Preventive Healthcare
Double Uterus: Causes, Symptoms, Pregnancy, and Treatment Explained
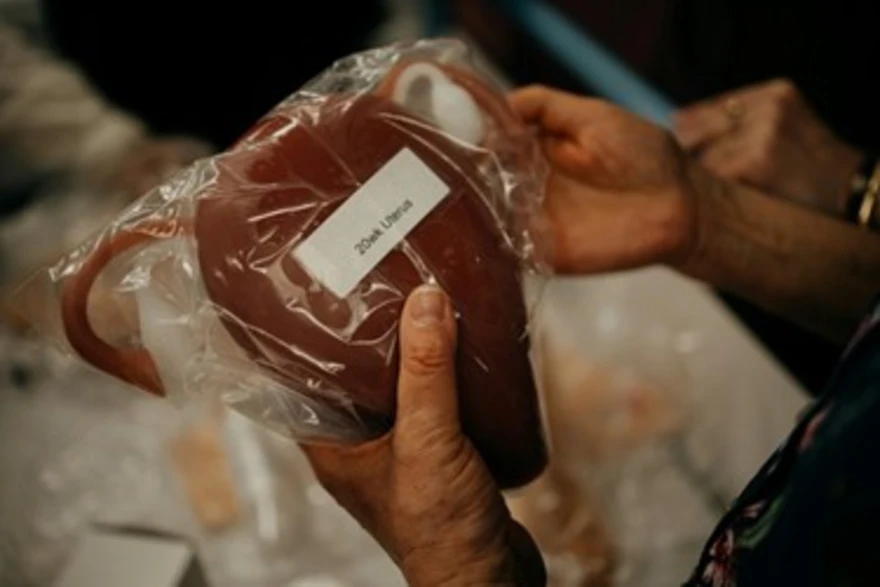
Table of Contents
- What is a Double Uterus (Uterus Didelphys)?
- Types of Uterine Malformations Related to Double Uterus
- How Does a Double Uterus Form? (Developmental Causes)
- Symptoms of Double Uterus (Uterus Didelphys)
- When to See a Doctor
- How is a Double Uterus Diagnosed?
- Double Uterus and Pregnancy: What You Should Know
- Treatment Options for Double Uterus
- Possible Complications if Untreated
- Living with a Double Uterus
- Prevention & Outlook
- Conclusion
- FAQs
- References
What is a Double Uterus (Uterus Didelphys)?
A double uterus, medically known as uterus didelphys, is a rare congenital anomaly of the female reproductive system where a woman is born with two separate uterine cavities, often each with its own cervix. This condition develops before birth when the two embryonic structures that normally fuse to form a single uterus remain completely separate.
If you or a loved one has been diagnosed with uterus didelphys, understanding the causes, symptoms, and implications for pregnancy and fertility is crucial. In this article, we provide a comprehensive overview of this condition, addressing common concerns and offering expert guidance on managing a double uterus.
Types of Uterine Malformations Related to Double Uterus
Developmental malformations of the uterus occur when the Müllerian ducts fail to form, fuse, or dissolve properly during fetal life.
The major types of uterine malformations include:
- Uterus Didelphys (Double Uterus): Complete duplication of the uterus and cervix, with two distinct cavities.
- Bicornuate Uterus: A single uterus that has two upper cavities forming a heart shape due to partial fusion failure.
- Septate Uterus: The uterus is divided internally by a fibrous or muscular septum, creating two compartments within one outer structure.
- Unicornuate Uterus: One side of the uterus develops normally while the other remains underdeveloped or absent.
- OHVIRA Syndrome (Obstructed Hemivagina and Ipsilateral Renal Anomaly): Also known as Herlyn–Werner–Wunderlich syndrome, is a rare combination of uterus didelphys with a hemivaginal obstruction and ipsilateral renal agenesis or dysplasia.
How Does a Double Uterus Form? (Developmental Causes)
A double uterus (uterus didelphys) forms when the two Müllerian ducts fail to fuse during fetal development. Instead of forming a single uterus, each duct develops into a separate one.
The exact cause of this congenital defect is unknown, but it may occur alongside urinary tract abnormalities, as both systems develop simultaneously in the embryo.
Symptoms of Double Uterus (Uterus Didelphys)
According to studies referenced by the National Institutes of Health (NIH), uterus didelphys is a rare Müllerian anomaly, accounting for approximately 5–8% of all congenital uterine malformations. Many women with uterus didelphys experience no symptoms and discover the condition incidentally during a pelvic exam or pregnancy ultrasound.
However, when symptoms occur, they may include:
- Heavy or prolonged menstrual bleeding due to the two uterine cavities shedding tissue.
- Irregular menstrual flow or spotting between periods
- Painful periods (dysmenorrhea) caused by obstructed outflow or tissue buildup
- Pelvic discomfort or pain during menstruation or intercourse
- Two cervices or, in some cases, a vaginal septum creating two vaginal openings may be identified during pelvic examination
- Recurrent miscarriages or preterm deliveries
- Difficulty conceiving (infertility in some cases)
When to See a Doctor
You should see a doctor or gynaecologist if you experience unusual menstrual patterns, severe cramps, or repeated miscarriages. Early medical consultation is also advised if you’ve been trying to conceive without success or if an imaging test suggests uterine abnormalities.
Even if uterus didelphys is discovered incidentally, consulting a specialist helps assess its impact on reproductive health. Regular follow-ups allow for proper management, especially for women planning pregnancy or already pregnant.
How is a Double Uterus Diagnosed?
Diagnosis of a double uterus typically involves a combination of pelvic examination, imaging, and minimally invasive tests.
The step-by-step diagnostic process includes:
- Pelvic Examination: The doctor may detect two cervices or vaginal canals.
- Ultrasound: Provides a basic visual of uterine shape and size, identifying dual structures.
- MRI (Magnetic Resonance Imaging): Offers detailed 3D visualisation of internal reproductive anatomy.
- Hysterosalpingography (HSG): An X-ray test that shows the shape of the uterus and fallopian tubes using contrast dye.
- Hysteroscopy: Endoscopic examination of the inside of the uterine cavity.
- Laparoscopy: Minimally invasive surgery to view pelvic organs directly.
- Renal ultrasound: To check for kidney abnormalities commonly associated with Müllerian duct anomalies.
Double Uterus and Pregnancy: What You Should Know
Women with uterus didelphys can conceive naturally because the ovaries function and the fallopian tubes usually work normally. However, pregnancy outcomes depend on which uterus the embryo implants in and the available space for fetal development.
Key facts about a double uterus and pregnancy:
- Pregnancy is possible and often successful, though there is a higher risk of miscarriage, preterm birth, and malpresentation.
- There’s a chance of fetal malpresentation (breech or transverse position).
- C-section deliveries are more common due to a narrow uterine space.
- In exceptionally rare cases, women have conceived simultaneously in both uteri, a condition termed ‘double pregnancy’ or ‘simultaneous bilateral pregnancy.
- Continuous prenatal monitoring is crucial for maternal and fetal safety.
Key complications to monitor for:
- Preterm birth
- Spontaneous abortion (miscarriage)
- Breech or abnormal fetal positioning
- Retained placenta or bleeding after delivery
Treatment Options for Double Uterus
Not all women with a uterus didelphys require treatment. Management depends on the presence of symptoms or complications.
Treatment strategies include:
- Observation: If asymptomatic, regular monitoring is sufficient.
- Surgical correction (Strassman or unification metroplasty): Is rarely indicated and typically reserved for specific cases where reproductive outcomes may improve.
- Vaginal Septum Removal: Helps relieve pain and improve sexual comfort or facilitate childbirth.
- Hormonal Management: For irregular menstrual cycles or pain relief.
- Reproductive Counselling: To plan safe pregnancies and reduce miscarriage risk.
Possible Complications if Untreated
- Recurrent pregnancy loss or preterm birth may occur due to reduced uterine volume and abnormal contractility.
- Dysmenorrhea (painful periods) from obstruction or dual menstruation.
- Labour complications, including breech presentation.
- In rare cases, complications arise due to abnormal implantation within one uterine cavity.
- Associated urinary tract issues, especially in OHVIRA syndrome cases.
Living with a Double Uterus
Many women with two uteruses live completely normal lives without health issues. With appropriate guidance, they can experience regular menstrual cycles, healthy pregnancies, and normal deliveries. Emotional support, reproductive counselling, and awareness play a significant role in managing anxiety or misconceptions about fertility.
Maintaining a healthy lifestyle, including a balanced diet, adequate hydration, and regular gynaecological checkups, can help monitor the condition effectively and support overall reproductive well-being.
Prevention & Outlook
Because uterus didelphys results from a developmental anomaly of the Müllerian ducts, it cannot be prevented, but early detection and multidisciplinary care improve outcomes. However, awareness, timely diagnosis, and personalised care significantly improve outcomes. Most women have normal hormonal cycles and can conceive successfully with medical guidance.
The long-term outlook for women with a double uterus is positive. With ongoing medical support, they can live healthy, fulfilling lives with minimal complications and excellent reproductive potential.
Conclusion
A double uterus (uterus didelphys) may sound alarming, but with today’s medical advances, it’s entirely manageable. Early detection through imaging tests, reproductive counselling, and careful pregnancy monitoring enables women to lead full, healthy lives.
Metropolis Healthcare supports this journey with comprehensive diagnostic testing, full-body checkups, home sample collection, and speciality reproductive tests — all backed by over 220 NABL & CAP certified laboratories producing accurate results, with over 10,000 touchpoints for nationwide convenience.
Your health begins with awareness — and the right diagnosis makes all the difference.
FAQs
What is the difference between a double uterus and a bicornuate uterus?
A double uterus involves two entirely separate uterine cavities, each with its own cervix (and sometimes two vaginas). In contrast, a bicornuate uterus is a single uterus with a deep indentation or septum, resulting in a heart-shaped uterine cavity but only one cervix.
Can a woman with a double uterus get pregnant naturally?
Yes, a natural pregnancy is possible. Many women with a double uterus conceive without intervention, but they are at higher risk for miscarriage, preterm labour, and require closer obstetric monitoring.
Is surgery necessary for a double uterus?
Surgery is rarely needed. It is only recommended if the condition causes significant symptoms (such as pain or obstructed menstrual flow) or if anatomical correction may improve pregnancy outcomes.
Does having a double uterus cause pain or heavy periods?
Some women experience painful periods (dysmenorrhea) or heavy menstrual bleeding (menorrhagia), especially if there is a vaginal septum or menstrual blood flow is obstructed, but many are asymptomatic.
Can a double uterus cause miscarriage or infertility?
Yes, it can increase the risk of miscarriage, infertility, and preterm birth compared to women with a single uterus.
How is a double uterus diagnosed?
- Medical history and pelvic exam
- Pelvic ultrasound
- MRI
- Hysterosalpingography (HSG)
- Hysteroscopy or laparoscopy if needed
- Renal ultrasound to check for kidney anomalies
What is the long-term outlook for women with a double uterus?
With appropriate care, most women with a double uterus can live healthy lives and have successful pregnancies. However, they require increased monitoring during pregnancy and may need specialised obstetric support for optimal outcomes.
References
https://pmc.ncbi.nlm.nih.gov/articles/PMC7231278/
https://my.clevelandclinic.org/health/diseases/23301-uterus-didelphys
https://www.mayoclinic.org/diseases-conditions/double-uterus/symptoms-causes/syc-20352261
https://www.webmd.com/women/uterine-didelphys-double-uterus




























