Preventive Healthcare
Pineal Tumours: Complete Guide To Diagnosis, Risks & Treatment Options
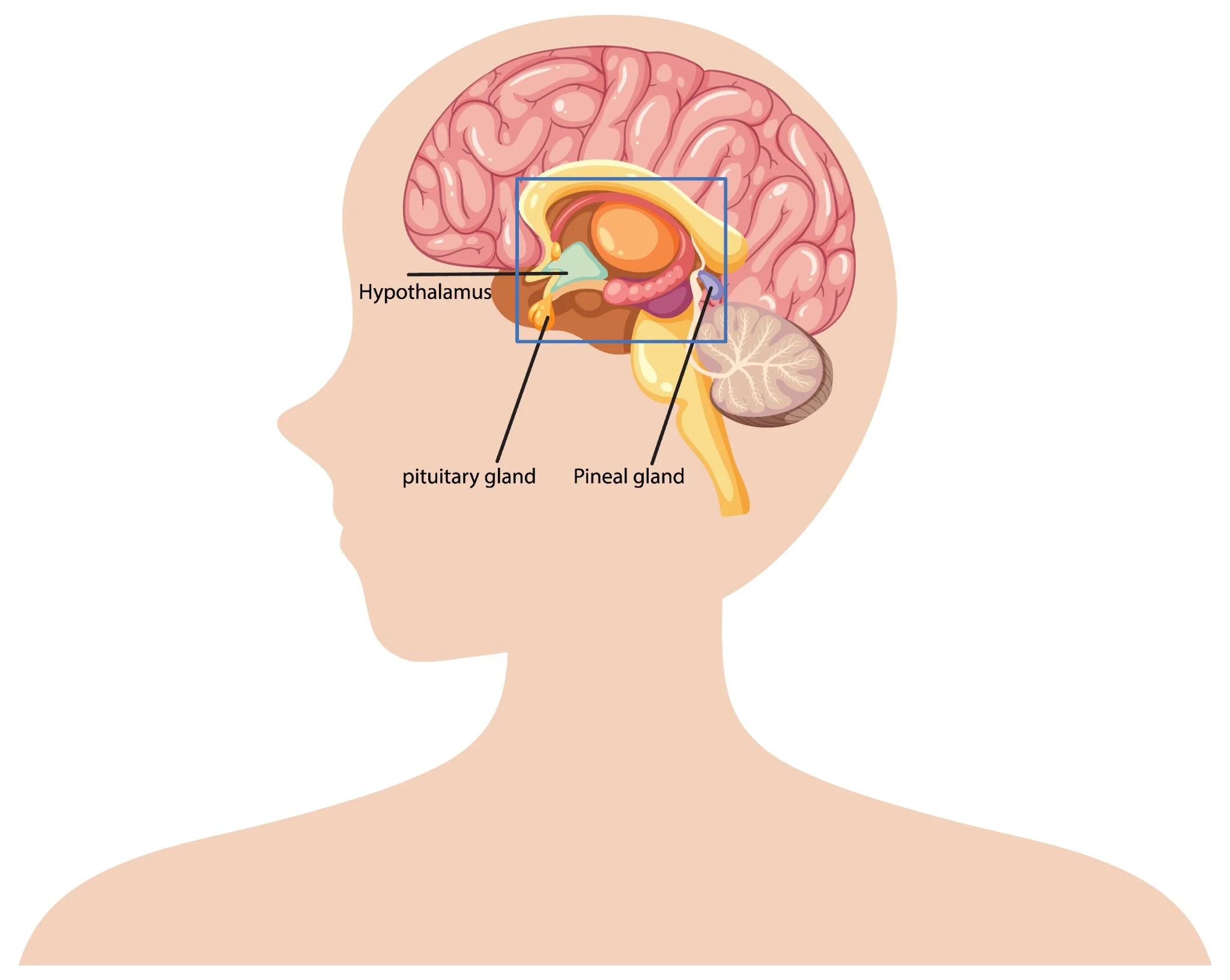
Table of Contents
- What Are Pineal Tumours?
- Understanding the Pineal Gland
- Types of Pineal Tumours
- How Common Are Pineal Tumours?
- Causes & Risk Factors of Pineal Tumours
- Pineal Tumour Symptoms
- Complications Associated With Pineal Tumours
- How Pineal Tumours Are Diagnosed
- Tests for Pineal Tumours
- Treatment Options for Pineal Tumours
- Prognosis & Survival Rate
- Recovery & Rehabilitation
- Living With a Pineal Tumour
- When to Seek Medical Help
- Conclusion
- FAQs
- References
What Are Pineal Tumours?
Pineal region tumours are a diverse group of neoplasms that arise from the pineal gland or adjacent structures such as germ cells, glial tissue, or supporting stroma, a small area located deep between the brain's hemispheres. These rare brain tumours can originate directly from pineal gland tissue or develop from surrounding structures. The pineal gland itself is only about 8 millimetres long, roughly the size of a rice grain, yet pineal tumours can cause significant health complications due to their strategic location.
Pineal region masses are broadly classified as primary tumours (originating in the pineal gland or nearby structures) and secondary lesions (metastases or local extensions from nearby brain regions). Primary pineal region tumours account for less than 1% of all intracranial neoplasms and approximately 3–11% of paediatric brain tumours. However, their location near critical brain structures makes early detection and proper treatment essential.
The complexity of pineal tumours lies in their proximity to vital brain areas that control cerebrospinal fluid flow, eye movements, and various neurological functions. When pineal tumours grow, they can block normal fluid pathways, leading to increased pressure within your skull and potentially life-threatening complications.
Understanding the Pineal Gland
The pineal gland serves as your body's internal clock, producing melatonin to regulate sleep-wake cycles and circadian rhythms.
This small endocrine gland also influences:
• Sleep patterns: Melatonin production increases in darkness, promoting restful sleep.
• Reproductive functions: Hormonal regulation affects sexual development and fertility.
• Seasonal behaviour: Light exposure influences mood and energy levels.
• Metabolic processes: Coordination with other hormone systems.
Located deep within your brain's centre, the pineal gland sits near the third ventricle, a fluid-filled cavity. This strategic position means pineal tumours can easily disrupt cerebrospinal fluid flow, causing hydrocephalus (fluid buildup in the brain). The gland's proximity to visual pathways also explains why pineal tumours often cause distinctive eye movement problems.
Types of Pineal Tumours
Pineal tumour types vary significantly in their behaviour, growth patterns, and treatment responses. The main categories include:
Pineal Parenchymal Tumours (WHO 2021 subtypes):
• Pineocytoma (WHO Grade 1): Slow-growing, low-grade tumours with a better prognosis
• Pineoblastoma (WHO Grade 4): Aggressive, high-grade tumours requiring intensive treatment
• Pineal parenchymal tumour of intermediate differentiation – PPTID (WHO Grade 2–3): Moderate-grade tumours with variable behaviour
• Papillary tumour of the pineal region (WHO Grade 2–3): Rare tumours with distinct cellular features
• Desmoplastic myxoid tumour, SMARCB1-mutant (WHO Grade 2): Desmoplastic myxoid tumour, SMARCB1-mutant: A newly recognised entity in the WHO 5th edition with loss of SMARCB1/INI1 expression
Intracranial Germ Cell Tumours:
• Germinoma (most common; radiosensitive): The most common type, often responds well to radiation
• Non-germinomatous GCTs (NGGCTs): teratoma, embryonal carcinoma, yolk sac tumour, choriocarcinoma
• Mixed GCTs (combinations of the above): Combinations of different germ cell elements
How Common Are Pineal Tumours?
Pineal tumours represent less than 1% of all brain tumours, making them exceptionally rare. In India, brain tumours overall affect approximately 5-10 people per 100,000 annually, with pineal tumours comprising only a tiny fraction of these cases. These statistics highlight why many healthcare providers have limited experience treating pineal tumours.
As per a 2021 review in the National Institutes of Health (NIH), pineal gland tumours are rare, accounting for about 3–11% of paediatric brain tumours but less than 1% of adult brain tumours. A large series of them showed germinomas (27%) and astrocytomas (26%) as the most common types, followed by pineoblastomas (12%) and pineocytomas (12%).
Age distribution varies significantly among different pineal tumour types. Pinealoblastomas typically affect children and young adults, with peak incidence occurring before age 20. Conversely, pineocytomas more commonly develop in adults aged 20-60 years. Germ cell tumours show a strong male predominance, affecting boys and men approximately four times more frequently than females.
Causes & Risk Factors of Pineal Tumours
Pineal tumour causes remain largely unknown, with most cases occurring sporadically without identifiable triggers. However, several factors may influence development:
• Molecular alterations vary by subtype: SMARCB1 mutations in desmoplastic myxoid tumours, RB1 or DICER1 alterations in pineoblastoma, and KIT/KITLG pathway mutations in germinomas.
• Age-related factors: Different tumour types show distinct age preferences.
• Gender influences: Male predominance in germ cell tumours suggests hormonal factors.
• Environmental exposures: No definitive environmental causes have been established.
• Radiation exposure: Previous brain radiation may rarely increase risk.
• Genetic syndromes: Certain inherited conditions may predispose to brain tumours.
Pineal Tumour Symptoms
Pineal tumours' symptoms typically result from increased brain pressure and compression of surrounding structures. Recognising these warning signs enables earlier diagnosis and treatment:
- Severe headaches: Often worse in the morning or when lying down, caused by increased intracranial pressure.
- Vision problems: One of the common brain tumour symptoms is difficulty looking upward (Parinaud syndrome), double vision, or blurred sight.
- Nausea and vomiting: Particularly common in the morning, related to increased brain pressure.
- Balance difficulties: Unsteady walking, coordination problems, or frequent falls.
- Sleep disturbances: Changes in sleep patterns due to disrupted melatonin production.
- Hearing changes: Decreased hearing or ringing in the ears.
- Cognitive problems: Memory difficulties, confusion, or personality changes.
- Hormonal disruptions: Precocious puberty in children or reproductive issues in adults.
Complications Associated With Pineal Tumours
Pineal tumours can lead to serious complications requiring prompt medical attention:
• Hydrocephalus: Fluid buildup causing dangerous brain pressure increases
• Parinaud syndrome: Characteristic eye movement problems affecting upward gaze
• Increased intracranial pressure: A life-threatening condition requiring emergency treatment
• Hormonal imbalance: Disrupted sleep cycles and reproductive function
• Neurological deficits: Permanent damage to brain areas controlling movement, sensation, or cognition
• Seizures: Abnormal electrical activity in the brain
• Coma: Severe cases may result in loss of consciousness.
• Spinal cord spread: Malignant tumours may metastasise along cerebrospinal fluid pathways.
How Pineal Tumours Are Diagnosed
Diagnosing pineal tumours requires a systematic approach combining clinical evaluation with advanced imaging and laboratory tests:
- Neurological examination: A comprehensive assessment of brain and nerve function, including eye movements, reflexes, coordination, and cognitive abilities.
- Magnetic resonance imaging (MRI): Detailed brain scans using powerful magnets to visualise tumour size, location, and characteristics.
- Computed tomography (CT) scans: X-ray-based imaging to detect calcium deposits and provide structural information.
- Blood marker tests: Serum and CSF tumour markers such as AFP, β-hCG, and placental alkaline phosphatase (PLAP) are essential for identifying and differentiating germ cell tumours.
- Cerebrospinal fluid analysis: Examining spinal fluid for cancer cells and tumour markers.
- Contrast-enhanced imaging: Special dyes improve tumour visibility on scans.
- Spinal MRI: Checking for tumour spread to the spine and spinal cord.
- Tissue biopsy: Obtaining tumour samples for definitive diagnosis and treatment planning.
Tests for Pineal Tumours
Comprehensive testing for pineal tumours involves multiple diagnostic approaches:
- Blood and CSF tumour markers: AFP and β-hCG in blood, plus AFP and β-hCG in CSF, help classify pineal germ cell tumours.
- CSF examination: CSF cytology with tumour markers (AFP, β-hCG) and dedicated brain tumour/neuroendocrine marker profiles support diagnosis and staging.
- Histopathology and IHC: Histopathology with immunohistochemistry (IHC), including synaptophysin, chromogranin, cytokeratin, SALL4, and PLAP, helps classify pineal parenchymal or germ cell tumours.
- Genetic and molecular profiling: Molecular profiling via next-generation sequencing (NGS) aids in identifying actionable alterations (e.g., SMARCB1, RB1, DICER1, KIT), which may guide precision therapy characterise mutations and guide targeted therapy.
- Hormone and endocrine testing: ACTH, ADH (vasopressin), and growth hormone, along with pituitary hormone profiles and TSH (ultrasensitive or neonatal), detect pituitary–hypothalamic imbalance.
- Visual field testing: Automated perimetry and other visual field tests detect vision loss from optic nerve or chiasmal compression.
- Neuropsychological assessment: Brief cognitive screening and detailed memory/attention tests assess the impact on thinking, behaviour, and mood.
Treatment Options for Pineal Tumours
Pineal tumour treatment depends on the tumour type, size, location, and your overall health status. Treatment approaches include:
• Surgical removal: Complete or partial tumour resection when technically feasible.
• Radiation therapy: Proton beam or conformal radiotherapy is preferred to minimise radiation damage to nearby midbrain and visual pathways.
• Chemotherapy: Medications that destroy cancer cells, particularly effective for certain germ cell tumours.
• Stereotactic radiosurgery: Stereotactic radiosurgery (e.g., Gamma Knife or CyberKnife) can be used for small residual or recurrent lesions, especially germinomas or low-grade parenchymal tumours.
• Combination therapy: Multiple treatment modalities used together for optimal outcomes.
• Supportive care: Managing symptoms and complications throughout treatment.
Surgery for Pineal Tumours: What to Expect
Surgical approaches for pineal tumours require exceptional skill due to the challenging location:
• Preoperative planning: Detailed imaging and surgical simulation to optimise approach.
• Minimally invasive techniques: Endoscopic approaches through small openings when possible.
• Microsurgical resection: Using operating microscopes for precise tumour removal.
• Intraoperative monitoring: Real-time assessment of brain function during surgery.
• Immediate postoperative care: Intensive monitoring for complications.
• Recovery planning: Rehabilitation services to optimise functional outcomes.
Prognosis & Survival Rate
Prognosis for pineal tumours varies dramatically based on tumour type and individual factors. Pineocytomas, being slow-growing and benign, often have excellent long-term outcomes with appropriate treatment. Five-year survival rates exceed 95% for these low-grade tumours when completely removed.
Conversely, Pineoblastomas (WHO Grade 4) have 5-year survival rates around 60–70%, with poorer outcomes in infants and those with metastatic CSF spread depending on factors like age at diagnosis, tumour extent, and treatment response. Germ cell tumours show intermediate outcomes, with Germinomas are highly radiosensitive, achieving >90% long-term survival with combined radiation and chemotherapy.
Recent advances in treatment have improved outcomes for many patients. Combination therapies, refined surgical techniques, and better supportive care contribute to enhanced survival and quality of life. However, long-term follow-up remains essential, as some pineal tumours may recur years after initial treatment.
Recovery & Rehabilitation
Recovery from pineal tumour treatment involves comprehensive rehabilitation addressing various aspects of function:
• Physical therapy: Rebuilding strength, balance, and coordination affected by the tumour treatment.
• Occupational therapy: Relearning daily living skills and adapting to any permanent changes.
• Speech therapy: Addressing communication difficulties or swallowing problems.
• Cognitive rehabilitation: Improving memory, attention, and executive function.
• Psychological support: Counselling to address emotional impacts of diagnosis and treatment.
• Educational support: Helping children return to school with appropriate accommodations.
• Hormone replacement: Managing ongoing endocrine dysfunction.
• Regular monitoring: Ongoing scans and tests to detect any tumour recurrence.
Living With a Pineal Tumour
Living with a pineal tumour diagnosis means balancing treatment needs with long-term health management. It’s natural to feel anxious due to the rarity and complexity of these tumours. A strong support system, family, friends, healthcare providers, and peer groups can make a significant difference by offering both emotional reassurance and practical guidance throughout your journey.
Daily life may involve managing symptoms, coping with treatment side effects, and attending regular follow-ups. Some patients continue to experience sleep disturbances requiring melatonin support, while others may need hormone therapy or help with cognitive changes. Staying in close communication with your medical team, tracking symptoms, and preparing questions for appointments can make care more effective. With consistent medical support and self-awareness, many individuals with pineal tumours continue to lead active, meaningful lives.
When to Seek Medical Help
Seek immediate medical attention if you experience:
• Persistent or worsening headaches: Constant or intensifying head pain may indicate increased pressure inside the skull and needs urgent evaluation.
• Sudden vision problems: Blurred, double, or rapidly changing vision can signal compression of eye-movement pathways by a pineal tumour.
• Seizures: Any new or unexplained seizure requires immediate medical assessment to prevent further neurological complications.
• Loss of balance or coordination: Difficulty walking or frequent stumbling may point to pressure on the cerebellum or midbrain.
• Rapid changes in memory or behaviour: Sudden confusion, forgetfulness, or personality shifts may reflect tumour-related effects on brain function.
• Symptoms of hydrocephalus: Severe headache, repeated vomiting, or mental confusion suggest dangerous fluid buildup in the brain and require emergency care.
Conclusion
Pineal tumours are rare and complex, but early diagnosis and the right treatment plan significantly improve outcomes. If you or a loved one is experiencing symptoms or has been advised to undergo evaluation, choosing a trusted diagnostic partner becomes essential.
Metropolis Healthcare offers 4,000+ advanced tests, speciality tumour and hormonal panels, and full body checkups designed to support comprehensive brain and endocrine assessment. With highly trained phlebotomists, a strong home collection network across 10,000+ touchpoints, and quick, accurate results, you get quality healthcare without delays. From precise diagnostics to dependable reporting, Metropolis ensures that every patient receives the clarity and confidence needed to make informed health decisions.
FAQs
Are pineal tumours cancerous?
Some pineal tumours are benign (like pineocytomas), while others, such as pineoblastomas or certain germ cell tumours, are malignant. Treatment and prognosis depend on the exact tumour type.
What are the early warning signs of pineal gland tumours?
Early signs include:
• Headache
• Blurred or double vision
• Difficulty moving eyes upward
• Nausea or vomiting
• Sleep disturbances
How fast do pineal tumours grow?
The growth rate of pineal tumours varies widely. Pineocytomas are slow-growing (WHO Grade 1), whereas pineoblastomas and non-germinomatous germ cell tumours are high-grade and often require multimodal therapy.
Can a pineal tumour be removed surgically?
Yes. Many pineal tumours can be surgically removed, although complete removal may not always be possible due to the tumour’s deep location. Surgeons may perform partial resections along with radiation therapy.
Is a pineal tumour life-threatening?
Untreated pineal tumours can become life-threatening by causing hydrocephalus, brainstem compression, or malignant spread. With treatment, many cases are manageable.
What is the survival rate for pineal tumours?
Survival varies for pineal tumours by type:
• Germinomas: 85–95%
• Pineocytomas: high long-term survival
• Pineoblastomas: lower survival due to aggressiveness
Can pineal tumours affect sleep and hormones?
Yes. Since the pineal gland regulates melatonin, tumours may disrupt sleep, circadian rhythm, and hormonal balance.
Do pineal tumours always require surgery?
No. Many germ cell tumours respond well to radiation and chemotherapy and may not require surgical removal.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8036741/
- https://emedicine.medscape.com/article/249945-overview
- https://www.cancerresearchuk.org/about-cancer/brain-tumours/types/pineal-region-tumours
- https://my.clevelandclinic.org/health/body/23334-pineal-gland




























