Preventive Healthcare
Small Intestine: Purpose, Procedure & Understanding Your Results
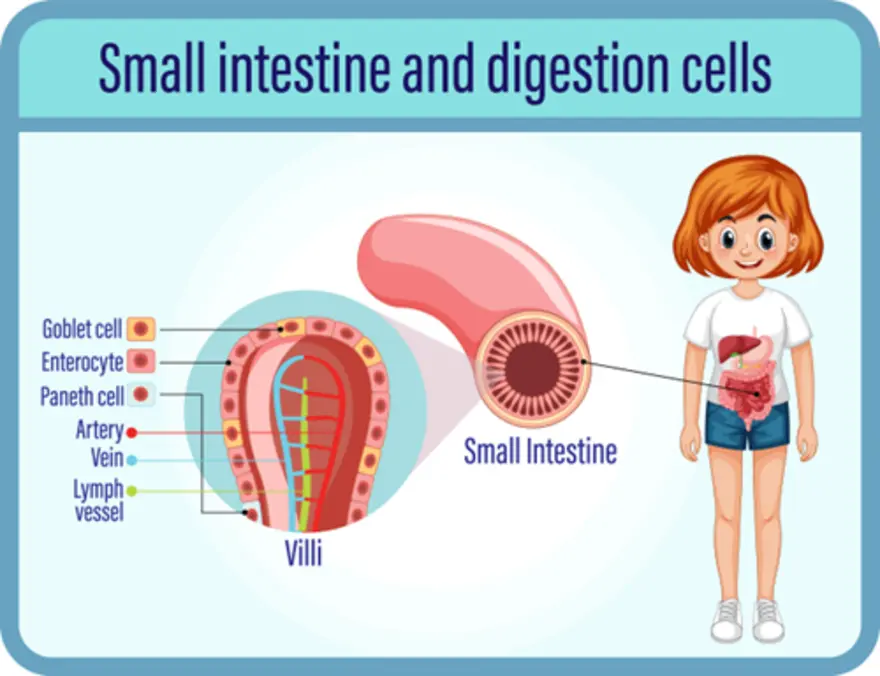
Table of Contents
- What Is the Small Intestine?
- Anatomy and Structure of the Small Intestine
- Functions of the Small Intestine
- Common Disorders of the Small Intestine
- Procedures Involving the Small Intestine
- Understanding Your Results
- Tests Used to Diagnose Small Intestine Disorders
- Prevention and Maintaining Small Intestine Health
- Conclusion
- FAQs
- References
What Is the Small Intestine?
The small intestine is a long, coiled tube that connects your stomach to the large intestine, serving as the primary site for nutrient digestion and absorption. Despite its name, the small intestine is actually longer than the length of the large intestine. The small intestine's length reaches 6–7 metres in adults. This vital organ processes the semi-digested food mixture called chyme that arrives from your stomach.
When food enters the small intestine, digestive enzymes from the pancreas and bile from the liver work together to break down proteins, fats, and carbohydrates into smaller molecules. The small intestine then absorbs these nutrients, along with vitamins, minerals, and water, into your bloodstream.
Anatomy and Structure of the Small Intestine
- The small intestine's anatomy is divided into three distinct sections, each with specialised functions:
- Duodenum: The first section, approximately 20-25 cm long, receives chyme from the stomach and digestive juices from the pancreas and liver
- Jejunum: The middle section, specialised for nutrient absorption through its rich, vascular lining with numerous folds
- Ileum: The final section, responsible for absorbing vitamin B12, bile salts, and any remaining nutrients
- The small intestine includes several remarkable features that maximise absorption:
- Plicae circulares: Circular folds that increase the surface area for nutrient absorption
- Villi: Tiny finger-like projections that further expand the absorptive surface
- Microvilli: Microscopic extensions on the villi that create a "brush border" effect
The wall structure consists of four layers: the outer serosa, muscular layers for movement, connective tissue with blood vessels, and the inner mucosa where absorption occurs. The mesentery anchors the small intestine to your abdominal wall, providing essential blood supply and nerve connections.
Functions of the Small Intestine
The primary function of the small intestine is to complete food digestion and absorb the nutrients your body needs for energy, growth, and repair. This process begins when partially digested food enters from your stomach, mixed with powerful digestive enzymes and bile that break down complex molecules into absorbable units.
The small intestine's specialised lining, with its extensive network of villi and microvilli, creates an enormous surface area - roughly equivalent to a tennis court when fully spread out. This remarkable design ensures maximum nutrient absorption, allowing amino acids, simple sugars, fatty acids, vitamins, and minerals to enter your bloodstream efficiently. Beyond digestion, the small intestine also supports immune defence and produces hormones that regulate digestion and energy balance throughout your body.
Common Disorders of the Small Intestine
Several conditions can affect the small intestine, often causing abdominal pain and digestive symptoms:
- Coeliac disease: As per ICMR, the small intestine is the organ most often affected in patients with coeliac disease, an autoimmune reaction to gluten that damages the intestinal lining.
- Crohn's disease: A type of inflammatory bowel disease causing chronic inflammation
- Small intestinal bacterial overgrowth (SIBO): Excessive bacteria in the small intestine
- Intestinal obstruction: Blockage preventing normal food passage
- Malabsorption syndromes: Conditions affecting nutrient absorption
- Peptic ulcers: Open sores in the duodenum
- Small intestine cancer: Though rare, can develop in any section
- Infections: Including gastroenteritis and parasitic infections
- Irritable bowel syndrome (IBS): Functional disorder affecting digestion
- Lactose intolerance: Inability to digest milk sugar properly
Also Read: Bowel Cancer : Symptoms, Treatments, Risk & Diagnosis
Procedures Involving the Small Intestine
Medical procedures for examining the small intestine have advanced significantly, offering doctors detailed views of this complex organ.
- Endoscopy procedures, including upper endoscopy and specialised techniques like double-balloon enteroscopy, allow direct visualisation and tissue sampling from different parts of the small intestine.
- Capsule endoscopy involves swallowing a small camera that travels through your digestive tract, capturing thousands of images.
- Imaging studies such as CT enterography and MRI provide detailed views of the small intestine’s anatomy and surrounding structures. These procedures help identify inflammation, tumours, obstructions, and other abnormalities.
- When necessary, surgical procedures may be performed to remove diseased sections, clear obstructions, or obtain tissue samples for further analysis.
Understanding Your Results
Interpreting small intestine test results requires understanding what each finding means for your digestive health. Normal results typically show healthy tissue structure, appropriate nutrient absorption levels, and an absence of inflammation or abnormal growths. However, abnormal findings might indicate various conditions affecting the small and large intestine.
Blood test abnormalities, such as anaemia or elevated inflammatory markers, can suggest malabsorption or inflammatory conditions. Imaging studies might reveal structural changes, while endoscopic findings could show tissue damage, ulcers, or unusual growths. Biopsy results provide a definitive diagnosis for conditions like coeliac disease or cancer.
How Is the Small Intestine Examined?
- Upper endoscopy (EGD): Visualises the duodenum and allows for biopsy collection
- Capsule endoscopy: Provides complete small intestine imaging through a swallowable camera
- Double-balloon enteroscopy: Enables deeper examination and therapeutic interventions
- CT and MRI scans: Assess structure, detect obstructions, and identify abnormalities
- Small bowel follow-through: X-ray study using contrast material to evaluate function
- Blood tests: Check for anaemia, nutritional deficiencies, and inflammatory markers
- Stool tests : Detect infections, malabsorption, or blood presence
What Are the Symptoms of Small Intestine Problems?
- Persistent abdominal pain: Often cramping or aching; may worsen after eating
- Bloating and excessive gas: Often occurring after meals or certain foods
- Chronic diarrhoea or constipation: Changes in bowel habits lasting weeks
- Unintentional weight loss: Despite maintaining normal eating habits
- Fatigue and weakness: Often due to nutrient malabsorption
- Nausea and vomiting: Especially if obstruction is present
- Blood in stool: May appear bright red or dark and tarry
- Greasy, foul-smelling stools: May indicate fat malabsorption
- Signs of malnutrition: Including hair loss, brittle nails, or skin changes
If you experience persistent abdominal pain or several of these symptoms, consult your healthcare provider promptly.
Tests Used to Diagnose Small Intestine Disorders
Comprehensive diagnosis often requires multiple tests to evaluate the small and large intestine:
- Complete Blood Count (CBC): Detects anaemia, infection, or other blood abnormalities
- C-Reactive Protein test: Measures inflammation levels in your digestive tract
- Erythrocyte Sedimentation Rate (ESR): Another inflammatory marker often elevated in intestinal disorders
- Stool tests: Identify infections, blood presence, or fat malabsorption indicators
- Histopathological examination of small intestine resection: Analyses tissue removed during surgery for cancer or severe disease
- Histopathological examination of GI endoscopic biopsy: Studies tissue samples obtained during endoscopy procedures
Treatment Options for Small Intestine Disorders
- Dietary modifications: Such as gluten-free diets for coeliac disease or lactose-free diets for intolerance
- Medications: Including anti-inflammatory drugs, antibiotics, or immunosuppressants as needed
- Surgical interventions: For obstructions, tumours, or severe inflammatory conditions
- Nutritional supplementation: To address vitamin and mineral deficiencies from malabsorption
- Probiotic therapy: To restore healthy gut bacteria balance
- Enzyme replacement therapy: For conditions affecting digestive enzyme production
Prevention and Maintaining Small Intestine Health
Maintaining optimal small intestine health involves adopting healthy lifestyle practices that support proper digestion and nutrient absorption. A balanced diet rich in fibre, fruits, vegetables, and lean proteins provides essential nutrients while promoting healthy gut bacteria. Staying adequately hydrated helps maintain the mucus lining that protects your intestinal walls.
Regular medical check-ups help identify potential issues early, and managing chronic conditions like diabetes reduces your risk of developing secondary digestive complications. Understanding the connection between the small and large intestine also helps you recognise when symptoms might indicate problems requiring medical attention.
Conclusion
Understanding your small intestine's vital role in digestion empowers you to recognise potential problems early and seek appropriate medical care. Whether you're experiencing abdominal pain, digestive symptoms, or simply want to maintain optimal gut health, remember that early detection and proper treatment significantly improve outcomes.
At Metropolis Healthcare, we support your digestive health journey with comprehensive diagnostic testing. Our extensive portfolio of over 4,000 tests includes specialised assessments for small intestine disorders, from basic blood work to advanced inflammatory markers. Our qualified technicians ensure comfortable home sample collection, while our advanced laboratories deliver accurate results through our user-friendly Metropolis Healthcare app.
FAQs
What Is the Role of the Small Intestine in Digestion?
The small intestine breaks down food and absorbs most of your nutrients. Enzymes and bile help convert proteins, fats, and carbohydrates into forms your body can use for energy and repair.
What Are Common Symptoms of Small Intestine Issues?
Key symptoms include abdominal pain, bloating, chronic diarrhoea, weight loss, nausea, fatigue, and signs of nutrient deficiencies. Persistent symptoms should be medically evaluated.
How Is the Small Intestine Treated?
Treatment depends on the condition. It may involve dietary changes, medications, or surgery, for example, a gluten-free diet for coeliac disease, anti-inflammatory drugs for Crohn’s, or surgery for obstructions.
What Does It Mean If I Have a Small Intestine Disorder?
It means a condition is affecting digestion or nutrient absorption. It can range from mild issues like lactose intolerance to more serious diseases. Early diagnosis helps prevent complications.
What Is Dumping Syndrome?
Dumping syndrome happens when food moves too quickly from the stomach to the small intestine, usually after stomach surgery. It causes nausea, pain, diarrhoea, dizziness, and a rapid heartbeat after meals.
How Can Dumping Syndrome Be Treated?
Treatment includes smaller, frequent meals, limiting sugary foods, increasing fibre and protein, and drinking fluids between meals. Severe cases may require medication to slow digestion and ease symptoms.
References
- https://www.icmr.gov.in/icmrobject/custom_data/pdf/resource-guidelines/ICMR%20-%20Diagnosis%20and%20Managmemnt.pdf
- https://my.clevelandclinic.org/health/body/22135-small-intestine
- https://www.chp.edu/our-services/transplant/intestine/education/about-small-large-intestines
- https://www.verywellhealth.com/small-intestine-problems-5210173
- https://www.ncbi.nlm.nih.gov/books/NBK459366/




























