valve disease treatment.
Lifestyle & Prevention Tips for Aortic Valve Disease
While congenital conditions can’t be prevented, lifestyle changes can reduce risks and improve heart health.
- Eat a balanced diet low in salt, saturated fats, and trans fats.
- Exercise regularly — walking, swimming, or yoga can help maintain cardiac fitness.
- Quit smoking and limit alcohol intake.
- Keep blood pressure, blood sugar, and cholesterol in check.
- Get vaccinated against infections that can lead to rheumatic fever.
- Maintain good dental hygiene — untreated gum infections can lead to infective endocarditis, affecting heart valves.
- Schedule routine heart check-ups if you have a known bicuspid or damaged valve.
Simple, consistent habits go a long way in preventing valve deterioration and supporting overall heart wellness.
Prognosis & Recovery
The outlook for aortic valve disease has improved significantly with advancements in diagnosis and surgery.
With proper medical care, most patients can live healthy, active lives. Recovery after valve repair or TAVR typically takes a few weeks, with gradual improvement in stamina and breathing.
Long-term success depends on regular cardiac monitoring, lifestyle adjustments, and adherence to prescribed medication. Patients with prosthetic valves or a history of endocarditis may require preventive antibiotics before dental or surgical procedures, as advised by their doctor.
Conclusion
Aortic valve disease may sound alarming, but with early detection, modern diagnostics, and timely intervention, it can be effectively managed.
Metropolis Healthcare offers comprehensive cardiac diagnostic services — from echocardiograms and lipid profiles to specialised cardiac enzyme tests — ensuring accurate and timely evaluation. With 4,000+ tests, NABL & CAP accredited labs, 10,000+ home collection touchpoints, and convenient booking options via website, app, call, or WhatsApp, Metropolis makes quality diagnostics accessible and reliable for every individual. Take charge of your heart health today — early diagnosis truly saves lives.
Frequently Asked Questions (FAQ)
What causes aortic valve disease?
It can be caused by congenital abnormalities such as a bicuspid valve, age-related degeneration, rheumatic fever, or infections like endocarditis that damage valve tissue.
What are the early signs of aortic valve disease?
- Mild breathlessness during activity
- Fatigue and reduced stamina
- Chest tightness or pressure, especially during exertion
Can aortic valve disease be cured without surgery?
While mild cases can be managed with medication and lifestyle modifications, severe forms typically require valve repair or replacement for lasting improvement.
How is aortic valve disease diagnosed?
- Echocardiogram – Main diagnostic tool to evaluate structure and flow.
- ECG – Identifies irregular rhythms.
- CT/MRI scans – Provide detailed anatomical insight.
- Cardiac catheterisation – Measures internal pressure for surgical planning.
What is the difference between aortic stenosis and regurgitation?
- Aortic Stenosis: Valve narrowing restricts blood flow from the heart.
- Aortic Regurgitation: Valve leakage causes backward blood flow.
Is aortic valve disease life-threatening?
Yes, if left untreated, it can lead to heart failure, arrhythmias, or sudden cardiac death. With early intervention and proper treatment, most patients live full, healthy lives.
Can lifestyle changes prevent aortic valve disease?
- Eat heart-friendly foods (fruits, vegetables, whole grains).
- Maintain a healthy weight.
- Avoid smoking and manage cholesterol.
- Stay active with regular, moderate-intensity exercise approved by your cardiologist.
- Schedule regular cardiac evaluations and echocardiograms to monitor valve function.
References
https://www.ncbi.nlm.nih.gov/books/NBK542205/
https://www.mayoclinic.org/diseases-conditions/aortic-valve-disease/symptoms-causes/syc-20355117
https://my.clevelandclinic.org/health/diseases/24452-aortic-valve-disease
https://www.ahajournals.org/doi/10.1161/01.cir.0000027621.26167.5e




























