Preventive Healthcare
Transverse Myelitis: Symptoms, Causes & Treatment
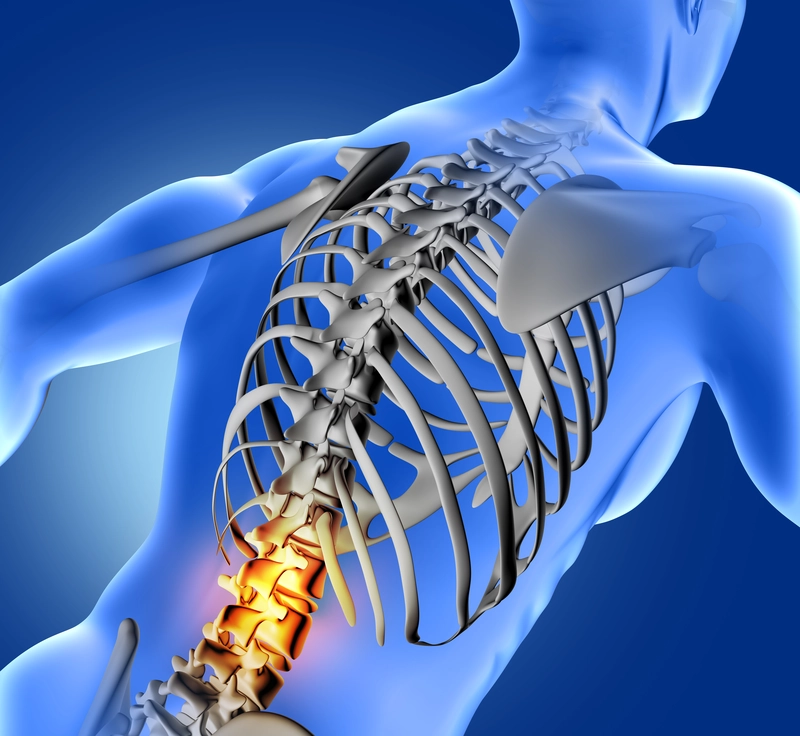
Table of Contents
- What Is Transverse Myelitis?
- Symptoms of Transverse Myelitis
- Causes of Transverse Myelitis
- Risk Factors for Transverse Myelitis
- Complications of Transverse Myelitis
- How Transverse Myelitis Is Diagnosed
- Treatment for Transverse Myelitis
- Pain Management
- Recovery and Prognosis
- Prevention Tips
- When to Seek Medical Help
- Conclusion
- FAQs
- References
What Is Transverse Myelitis?
Transverse myelitis (TM) is a rare neurological disorder characterised by inflammation of the spinal cord, leading to injury of the myelin sheath — the protective fatty covering of nerve fibres, the protective fatty covering surrounding nerve fibres in the spinal cord. Myelin acts as insulation, allowing electrical signals to efficiently travel between the nerves of the spinal cord and the rest of the body. When this myelin is damaged or destroyed in TM, the nerves cannot properly conduct these signals. The inflammation seen in TM often extends across a specific segment of the spinal cord, leading to the term "transverse".
Depending on the level of the spinal cord affected, this impaired nerve signalling can cause a variety of neurological symptoms, which may include muscle weakness, sensory changes, pain, and bowel/bladder problems. TM can strike individuals of any age, gender, or background, often with a rapid onset of symptoms that can significantly impact quality of life.
Symptoms of Transverse Myelitis
Transverse myelitis symptoms can develop rapidly over the course of hours to days and may affect:
- Motor function
- Sensation
- Autonomic functions like bladder and bowel control
It's important to note that the specific symptoms and their severity can vary significantly from person to person, depending on factors such as the location and extent of spinal cord inflammation. Some may experience milder, transient symptoms, while others may have a rapid onset of paralysis and long-term impairments.
Early Symptoms
- Sharp or shooting back pain
- Tingling or numbness in legs or arms
- Muscle weakness, heaviness, or stiffness in the limbs
Neurological Symptoms
As the condition progresses, individuals with transverse myelitis may experience:
- Loss of sensation, such as the inability to feel temperature, touch, or pain below the affected spinal cord level.
- Reflex changes, with reflexes becoming either exaggerated or diminished.
- Partial or complete paralysis of the muscles below the level of spinal inflammation.
- Difficulty in balancing and walking.
Bladder and Bowel Symptoms
TM can also impact autonomic functions controlled by the spinal cord, leading to:
- Urinary urgency, frequency, or retention
- Bowel incontinence or severe constipation
If you notice any of these symptoms, it's crucial to seek medical attention promptly for an accurate diagnosis and appropriate treatment.
Causes of Transverse Myelitis
While the exact mechanisms behind TM are not fully understood, researchers believe that most cases involve some form of abnormal immune system response that leads to spinal cord inflammation. Some of the main identified transverse myelitis causes include:
Autoimmune Disorders
Conditions such as multiple sclerosis (MS) and neuromyelitis optica (NMO) can cause transverse myelitis. In these diseases, immune-mediated attacks lead to inflammation and demyelination (loss of the protective myelin sheath), which disrupts nerve signalling in the spinal cord. These autoimmune neurological disorders can have a significant impact on an individual's quality of life, requiring ongoing management and support.
Infections
Certain infections can trigger TM, either through direct inflammation or by prompting an abnormal immune response. These include:
- Viral infections like herpes viruses, influenza, Zika virus, and HIV
- Bacterial infections such as syphilis, Lyme disease, and tuberculosis
Post-Vaccination Immune Response (Extremely Rare)
In exceedingly rare cases, transverse myelitis has been temporally associated with certain vaccinations, though a direct causal link is not established, such as those for influenza, hepatitis B, and measles-mumps-rubella (MMR). When this occurs, it is thought to be the result of an abnormal immune system response triggered by the vaccine.
It's crucial to note that these cases are exceedingly uncommon, and the risk of developing TM from a vaccine is far lower than the risks associated with the infections they prevent.
Other Causes
Less commonly, TM may be linked to direct spinal cord compression, injury, or certain cancers. In some cases, despite thorough evaluation, no specific underlying cause is identified (idiopathic TM). According to the National Institutes of Health (NIH), transverse myelitis affects approximately 1 to 8 individuals per million per year, with 15–30% of cases classified as idiopathic.
Risk Factors for Transverse Myelitis
- Age: TM can occur at any age but shows bimodal peaks between 10–19 years and 30–39 years, although it can occur at any age.
- Viral infections: Having a recent or concurrent viral infection appears to increase the risk of developing TM.
- Family history of autoimmune disorders: Individuals with a family history of autoimmune neurological disorders, like multiple sclerosis or other autoimmune conditions, may have a genetic predisposition to TM.
Complications of Transverse Myelitis
The complications experienced by individuals with transverse myelitis can vary widely depending on the severity and location of spinal cord inflammation. Some potential long-term effects may include:
- Chronic pain, particularly neuropathic pain, results from damage to the nervous system.
- Sexual dysfunction, including difficulties with arousal, sensation, or orgasm.
- Depression or anxiety related to the challenges of living with a chronic neurological condition.
- Permanent disability, such as partial or complete paralysis, sensory deficits, or loss of bladder/bowel control.
While some people with TM do experience significant recovery of function over time, others may have persistent neurological deficits that impact their daily activities and quality of life.
How Transverse Myelitis Is Diagnosed
Diagnosing transverse myelitis involves a step-by-step evaluation to assess neurological symptoms, localise spinal cord damage, and identify potential causes:
1. Clinical Evaluation
Doctors will review your medical history and symptom progression, looking for hallmark signs like rapidly developing weakness, sensory changes, or bladder/bowel dysfunction.
2. Neurological Exam
A neurological exam for TM evaluates muscle strength, reflexes, and sensory responses to determine the level and extent of spinal cord involvement. This helps differentiate transverse myelitis from other neurological disorders by identifying patterns of weakness, sensory loss, and abnormal reflexes that correspond to specific spinal cord areas.
3. MRI Scan
MRI scans play a key role in diagnosing transverse myelitis. They provide detailed images that can reveal regions of spinal cord inflammation and swelling. MRI scan not only helps confirm the presence of TM but also aids in excluding other causes of neurological symptoms, such as structural lesions like tumours or herniated discs, or vascular problems. Additionally, MRI patterns may point to associated conditions such as multiple sclerosis or neuromyelitis optica spectrum disorders.
Also Read: Spinal Tumors: Symptoms, Causes, and Risk Factors
4. Lumbar Puncture (Spinal Tap)
In a lumbar puncture, a small sample of cerebrospinal fluid (CSF) is collected from the lower back for laboratory analysis. CSF tests can uncover signs of inflammation, including elevated white blood cell counts or protein levels. Specific CSF findings, like oligoclonal bands, may signify an autoimmune condition. Lumbar puncture also helps rule out infections that can mimic transverse myelitis symptoms.
5. Blood Tests
Blood Test provides valuable information for TM diagnosis:
- Check for autoimmune markers (e.g., aquaporin-4 antibodies, ANA)
- Screen for recent or ongoing infections (viral, bacterial, fungal, or parasitic)
- Rule out metabolic or systemic diseases that might mimic TM symptoms
Treatment for Transverse Myelitis
Prompt treatment is vital for reducing spinal cord inflammation, minimising damage, and promoting recovery in transverse myelitis. Therapeutic approaches include:
Medications
- Corticosteroids: High-dose intravenous corticosteroids are typically administered to rapidly control spinal cord inflammation and limit tissue injury. Oral steroids are often continued after the initial treatment.
- Plasma exchange (PLEX): For patients who do not respond adequately to corticosteroids, PLEX may be considered within 2 weeks of onset to remove circulating autoantibodies and immune complexes.
- Immunosuppressive drugs: Medications that suppress immune system activity, such as mycophenolate or azathioprine, may be recommended for recurrent TM or cases linked to autoimmune disorders.
- Antiviral or antibiotic medications if an infection is identified.
- Pain management strategies for neuropathic pain and muscle spasms.
Physical and Occupational Therapy
Rehabilitation is a fundamental part of transverse myelitis treatment, helping patients regain strength, mobility, and independence. Physical therapists design exercise programmes to rebuild muscle function, improve flexibility, and prevent contractures. Occupational therapists focus on enhancing skills for daily activities and providing adaptive tools or modifications. Personalised therapy plans are essential for maximising recovery and quality of life after TM.
Pain Management
Many individuals with transverse myelitis experience chronic pain, including neuropathic pain and muscle spasms. Treatment typically involves a combination of medications such as anti-seizure drugs (gabapentin, pregabalin), antidepressants (amitriptyline, duloxetine), and muscle relaxants (baclofen, tizanidine). In cases of severe, refractory pain, opioids may be cautiously prescribed under specialist supervision.
Non-drug therapies like heat/cold application, massage, acupuncture, and relaxation techniques can provide additional relief. Working closely with a pain management specialist is key to developing an effective, personalised plan for TM-related pain.
Recovery and Prognosis
Recovery from transverse myelitis is highly variable. Some people recover fully, but about one-third are left with significant limitations, and another third have moderate residual symptoms. Recovery may take months to years, and early treatment is linked to better outcomes. Severe cases may result in lasting loss of function, such as paralysis or ongoing bladder/bowel problems.
Prevention Tips
Transverse myelitis often occurs as a complication of autoimmune disorders, infections, or other underlying conditions. Hence, complete prevention may not always be possible. However, some measures can reduce risk or aid early detection:
- Stay up to date with recommended vaccinations (e.g., measles, influenza, COVID-19) to reduce infection-related risk factors.
- Promptly treat autoimmune neurological disorders that could trigger inflammation.
- Regular health checkups to monitor and manage underlying risk factors.
- A healthy lifestyle with a balanced diet rich in vitamins and minerals, and regular exercise.
When to Seek Medical Help
Transverse myelitis often develops rapidly, necessitating quick medical attention. Warning signs include:
- Sudden weakness or paralysis in the legs or arms
- Numbness or tingling that spreads across the body
- Shooting pain in the back, arms, legs, or torso
- Loss of bladder or bowel control
If you experience these symptoms, go to the emergency room or call your doctor immediately. Swift diagnosis and treatment are essential for preventing permanent damage and improving outcomes in transverse myelitis.
Conclusion
Transverse myelitis is a rare but serious neurological condition that requires prompt diagnosis and treatment to minimise the risk of long-term disability. By understanding the symptoms, causes, and diagnostic process for TM, you can be better prepared to develop an effective treatment plan. With a combination of medical interventions, rehabilitation, and ongoing support, many individuals with transverse myelitis can achieve significant recovery and maintain a good quality of life.
Metropolis Healthcare, one of India's leading diagnostic service providers, offers a comprehensive suite of over 4,000 tests and profiles, ranging from routine diagnostics to highly specialised tests for neurological disorders, infectious diseases, and genetic conditions. Our expert phlebotomists provide a convenient home sample collection option for blood tests that can help identify autoimmune disorders or infections related to TM. To learn more about our services or schedule a health checkup, visit our website or download the Metropolis Healthcare App.
FAQs
1. Is transverse myelitis curable?
Currently, there is no cure for transverse myelitis. However, early and aggressive treatment can significantly enhance recovery and help manage ongoing symptoms. The goal of treatment is to reduce spinal cord inflammation, minimise dysfunction, and prevent recurrent episodes.
2. What triggers transverse myelitis?
Transverse myelitis causes include autoimmune reactions, viral or bacterial infections, or sometimes unknown factors (idiopathic cases). Infections often precede the onset, but sometimes no specific trigger can be identified.
3. Can transverse myelitis cause permanent disability?
Yes, permanent disability can occur, especially if treatment is delayed or the initial attack is severe. Some people are left with persistent weakness, sensory loss, or bladder/bowel dysfunction. Early diagnosis and treatment are critical for minimising long-term impacts and optimising function.
4. How long does it take to recover from transverse myelitis?
TM recovery varies greatly from person to person. Some people improve within a few months, while others take up to several years. Only about one-third of patients recover fully, emphasising the importance of timely care and comprehensive rehabilitation.
5. What's the difference between transverse myelitis and multiple sclerosis?
Multiple sclerosis (MS) is a chronic, relapsing disease primarily affecting the brain and spinal cord, while transverse myelitis is often a single, isolated event. TM can occur by itself or as part of other neurological syndromes, including MS. Transverse myelitis typically involves both sides of the spinal cord; MS lesions can be scattered and less extensive.
References
- https://my.clevelandclinic.org/health/diseases/8980-transverse-myelitis
- https://www.ncbi.nlm.nih.gov/books/NBK559302/
- https://www.ninds.nih.gov/health-information/disorders/transverse-myelitis
- https://medlineplus.gov/ency/article/007766.htm




























