Preventive Healthcare
Gastrointestinal Bleeding: Signs, Causes & When It Becomes an Emergency
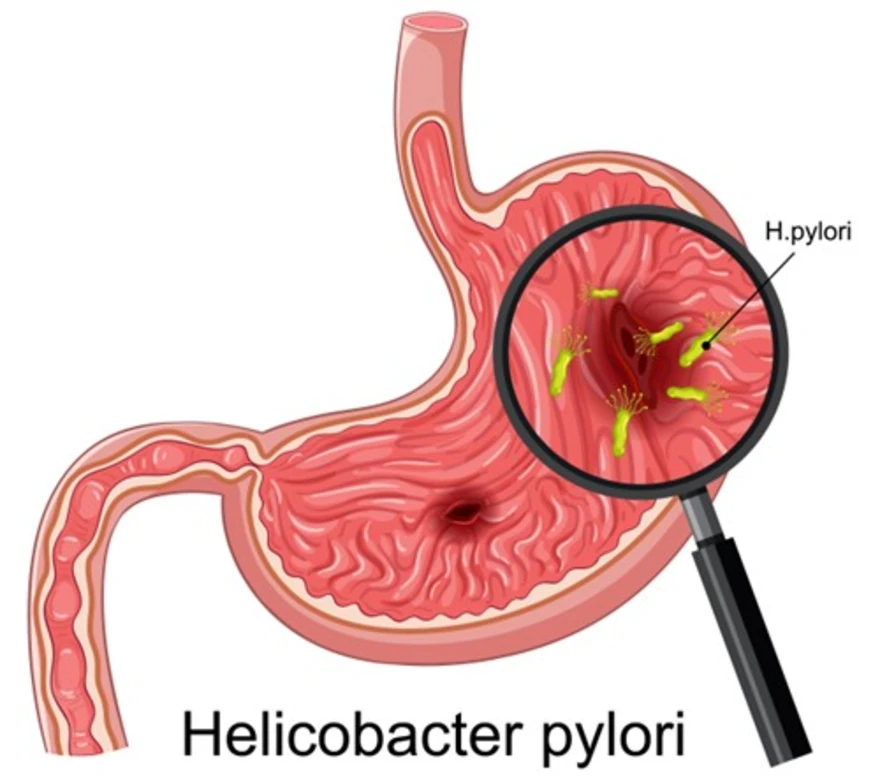
Table of Contents
- What is Gastrointestinal Bleeding?
- Signs and Symptoms of Gastrointestinal Bleeding
- Causes of Gastrointestinal Bleeding
- When Does Gastrointestinal Bleeding Become an Emergency?
- How is Gastrointestinal Bleeding Diagnosed?
- Tests Used to Diagnose Gastrointestinal (GI) Bleeding
- Treatment for Gastrointestinal Bleeding
- Prevention of Gastrointestinal Bleeding
- Conclusion
- FAQs
What is Gastrointestinal Bleeding?
Gastrointestinal bleeding refers to any bleeding that occurs within the digestive system, including the oesophagus, stomach, small intestine, large intestine, rectum, and anus. Rather than being a disease itself, a GI bleed represents a symptom of various underlying conditions affecting different parts of your digestive tract.
Medical professionals classify gastrointestinal bleeding into two main categories: upper gastrointestinal bleeding, which occurs proximal to the ligament of Treitz (upper GI) and distal to it (lower GI), and lower gastrointestinal bleeding, which happens in the colon, rectum, or anus. The severity can range from slow, chronic blood loss that develops gradually to sudden, severe bleeding requiring immediate emergency intervention.
Signs and Symptoms of Gastrointestinal Bleeding
Recognising GI bleed symptoms early can make a significant difference in treatment outcomes. The most common gastrointestinal bleeding symptoms include:
• Visible blood in stool — bright red blood or black, tarry stools (melena)
• Blood in vomit — fresh blood or coffee-ground appearance
• Unexplained fatigue and weakness — often due to slow, chronic blood loss leading to iron-deficiency anaemia
• Shortness of breath — suggesting possible anaemia
• Dizziness or lightheadedness — particularly when standing
• Rapid heartbeat — your body's response to blood loss
• Pale skin or gums — indicating reduced blood volume
• Abdominal pain or cramping — varying in intensity and location
How Do You Recognise Gastrointestinal Bleeding?
Are you wondering how to identify gastrointestinal bleeding in its early stages? Watch for these specific warning signs:
• Bright red blood on toilet paper after bowel movements
• Dark, sticky stools that appear black or maroon
• Vomiting blood or material resembling coffee grounds
• Sudden onset of weakness during daily activities
• Feeling faint when changing positions quickly
• Unexplained drop in energy levels over several days or weeks
Causes of Gastrointestinal Bleeding
Understanding GI bleed causes helps you identify risk factors and take preventive measures. The most common causes vary depending on the location within your digestive system.
Peptic ulcer disease remains the most common cause of upper GI bleeding, primarily due to Helicobacter pylori infection or chronic NSAID use of upper gastrointestinal bleeding, often developing due to Helicobacter pylori bacterial infection or prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs). For example, a 45-year-old teacher who regularly takes aspirin for headaches might develop stomach ulcers that eventually bleed.
Gastritis and esophagitis often result from alcohol use, chronic acid reflux, or certain medications (e.g., NSAIDs, corticosteroids), certain medications, or chronic acid reflux. Diverticular bleeding typically occurs when small arteries at the base of diverticula rupture — a common cause of painless lower GI bleeding in older adults.
Cancer and polyps anywhere along the digestive tract can erode blood vessels and cause bleeding. Angiodysplasia, involving abnormal blood vessel formation, most commonly affects the colon in elderly patients.
As per a 2023 study published in BMC Emergency Medicine (NIH), portal hypertension due to liver cirrhosis is a major cause of upper GI bleeding, with esophageal varices seen in more than half of affected patients.
Inflammatory Bowel Disease (IBD) and GI Bleeding
Inflammatory bowel diseases, including Crohn's disease and ulcerative colitis, cause chronic inflammation throughout the digestive tract. This persistent inflammation leads to ulcers and erosions that frequently bleed, ranging from mild spotting to severe haemorrhage requiring hospitalisation.
Patients with inflammatory bowel diseases often experience intermittent gastrointestinal bleeding episodes alongside other symptoms like abdominal pain, diarrhoea, and weight loss. Managing these conditions requires ongoing medical supervision and specialised treatment approaches.
Enlarged Spleen and GI Bleeding
While an enlarged spleen doesn't directly cause gastrointestinal bleeding, the underlying conditions creating spleen enlargement often lead to bleeding complications. Liver cirrhosis, for instance, increases pressure within the portal vein system, causing varices (swollen veins) in the oesophagus or stomach.
These varices carry a high rupture risk and can produce life-threatening bleeding episodes. Patients with liver disease require regular monitoring for signs of gastrointestinal bleeding and may need preventive treatments to reduce bleeding risk.
Haemorrhoids and Anal Fissures as Causes
Common causes of lower gastrointestinal bleeding include:
• Haemorrhoids - swollen blood vessels causing painless, bright red bleeding
• Anal fissures - small tears producing painful, bright red bleeding during bowel movements
• Inflammatory conditions affecting the rectum or anus
• Rectal polyps that may bleed intermittently
When Does Gastrointestinal Bleeding Become an Emergency?
Recognising when gastrointestinal bleeding becomes life-threatening helps you seek emergency care promptly. Immediate medical attention becomes crucial when you experience heavy, ongoing bleeding with large amounts of blood in vomit or stool.
Emergencies include sudden onset of dizziness, fainting, confusion, or loss of consciousness alongside bleeding symptoms. A rapid heart rate combined with low blood pressure indicates your body is struggling to maintain adequate blood circulation. Severe abdominal pain accompanying bleeding may suggest serious underlying complications.
How is Gastrointestinal Bleeding Diagnosed?
Healthcare providers follow a systematic approach to diagnose gastrointestinal bleeding:
- Complete medical history - Discussing symptoms, medications, and risk factors
- Physical examination - Checking vital signs, skin colour, and abdominal tenderness
- Laboratory tests - Measuring blood count, clotting function, and liver enzymes
- Imaging studies - Imaging studies such as CT angiography are often used to detect active bleeding when endoscopy is inconclusive
- Endoscopic procedures - Direct visualisation of the digestive tract
Tests Used to Diagnose Gastrointestinal (GI) Bleeding
Modern diagnostic techniques for identifying GI bleed sources include:
• Upper endoscopy - examining the oesophagus, stomach, and duodenum
• Colonoscopy - visualising the entire colon and rectum
• Capsule endoscopy - swallowing a tiny camera to examine the small intestines
• CT angiography - imaging active bleeding sites
• Tagged red blood cell scans - tracking bleeding using radioactive markers
• Blood tests - assessing anaemia severity and clotting disorders
Treatment for Gastrointestinal Bleeding
Gastrointestinal bleeding treatment depends on the bleeding source, severity, and underlying cause:
• Emergency stabilisation - IV fluids and blood transfusions for severe cases
• Endoscopic interventions - cautery, injection therapy, or clip placement
• Medications - proton pump inhibitors for ulcers, antibiotics for infections
• Surgical procedures - reserved for cases where other treatments fail
• Management of underlying conditions - treating inflammatory bowel diseases or liver disease
Prevention of Gastrointestinal Bleeding
Preventing gastrointestinal bleeding involves addressing modifiable risk factors:
• Use NSAIDs cautiously, especially if you have ulcer risk factors
• Treat H. pylori infections promptly when diagnosed
• Manage chronic conditions -Regular care for liver disease or inflammatory bowel disease
• Limit alcohol consumption - Reducing gastritis and liver damage risk
• Maintain a healthy diet - High-fibre foods prevent haemorrhoids and fissures
• Regular screening - Colon cancer screening as recommended by your doctor
Conclusion
Gastrointestinal bleeding is a warning sign that should never be ignored. Whether it appears as blood in vomit, black tarry stools, or persistent fatigue from slow blood loss, early recognition and diagnosis are essential to prevent complications like anaemia, infection, or shock. Knowing the signs, understanding the common causes, and seeking timely medical care can significantly improve outcomes and reduce the risk of emergencies.
For accurate evaluation and monitoring, Metropolis Healthcare offers over 4,000 tests, including full body checkups and specialised panels relevant to digestive health. Patients can opt for convenient home sample collection supported by 10,000+ touchpoints, with quick turnaround times and stringent quality controls for reliable results. Booking is simple via website, mobile app, phone call, or WhatsApp, making it easier to act quickly when gastrointestinal symptoms appear and to stay proactive about long-term digestive health.
FAQs
Is gastrointestinal bleeding serious?
Gastrointestinal bleeding severity ranges from minor to life-threatening conditions. Even small amounts of chronic bleeding can cause significant anaemia and impact your overall health. Sudden or severe bleeding requires immediate emergency care to prevent serious complications.
Can GI bleeding be treated without surgery?
Most gastrointestinal bleeding episodes respond well to non-surgical treatments, including medications, endoscopic procedures, and other minimally invasive interventions. Surgery becomes necessary only when these conservative approaches prove ineffective or in cases of severe, recurrent bleeding.
What happens if gastrointestinal bleeding is left untreated?
Untreated gastrointestinal bleeding can lead to severe anaemia, shock, organ failure, and potentially death, particularly with rapid or severe blood loss. Chronic undiagnosed bleeding may also indicate underlying cancers or other serious conditions requiring prompt medical attention.
How can I stop gastrointestinal bleeding at home?
• Never attempt self-treatment for significant gastrointestinal bleeding
• Seek immediate medical care if you notice blood in stool or vomit
• For minor rectal bleeding from haemorrhoids or fissures, maintain soft stools through adequate hydration and fibre intake
• Consult healthcare providers to confirm the bleeding source and receive appropriate treatment




























