Preventive Healthcare
Demyelinating Disease Explained: What You Need to Know
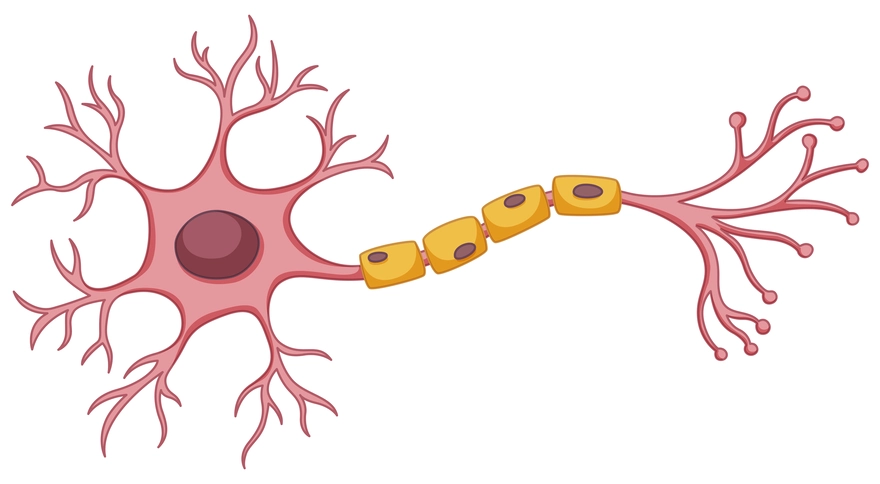
Table of Contents
- What Are Demyelinating Diseases?
- How Common Are Demyelinating Diseases?
- What Causes Demyelinating Diseases?
- Symptoms of Demyelinating Diseases
- Types of Demyelinating Diseases
- How Are Demyelinating Diseases Diagnosed?
- Treatment Options for Demyelinating Diseases
- Living With a Demyelinating Condition
- Prevention & Risk Reduction
- Conclusion: Prioritising Neurological Health
- FAQs
What Are Demyelinating Diseases?
Demyelinating diseases are neurological conditions characterised by damage to the myelin sheath surrounding nerve fibres in the central nervous system (brain and spinal cord) or, less commonly, the peripheral nervous system. Myelin acts as an insulator, enabling rapid and efficient transmission of electrical signals between nerve cells. When myelin is damaged or destroyed, the communication between the brain and other parts of the body is disrupted, leading to a wide range of neurological symptoms.
The damage to myelin can occur due to various factors, including autoimmune reactions, genetic predisposition, viral infections, and exposure to toxins. Depending on the specific disease and the areas of the nervous system affected, individuals may experience different symptoms and progression patterns.
How Common Are Demyelinating Diseases?
Demyelinating diseases, such as multiple sclerosis (MS), affect millions of people globally. MS, the most common demyelinating disorder, is estimated to affect over 2.8 million people worldwide, with a higher prevalence in women than men. The incidence of these conditions varies by geographic location and specific disease type, but they remain a significant health concern across all populations.
What Causes Demyelinating Diseases?
The exact causes of demyelinating diseases are not fully understood, but several factors are believed to contribute to their development:
- Autoimmune reactions: In some cases, the body's immune system mistakenly attacks and destroys healthy myelin, as seen in multiple sclerosis.
- Genetic predisposition: Having a family history of demyelinating disorders may increase an individual's risk of developing these conditions.
- Environmental factors: Exposure to certain viruses, such as Epstein-Barr virus, and low vitamin D levels have been associated with an increased risk of MS.
- Toxins: Exposure to toxins like organic solvents and heavy metals may contribute to myelin damage.
- Nutritional deficiencies: Vitamin B12 deficiency can cause demyelination and neurological symptoms, often reversible with timely treatment.
Symptoms of Demyelinating Diseases
The symptoms of demyelinating diseases can vary widely depending on the specific condition and the areas of the nervous system affected. Some common demyelinating disease symptoms include:
- Numbness, tingling, or weakness in the limbs
- Muscle stiffness and spasms
- Fatigue and decreased endurance
- Vision problems, such as blurred or double vision
- Difficulty with balance and coordination
- Bladder and bowel dysfunction
- Cognitive issues, including memory problems and difficulty concentrating
- Mood changes, such as depression or irritability
It's important to note that demyelinating disease symptoms can range from mild to severe and may come and go in episodes called relapses or exacerbations.
Types of Demyelinating Diseases
There are several types of demyelinating diseases, each with its own characteristics and patterns of myelin damage. Some of the most common demyelinating disease types include:
- Multiple Sclerosis (MS): MS is the most prevalent demyelinating disorder, affecting the brain, spinal cord, and optic nerves. It is characterised by the formation of scars or lesions in the central nervous system, leading to a wide range of neurological symptoms.
- Neuromyelitis Optica Spectrum Disorder (NMOSD): NMOSD primarily affects the optic nerves and spinal cord, causing inflammation and damage to myelin. It can lead to vision loss, weakness, and paralysis.
- Acute Disseminated Encephalomyelitis (ADEM): ADEM is a rare condition that typically occurs following a viral infection or vaccination. It causes widespread inflammation in the brain and spinal cord, leading to neurological symptoms.
- Transverse Myelitis: This condition involves inflammation of the spinal cord, resulting in weakness, sensory changes, and bladder or bowel dysfunction.
- Leukodystrophies: These are a group of inherited disorders that affect the production and maintenance of myelin, leading to progressive neurological deterioration.
Understanding the specific type of demyelinating disease is essential for determining the most appropriate treatment approach and managing the condition effectively.
How Are Demyelinating Diseases Diagnosed?
Diagnosing a demyelinating disease involves a combination of medical history, physical examination, and various diagnostic tests. Some common methods used to diagnose these conditions include:
- Magnetic Resonance Imaging (MRI): MRI scans detect areas of myelin damage (lesions) in the brain and/or spinal cord; lesion location, distribution, and enhancement patterns help distinguish between demyelinating disorders
- Lumbar Puncture (Spinal Tap): Analysis of the cerebrospinal fluid can reveal the presence of inflammation or specific antibodies associated with certain demyelinating diseases.
- Evoked Potentials: These tests measure the electrical activity in the brain in response to visual, auditory, or sensory stimuli, helping to assess the function of the nervous system.
- Blood Tests: Blood work can help rule out other conditions that may mimic the symptoms of demyelinating diseases and can also detect the presence of specific antibodies.
A thorough evaluation by a neurologist is essential for accurately diagnosing and determining the most appropriate demyelinating disease treatment plan.
Treatment Options for Demyelinating Diseases
Treatment for demyelinating diseases depends on the specific type and severity of the condition.
Some common demyelinating disease treatment approaches include:
- Disease-Modifying Therapies (DMTs): These medications, often used in multiple sclerosis, help to reduce the frequency and severity of relapses and slow the progression of disability.
- Corticosteroids: High-dose corticosteroids, such as methylprednisolone, can be used to reduce inflammation and manage acute relapses.
- Symptom Management: Medications and therapies can be used to address specific symptoms, such as muscle relaxants for spasticity, pain relievers for neuropathic pain, and bladder management techniques for urinary dysfunction.
- Rehabilitation: Physical therapy, occupational therapy, and speech therapy can help individuals maintain function, adapt to limitations, and improve their quality of life.
- Lifestyle Modifications: Adopting a healthy lifestyle, including a balanced diet, regular exercise, stress management, and adequate sleep, can help manage symptoms and promote overall well-being.
Living With a Demyelinating Condition
Managing a demyelinating disease requires a comprehensive approach that includes:
- Regular medical follow-up and adherence to prescribed treatments
- Engaging in physical and occupational therapy to maintain mobility and independence
- Making lifestyle adjustments, such as maintaining a balanced diet, managing stress, and avoiding smoking
- Seeking support through counseling and patient support groups
- Monitoring for and promptly addressing new symptoms or relapses
Working closely with your healthcare team and building a strong support network can help you navigate the challenges and optimise your quality of life.
Prevention & Risk Reduction
While some demyelinating diseases causes are not preventable, there are steps you can take to reduce your risk:
- Avoid exposure to environmental toxins and chemicals whenever possible.
- Maintain adequate levels of vitamin B12 through a balanced diet or supplements if needed.
- Take steps to prevent infections, such as staying up to date on vaccinations and practicing good hygiene.
- If you have a family history of demyelinating diseases, consider genetic counseling to understand your risk.
- Adopt healthy lifestyle habits, including a nutritious diet, regular exercise, and avoiding smoking and excessive alcohol consumption.
Conclusion: Prioritising Neurological Health
Demyelinating diseases are complex neurological disorders that can have a significant impact on daily life. However, with early diagnosis, appropriate treatment, and a proactive approach to management, it is possible to maintain a good quality of life. Staying informed about your condition, working closely with your healthcare team, and prioritising your overall health and well-being are key to navigating this journey successfully.
If you have concerns about demyelinating disease symptoms or are seeking reliable diagnostic services, consider reaching out to Metropolis Healthcare. As a leading chain of diagnostic labs across India, Metropolis offers accurate pathology testing and health check-up services. Our team of qualified blood collection technicians can perform at-home visits for your convenience, and test reports are easily accessible online. With a commitment to delivering reliable results and personalised care, Metropolis Healthcare can be a valuable partner in your neurological health journey.
FAQs
How does an MRI detect a demyelinating disease?
MRI scans use powerful magnets and radio waves to create detailed images of the brain and spinal cord. In individuals with demyelinating diseases, MRI can detect areas of myelin damage or lesions, which appear as bright or dark spots on the scan. The location and pattern of these lesions can help doctors diagnose the specific type of demyelinating disorder.
What is the life expectancy for a demyelinating disease?
Life expectancy with demyelinating diseases varies by condition, severity, and treatment. Early diagnosis and proper management help many live long, productive lives. However, aggressive forms like severe multiple sclerosis may significantly reduce life expectancy in some individuals.
Is demyelination life-threatening?
Demyelination itself isn't typically life-threatening, but complications from demyelinating diseases can be serious. Severe muscle weakness or paralysis may cause respiratory issues or higher infection risk. However, with proper treatment and ongoing care, most individuals can manage symptoms effectively and maintain a good quality of life over time.
Can demyelination be cured?
There is currently no cure for most demyelinating diseases, but some causes (e.g., B12 deficiency, certain infections) are reversible if treated promptly. Proper medications, physical therapy, and lifestyle changes help manage symptoms. In some cases, the nervous system can partially repair myelin.
Can you have demyelination without having MS?
Yes, demyelination can occur without having multiple sclerosis (MS). Other demyelinating disease causes include infections, autoimmune diseases (like lupus), metabolic disorders, certain medications, toxins, and conditions such as neuromyelitis optica or acute disseminated encephalomyelitis (ADEM). While MS is a common cause, it’s not the only one. Accurate diagnosis is essential to determine the underlying condition and guide treatment.




























