Preventive Healthcare
Babesiosis: A Complete Guide to This Tick-Borne Infection
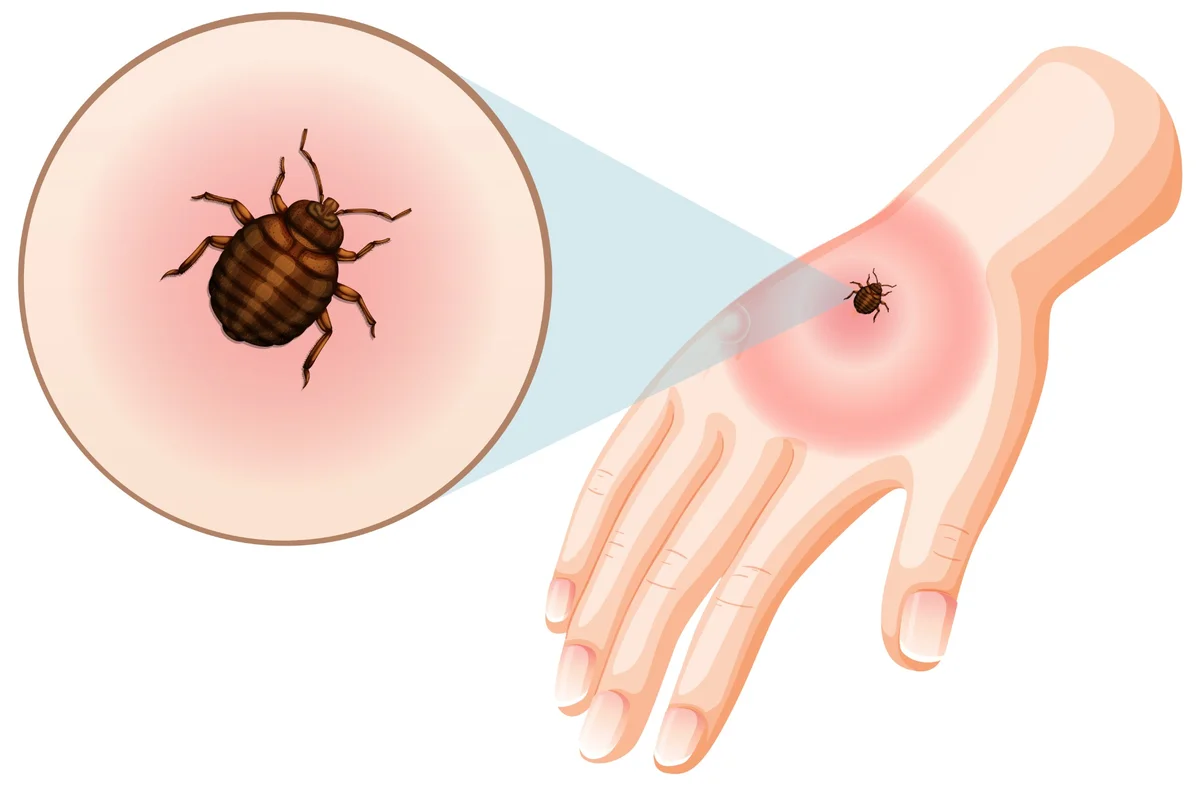
Table of Contents
- What Is Babesiosis?
- How Babesiosis Spreads
- Where Is Babesiosis Found?
- Babesiosis Symptoms
- Causes & Pathophysiology
- Risk Factors for Severe Babesiosis
- Complications of Babesiosis
- When to Seek Emergency Care
- How Babesiosis Is Diagnosed
- Treatment for Babesiosis
- Can Babesiosis Go Away on Its Own?
- Babesiosis Prevention
- Babesiosis vs. Lyme Disease vs. Anaplasmosis
- Babesiosis and Co-Infections
- Babesiosis in Children
- Babesiosis in Pregnancy
- Global Distribution & Climate Change Impact
- When to Consult a Doctor
- Conclusion
- FAQs
Babesiosis is an emerging tick-borne infection that attacks your red blood cells, causing symptoms that range from mild, flu-like illness to severe haemolytic anaemia. This parasitic disease, transmitted primarily through infected blacklegged tick bites, remains largely unknown to many people despite its increasing prevalence in certain regions.
Understanding the causes and early symptoms of babesiosis—and knowing when to seek medical attention—can significantly improve outcomes can make a significant difference in your health outcomes.
What Is Babesiosis?
Babesiosis is an infectious disease caused by protozoan parasites of the genus Babesia, which specifically target and destroy red blood cells. These microscopic organisms invade your erythrocytes, multiply inside them, and eventually cause the cells to burst, leading to haemolytic anaemia in severe cases.
The most common species affecting humans is Babesia microti, primarily found in certain regions where blacklegged ticks thrive. Once these parasites enter your bloodstream through a tick bite, they begin their destructive cycle within your red blood cells. This red blood cell infection can range from completely asymptomatic to life-threatening, depending on various factors including your immune system strength and overall health status.
Unlike many other infections, babesiosis can persist in your system for months or even years if left untreated, making early diagnosis of babesiosis crucial for effective management.
How Babesiosis Spreads
Understanding how this infection transmits helps you take appropriate preventive measures:
- Tick bites: The primary transmission occurs through bites from infected blacklegged (deer) ticks carrying Babesia parasites
- Blood transfusions: Contaminated blood products can transmit the infection because Babesia parasites can survive in stored blood
- Organ transplantation: Rarely, infected donor organs may transmit the infection to recipients
- Mother-to-child transmission: Pregnant women can pass the infection to their babies during pregnancy or delivery
- No casual contact spread: You cannot catch babesiosis through touching, coughing, or everyday contact with infected individuals
How Long It Takes to Get Babesiosis After a Tick Bite
After an infectious tick bite, babesiosis symptoms typically begin appearing 1-6 weeks later. The incubation period varies significantly between individuals, with some people developing symptoms within a week while others may not notice any signs for several months. This delayed onset often makes it challenging to connect the illness with the original tick exposure, especially if you don't remember being bitten.
Where Is Babesiosis Found?
Babesiosis occurs most commonly in temperate regions where blacklegged ticks establish populations. In the United States, human cases concentrate in the Northeast and upper Midwest states, particularly areas where Lyme disease is also endemic. The infection is considered emerging, with reported cases increasing due to expanding tick populations, climate changes, and improved diagnostic recognition.
Globally, different Babesia species cause disease in Europe and Asia, often associated with cattle or wildlife reservoirs. As environmental conditions change and tick ranges expand, babesiosis may appear in previously unaffected areas.
Babesiosis Symptoms
Many people with babesiosis never develop noticeable symptoms, but when they occur, they often resemble flu-like illness:
- Fever (often high and persistent)
- Chills and sweats (particularly night sweats)
- Fatigue and weakness (sometimes severe)
- Headache (can be intense)
- Body aches and muscle pain
- Loss of appetite
- Nausea and sometimes vomiting
- General malaise (feeling unwell)
- Dark urine or jaundice (indicating haemolytic anaemia)
- Shortness of breath (in severe cases)
Mild vs. Severe Symptoms of Babesiosis
|
Mild Babesiosis |
Severe Babesiosis |
|
Low-grade fever, manageable fatigue |
High persistent fever, profound weakness |
|
Mild anaemia, stable condition |
Significant haemolytic anaemia, jaundice |
|
Normal breathing patterns |
Shortness of breath, respiratory distress |
|
Stable blood pressure |
Low blood pressure, possible shock |
|
Normal organ function |
Potential organ failure |
|
Usually outpatient treatment |
Often requires hospitalisation |
Causes & Pathophysiology
Babesiosis is caused by protozoan parasites that invade and multiply within your red blood cells. After entering through tick bites, these organisms reproduce asexually inside erythrocytes, eventually causing cell destruction and haemolytic anaemia. This process releases cellular contents into your bloodstream, triggering inflammatory responses and potentially leading to organ dysfunction in severe cases.
The parasites' ability to hide within red blood cells makes them particularly challenging for your immune system to eliminate, explaining why some infections persist for extended periods.
Risk Factors for Severe Babesiosis
Certain groups face higher risks for developing severe babesiosis symptoms:
- Adults over 50 years of age are more likely to experience complications
- People without spleens (asplenic individuals) cannot effectively clear infected red blood cells and are especially susceptible to severe infection
- Immunocompromised patients including those with HIV, cancer, or taking immunosuppressive medications
- Individuals with chronic illnesses such as heart disease or diabetes
- Those taking certain medications that affect immune function
Complications of Babesiosis
Severe babesiosis can lead to serious complications requiring immediate medical attention:
- Severe haemolytic anaemia requiring transfusions
- Kidney failure from damaged red blood cells
- Liver dysfunction and jaundice
- Acute respiratory distress syndrome (ARDS)
- Heart failure or cardiac complications
- Blood clotting disorders
- Multi-organ failure in extreme cases
When to Seek Emergency Care
Contact emergency services immediately if you experience:
- Difficulty breathing or shortness of breath at rest
- Chest pain or rapid heartbeat
- Severe weakness or inability to stand
- Dark brown or cola-coloured urine
- Yellow skin or eyes (jaundice)
- High fever above 39°C (102°F) with severe symptoms
- Confusion or altered mental state
How Babesiosis Is Diagnosed
Healthcare providers use several methods for accurate babesiosis diagnosis:
- Blood smear examination: Microscopic examination reveals parasites inside red blood cells
- Molecular testing (PCR): Detects parasite DNA with high accuracy
- Antibody testing: Measures immune response to Babesia infection
- Complete blood count: Shows signs of haemolytic anaemia and low platelet counts
- Clinical assessment: Evaluates symptoms, tick exposure history, and risk factors
Your doctor will also inquire about any recent travel to tick-endemic areas, outdoor activities, and whether you've noticed any tick bites recently.
Treatment for Babesiosis
Babesiosis is treated when symptoms are present or when the parasite remains detectable on testing for an extended period. According to research summarised by the National Library of Medicine, most mild to moderate infections are managed with a combination of atovaquone and azithromycin, which is generally effective and better tolerated. Quinine with clindamycin may be used as an alternative but is more likely to cause side effects.
Treatment typically lasts 7–14 days, with adjustments depending on clinical response. People with weakened immunity or recurring infection may need longer therapy until blood tests confirm parasite clearance. In cases that do not improve, different drug combinations may be used, though no single option is clearly superior.
Treatment for Severe Babesiosis
Severe cases require more intensive babesiosis treatment approaches:
- Hospitalisation for close monitoring and supportive care
- Intravenous clindamycin plus quinine (or quinidine with cardiac monitoring)
- Exchange transfusion may be required for parasitaemia ≥10%, severe anaemia, or evidence of organ dysfunction
- Blood transfusions to correct significant haemolytic anaemia
- Organ support, such as dialysis for kidney failure
- Intensive care monitoring, as respiratory distress and multi-organ complications are common in severe disease
Can Babesiosis Go Away on Its Own?
While some people with strong immune systems might clear mild babesiosis infections without treatment, this approach carries significant risks. Untreated infections can persist for months or years, potentially leading to chronic symptoms and serious complications. The parasites may persist at low levels and reactivate during periods of immune suppression, making proper medical treatment essential for complete recovery.
Babesiosis Prevention
- Use insect repellents containing DEET, picaridin, or permethrin on skin and clothing
- Wear protective clothing including long sleeves, long trousers, and closed shoes when in tick habitats
- Perform thorough daily tick checks on yourself, your children, and pets after outdoor activities
- Shower within two hours of coming indoors to wash off unattached ticks
- Keep grass short and remove leaf litter around your home
- Create barriers using wood chips or gravel between wooded areas and your garden
How to Remove a Tick Safely
- Use fine-tipped tweezers to grasp the tick as close to your skin as possible
- Pull steadily upward with even pressure; don't twist or jerk the tick
- Clean the bite area thoroughly with soap and water or an antiseptic solution
- Dispose of the tick by flushing it down the toilet or placing it in alcohol
- Monitor the bite site for signs of infection or unusual symptoms over the following weeks
Babesiosis vs. Lyme Disease vs. Anaplasmosis
|
Feature |
Babesiosis |
Lyme Disease |
Anaplasmosis |
|
Primary symptoms |
Flu-like, haemolytic anaemia |
Bull's-eye rash, joint pain |
Fever, headache, muscle aches |
|
Diagnostic tests |
Blood smear, PCR |
Antibody tests, clinical signs |
Blood tests, PCR |
|
Treatment |
Atovaquone + azithromycin |
Doxycycline |
Doxycycline |
|
Complications |
Severe anaemia, organ failure |
Arthritis, neurological issues |
Low white blood cell count |
Babesiosis and Co-Infections
Approximately 20% of babesiosis patients also contract Lyme disease, as the same ticks can carry multiple pathogens simultaneously. Co-infections typically result in more severe symptoms and prolonged illness duration. If you're diagnosed with one tick-borne disease, your healthcare provider will likely test for others to ensure comprehensive treatment.
Babesiosis in Children
Children usually experience milder babesiosis symptoms than adults, often resembling common viral infections. However, very young children and those with compromised immune systems face higher risks for severe complications. Parents should watch for persistent fever, unusual fatigue, or breathing difficulties following potential tick exposure.
Babesiosis in Pregnancy
Pregnant women with babesiosis face risks of transmitting the infection to their unborn babies. The condition can also complicate pregnancy through severe anaemia or other complications. Prompt diagnosis and treatment during pregnancy are crucial to protect both maternal and foetal health.
Global Distribution & Climate Change Impact
Climate change is expanding tick habitats and extending their active seasons, potentially increasing babesiosis transmission in previously unaffected regions. Warmer temperatures and changing precipitation patterns create favourable conditions for tick populations to establish in new areas, making awareness and prevention even more important.
When to Consult a Doctor
Seek medical attention if you develop flu-like symptoms within six weeks of potential tick exposure, especially if you've been in areas where babesiosis is endemic. Early consultation allows for prompt babesiosis diagnosis and treatment, significantly improving your prognosis and reducing complication risks.
Conclusion
Babesiosis represents a serious but manageable tick-borne infection that requires awareness, prevention, and prompt medical attention. The key to managing this red blood cell infection lies in prevention through tick bite avoidance and seeking immediate medical care when symptoms develop.
At Metropolis Healthcare, we support your health journey with comprehensive diagnostic services designed for accuracy and convenience. Our extensive portfolio of over 4,000 tests includes specialised panels for infectious diseases like babesiosis, ensuring precise diagnosis when you need it most. Through our network of 10,000+ touchpoints across India, we bring reliable testing directly to your doorstep with our home sample collection service.
FAQs
What causes babesiosis in humans?
Babesiosis is caused by Babesia parasites transmitted primarily through infected blacklegged tick bites. These microscopic organisms invade red blood cells, multiply within them, and cause cell destruction leading to various symptoms ranging from mild flu-like illness to severe haemolytic anaemia.
How serious is babesiosis?
The severity of babesiosis varies significantly between individuals. Many people experience no symptoms at all, while others develop mild flu-like illness. However, vulnerable populations including older adults, people without spleens, and immunocompromised individuals can develop life-threatening complications.
What are the first signs of babesiosis?
Early babesiosis symptoms typically include fever, chills, sweats, fatigue, headache, and body aches—very similar to flu symptoms. These signs usually appear 1-6 weeks after an infected tick bite.
Can babesiosis be cured?
Yes, babesiosis can be effectively treated with appropriate antibiotic combinations, typically atovaquone plus azithromycin. Early treatment leads to better outcomes, while severe cases may require hospitalisation and additional supportive care.
How long does babesiosis last?
With proper treatment, most people recover from babesiosis within 1-2 weeks. However, untreated infections can persist for months or even years, with symptoms potentially lasting 6-8 weeks.
Can you get babesiosis twice?
Reinfection with babesiosis is possible but uncommon. Previous infection may provide some immunity, but this protection isn't complete or permanent. People can potentially contract different Babesia species or experience reactivation of persistent infections during periods of immune suppression.
Will doxycycline treat babesiosis?
Doxycycline is not the standard treatment for babesiosis. The preferred treatment combines atovaquone with azithromycin, or alternatively clindamycin with quinine for severe cases.
How do you prevent babesiosis from tick bites?
Prevention focuses on avoiding tick bites through protective clothing, insect repellents containing DEET or picaridin, daily tick checks after outdoor activities, prompt tick removal, and maintaining tick-free environments around your home by keeping grass short and removing leaf litter.
References
- https://www.ncbi.nlm.nih.gov/books/NBK430715/#article-18082.s8
- https://my.clevelandclinic.org/health/diseases/24809-babesiosis
- https://www.cdc.gov/dpdx/babesiosis/index.html
- https://www.publichealthontario.ca/en/Diseases-and-Conditions/Infectious-Diseases/Vector-Borne-Zoonotic-Diseases/Babesiosis




























