Preventive Healthcare
Organ Failure: Types, Causes & Life-Saving Interventions
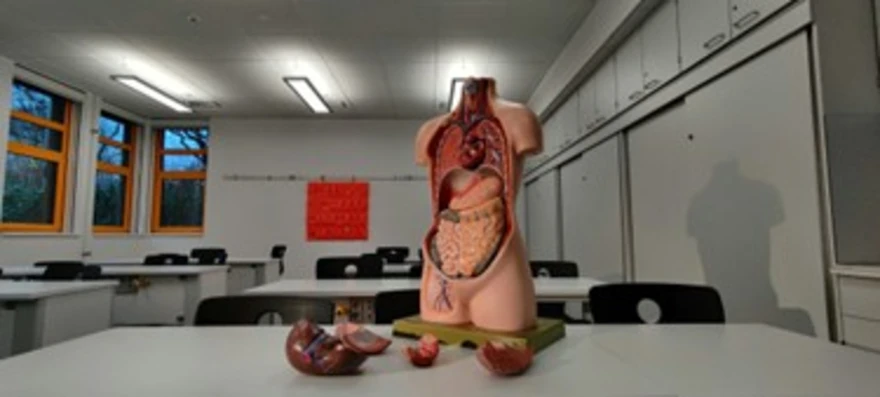
Table of Contents
- What is Organ Failure?
- Types of Organ Failure
- Major Organs Commonly Affected
- Early Signs and Symptoms of Organ Failure
- Causes and Risk Factors of Organ Failure
- Complications Associated with Organ Failure
- Diagnosis of Organ Failure
- Examinations and Tests to Diagnose Organ Failure
- Treatment & Life-Saving Interventions for Organ Failure
- Prevention of Organ Failure
- Prognosis and Recovery Outlook
- When to Seek Emergency Medical Help
- Global and Local Perspectives on Organ Failure Care
- Living with Organ Failure: Lifestyle and Support Tips
- Conclusion
- FAQs
- References
What is Organ Failure?
Organ failure refers to the inability of one or more vital organs—such as the heart, lungs, liver, kidneys, or brain—to maintain normal physiological function required for homeostasis. Each organ has a specific role in maintaining your body’s balance.
For instance, your kidneys filter waste, the liver detoxifies blood, and the lungs deliver oxygen. When one of these organs stops functioning properly, toxins build up, circulation slows, and oxygen levels fall, putting every other organ at risk.
In simple terms, organ failure signals that a vital system of the body is no longer sustaining normal life functions. It may develop suddenly due to infection or trauma (acute organ failure), or gradually over years because of chronic diseases such as diabetes or hypertension (chronic organ failure).
Types of Organ Failure
Organ failure is not uniform—it varies depending on the number of organs affected and the speed of onset.
Understanding the types can help in timely recognition and treatment:
- Acute Organ Failure: Occurs suddenly, often due to infection, injury, or a drug reaction. If treated promptly, it can be reversible.
- Chronic Organ Failure: Develops over time, such as chronic kidney disease or congestive heart failure, where gradual deterioration leads to loss of function.
- Single-Organ Failure: Involves failure of one organ, such as liver failure due to hepatitis or heart failure due to coronary artery disease.
- Multiple Organ Dysfunction Syndrome (MODS): When two or more organ systems fail simultaneously, often due to sepsis or trauma. MODS is the preferred clinical term replacing ‘Multiple Organ Failure’ in current intensive care medicine, often due to sepsis or trauma. It’s the most severe form and requires intensive care support.
Major Organs Commonly Affected
Several vital organs are susceptible to failure, each with its own set of consequences:
- Heart: Responsible for pumping blood and maintaining circulation. When it fails, oxygen delivery to other organs drops, leading to fatigue, breathlessness, and oedema.
- Lungs: Facilitate oxygen and carbon dioxide exchange. According to the NIH, respiratory failure occurs when blood oxygen levels fall (hypoxemia) or carbon dioxide levels rise (hypercapnia), leading to respiratory distress.
- Liver: Processes nutrients and detoxifies chemicals. Liver failure causes jaundice, confusion, and bleeding disorders.
- Kidneys: Filter toxins and maintain fluid-electrolyte balance. Kidney failure leads to fluid retention, high potassium levels, and decreased urine output.
- Brain: Controls bodily functions. Neurological failure due to stroke, trauma, or hypoxia can lead to loss of consciousness, coma, or brain death.
Early Signs and Symptoms of Organ Failure
Recognising the organ failure symptoms early can make all the difference between recovery and progression.
Some common warning signs include:
- Persistent fatigue and weakness: A universal symptom across all organ systems.
- Shortness of breath: Often indicates cardiac or pulmonary compromise.
- Swelling in legs, ankles, or abdomen: Suggests heart or kidney issues.
- Reduced urine output: Common in kidney failure.
- Yellowing of eyes or skin (jaundice): Typical of liver dysfunction.
- Confusion or disorientation: May occur with liver, brain, or oxygen deprivation issues.
- Rapid or irregular heartbeat: Linked to cardiac arrhythmias or electrolyte imbalance.
Causes and Risk Factors of Organ Failure
Organ failure can arise from a variety of internal diseases or external triggers that disrupt the body’s normal functioning.
Common Causes:
- Infections: Severe infections like sepsis or pneumonia can trigger a chain reaction leading to organ shutdown.
- Chronic illnesses: Uncontrolled diabetes, hypertension, and obesity put constant stress on organs such as the kidneys and heart.
- Autoimmune diseases: Conditions like lupus can cause inflammation that damages vital organs.
- Drug or alcohol abuse: Chronic drug or alcohol misuse can cause toxic damage to the liver, heart, pancreas, and nervous system.
- Dehydration or blood loss: Leads to reduced oxygen and nutrient supply to organs.
- Toxic exposure: Industrial chemicals, pollution, and certain medications can poison organs.
Risk Factors:
Ageing, smoking, poor diet, stress, sedentary lifestyle, and genetic predispositions all raise your likelihood of developing organ failure. The ICMR recommends periodic health screenings and lifestyle modifications to detect and prevent disease progression.
Complications Associated with Organ Failure
When an organ fails, its function is either taken over partially by other organs or completely lost. This imbalance strains your body, often leading to further complications such as:
- Multiple Organ Dysfunction (MODS): Progressive failure of two or more organ systems secondary to an uncontrolled inflammatory or septic response.
- Sepsis and infection: Poor immune response can trigger systemic infections.
- Fluid overload: Common in heart or kidney failure, resulting in pulmonary congestion, swelling (edema), and breathlessness.
- Metabolic imbalances: Electrolyte disturbances or acid-base disorders.
- Coma or brain dysfunction: Particularly in liver or respiratory failure.
Diagnosis of Organ Failure
Doctors diagnose organ failure using a step-by-step approach that combines medical history, physical assessment, and lab investigations:
- Clinical Evaluation: Identifying symptoms like swelling, breathlessness, or jaundice.
- Vital Sign Monitoring: Measuring blood pressure, oxygen levels, and heart rate.
- Laboratory Tests: Complete Blood Count (CBC) and Urinalysis (Routine and Microscopic Examination) help identify infection, anemia, and renal abnormalities.
- Imaging: Ultrasound, CT, or MRI scans to assess structural changes.
- Functional Tests: ECG for the heart, spirometry for the lungs, and Renal Function Tests (RFT) Maxi for the kidneys.
- Biopsy: In some cases, tissue samples help confirm chronic disease or organ damage.
Examinations and Tests to Diagnose Organ Failure
A range of advanced diagnostic panels and speciality tests help assess how well your organs are functioning:
- Liver Function Test (LFT): Evaluates enzyme levels to detect liver inflammation or damage.
- Kidney Function Test (KFT): Measures creatinine and urea to assess renal health.
- Cardiac Risk Marker Panel: Detects early heart disease and risk of heart failure.
- Thyroid Profile Test: Monitors metabolism, which affects multiple organ functions.
- Electrolyte Test: Checks sodium, potassium, and calcium levels essential for cell function.
- CBC Test: Helps identify infections and anaemia affecting oxygen transport.
Treatment & Life-Saving Interventions for Organ Failure
Treatment varies depending on which organ has failed and how severe the damage is. The primary goal is to restore function, prevent complications, and support recovery.
Emergency Supportive Care
- Administration of oxygen or mechanical ventilation in respiratory distress
- Intravenous fluids to maintain blood pressure and circulation
- Dialysis for kidney failure to remove toxins
- Blood transfusions to restore oxygen capacity
- Intensive Care Unit (ICU) monitoring with continuous hemodynamic, respiratory, and neurological assessment for patients with multi-organ dysfunction
Medication & Organ-Specific Therapy
Medications help stabilise the failing organ and manage symptoms.
- Heart failure: Diuretics, beta-blockers, and ACE inhibitors improve heart efficiency.
- Kidney failure: Medications to control blood pressure and phosphorus levels.
- Liver failure: Managed with antivirals or immunosuppressants in hepatitis-related cases, and supportive therapy including lactulose and vitamin supplementation.
- Lung failure: Bronchodilators, steroids, and oxygen therapy.
Surgical & Transplant Options
If organ damage is irreversible, surgery or transplantation may be necessary.
- Kidney transplant or dialysis for end-stage renal failure.
- Liver transplant in cases of cirrhosis or acute hepatic failure.
- Heart bypass or transplant for severe cardiac conditions.
These advanced interventions can substantially improve both life expectancy and quality of life when performed under appropriate indications.
Rehabilitation & Long-Term Care
- Regular checkups and follow-up tests
- Diet counselling and physiotherapy
- Immunosuppressant management after transplants
- Emotional and psychological support
- Regular monitoring for secondary complications
Prevention of Organ Failure
Prevention begins with protecting your vital organs through lifestyle and health awareness:
- Eat a balanced diet rich in fruits, vegetables, and whole grains
- Maintain healthy blood pressure and glucose levels
- Avoid smoking, alcohol, and recreational drugs
- Exercise for at least 30 minutes a day
- Get adequate sleep and manage stress
- Schedule routine health screenings and full-body checkups
These preventive measures safeguard your organs long before disease sets in.
Prognosis and Recovery Outlook
The prognosis depends on which organ is affected and how early you begin treatment. Many acute organ failures are reversible, while chronic conditions may need lifelong management. With advances in critical care, organ support technologies, and transplantation, selected patients with multi-organ dysfunction can achieve meaningful recovery and improved quality of life.
When to Seek Emergency Medical Help
Seek urgent medical attention if you experience any of the following:
- Sudden shortness of breath or chest pain
- Rapid swelling of legs or abdomen
- Confusion or loss of consciousness
- Inability to urinate or reduced urine output
- Yellowing of skin or eyes
- Severe fatigue or fainting spells
Immediate care can prevent permanent damage or death.
Global and Local Perspectives on Organ Failure Care
Globally, organ failure remains a leading cause of hospitalisations, critical illness, and death. Access to advanced treatments like dialysis or transplantation varies significantly by country and region, with disparities in outcomes based on healthcare infrastructure, socioeconomic factors, and organ donation rates. Local health systems address organ failure through prevention, early detection, and critical care interventions to improve survival and quality of life.
Living with Organ Failure: Lifestyle and Support Tips
Living with organ failure requires patience, adherence, and emotional strength. You can improve your quality of life through small, consistent efforts:
- Follow your treatment and medication schedule strictly
- Stay in touch with your healthcare provider
- Eat nutrient-dense foods and limit processed items
- Join support groups for motivation and guidance
- Manage stress through yoga, meditation, or light exercise
- Undergo periodic diagnostic and functional monitoring to assess recovery and detect early relapse or secondary complications
Conclusion
Organ failure is a serious but often preventable condition. Early diagnosis, lifestyle changes, and regular testing can protect your vital organs and improve recovery chances.
With Metropolis Healthcare’s advanced technology, NABL & CAP accredited labs, and over 4,000 diagnostic tests, you can track your organ health accurately from the comfort of your home. Their home sample collection service across 10,000 touchpoints ensures quick results and peace of mind.
Visit the Metropolis Healthcare website or connect via app, call, or WhatsApp to book your comprehensive organ function checkup today.
FAQs
What happens when an organ fails?
When an organ fails, it loses its ability to perform its normal function. This leads to toxin buildup, fluid imbalance, and oxygen deficiency, which can eventually impact other organs.
Which organ failure is most common?
Heart and kidney failures are among the most common, often resulting from hypertension, diabetes, and lifestyle diseases.
Can organ failure be reversed?
Yes, especially if it’s detected early and treated aggressively. Acute organ failure cases may fully recover with supportive care and therapy.
How long can a person live with organ failure?
Life expectancy depends on the organ involved, severity, and treatment compliance. With proper care—like dialysis or transplantation—patients can live many years.
What is the first sign of organ failure?
- Extreme fatigue or weakness
- Shortness of breath
- Unexplained swelling
- Loss of appetite
How can you prevent organ failure naturally?
- Maintain a healthy diet.
- Exercise regularly
- Avoid smoking and alcohol
- Get regular health screenings
Is organ failure the same as organ damage?
No. Organ damage means partial dysfunction, whereas organ failure means complete loss of vital function.
How do doctors detect organ failure early?
Through screening tests like LFT, KFT, ECG, and imaging studies. Early testing identifies changes before symptoms worsen.
References
- https://www.ncbi.nlm.nih.gov/books/NBK554514/
- https://www.mayoclinic.org/diseases-conditions/multiple-organ-dysfunction-syndrome/symptoms-causes/syc-20354721
- https://www.kidney.org/atoz/content/OrganFailure
- https://www.hopkinsmedicine.org/health/conditions-and-diseases/multiple-organ-dysfunction-syndrome-mods
- https://www.nhs.uk/conditions/kidney-failure/
- https://www.webmd.com/a-to-z-guides/organ-failure-types-causes-symptoms-treatments
- https://www.nhlbi.nih.gov/health/respiratory-failure/causes




























