Preventive Healthcare
What Is End-Stage Renal Disease? Symptoms, Causes, And Treatment Options
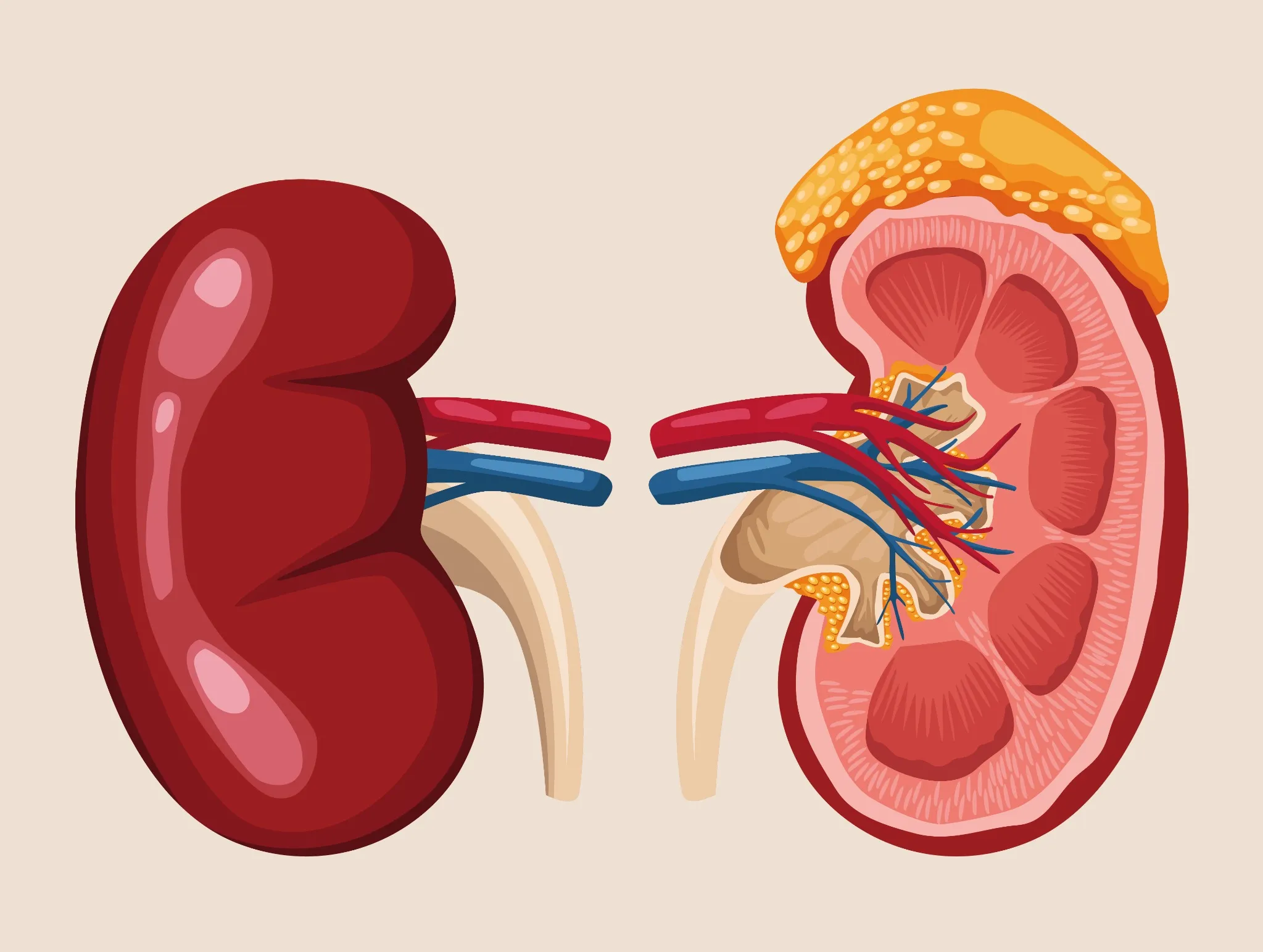
Table of Contents
- What Is End-Stage Renal Disease (ESRD)?
- Stages of Kidney Disease Leading to ESRD
- Causes of End-Stage Renal Disease
- Symptoms of End-Stage Renal Disease
- Complications of ESRD
- When to See a Doctor
- How End-Stage Renal Disease Is Diagnosed
- Tests for ESRD
- Treatment Options for End-Stage Renal Disease
- Medications Used in ESRD
- Diet & Lifestyle Guidelines for ESRD
- Life Expectancy & Prognosis
- Preventing ESRD in High-Risk Individuals
- Home Care Tips for ESRD Patients
- When to Consider Palliative or Supportive Care (Conservative Management)
- Conclusion
- FAQs
- References
What Is End-Stage Renal Disease (ESRD)?
End-stage renal disease (ESRD) is the final and most severe stage of chronic kidney disease (CKD). It occurs when the kidneys lose about 85–90% of their function, and the glomerular filtration rate (GFR) falls below 15 mL/min/1.73 m². At this point, the kidneys cannot clear waste, toxins, and extra fluid properly, leading to a dangerous build-up of waste products in the body, called uremia.
As per the National Institutes of Health (NIH), CKD is a progressive condition affecting more than 10% of the world’s population, that is, over 800 million people and is more common in older adults, women, racial minorities, and people with diabetes or high blood pressure.
ESRD corresponds to stage 5 CKD, where the kidneys can no longer support the body’s normal needs. Waste removal, fluid and electrolyte balance, and hormone production (which help regulate blood pressure and red blood cell formation) are all severely impaired. Without treatment such as dialysis or a kidney transplant, ESRD can be fatal. It usually develops after many years of kidney damage, but in some cases, it can progress faster after severe kidney injury.
Stages of Kidney Disease Leading to ESRD
Chronic kidney disease progresses through five distinct stages before reaching ESRD:
- Stage 1: Kidney damage with normal or increased GFR (≥90 mL/min).
- Stage 2: Mild loss of kidney function (GFR 60–89 mL/min).
- Stage 3: Moderate decline (GFR 30–59 mL/min).
- Stage 4: Severe decline (GFR 15–29 mL/min).
- Stage 5 (ESRD): Kidney failure with GFR <15 mL/min.
Causes of End-Stage Renal Disease
ESRD causes vary, but the most common underlying conditions include:
• Diabetes mellitus: The leading cause of ESRD, accounting for approximately 40% of cases.
• Hypertension: Responsible for roughly one-third of ESRD cases
• Glomerulonephritis: Inflammation of the kidney filtering units
• Polycystic kidney disease: Inherited disorder causing fluid-filled cysts
• IgA nephropathy: Immune-mediated kidney disease
• Lupus nephritis: Kidney inflammation from systemic lupus
• Alport syndrome: Genetic disorder affecting kidney structure
• Focal segmental glomerulosclerosis: Scarring of filtering units
How ESRD Develops (Pathophysiology)
ESRD typically develops as chronic kidney disease progresses over many years. Your kidneys initially compensate for declining function through hyperfiltration, in which the remaining nephrons work harder to filter waste. However, this compensatory mechanism eventually becomes overwhelmed as the original disease process continues to damage kidney tissue.
The increased workload on remaining nephrons accelerates their deterioration, creating a cascade of systemic complications. Waste products accumulate, electrolyte imbalances develop, and your kidneys' hormonal functions deteriorate, affecting multiple organ systems throughout your body.
Symptoms of End-Stage Renal Disease
ESRD symptoms develop gradually as kidney function declines and may include:
- Severe fatigue
- Nausea and vomiting
- Muscle cramps
- Swelling in the feet, legs, and around the eyes
- Shortness of breath
- Loss of appetite
- Itching
- Changes in urination
- Trouble concentrating
- High blood pressure
Early vs. Late Symptoms of ESRD
|
Symptom Stage |
Early ESRD Symptoms |
Advanced ESRD Symptoms |
|
Energy Level |
Mild fatigue, reduced stamina |
Severe exhaustion, inability to perform daily activities |
|
Gastrointestinal |
Occasional nausea, reduced appetite |
Persistent vomiting, complete appetite loss |
|
Fluid Balance |
Mild ankle swelling |
Severe oedema, difficulty breathing |
|
Mental Function |
Mild concentration issues |
Confusion, memory problems, seizures |
|
Urination |
Reduced urine output |
Little to no urine production |
Complications of ESRD
ESRD creates numerous serious complications affecting multiple body systems:
• Cardiovascular disease: Leading cause of death in ESRD patients
• Severe anemia: Causing extreme fatigue and cognitive impairment
• Bone disease: Weakened bones due to mineral imbalances
• Electrolyte disturbances: Dangerous potassium, sodium, and phosphorus levels
• Metabolic acidosis: Blood becomes too acidic
• Secondary hyperparathyroidism: Overactive parathyroid glands
• Protein-energy malnutrition: Muscle wasting and weight loss
• Immune system suppression: Increased infection risk
When to See a Doctor
Seek immediate medical attention if you experience:
• Persistent swelling that doesn't improve with elevation.
• Severe shortness of breath or chest pain.
• Confusion, seizures, or altered mental state.
• Blood in the urine or significantly decreased urination.
• Uncontrolled nausea and vomiting preventing fluid intake.
• Signs of severe electrolyte imbalance, like irregular heartbeat.
How End-Stage Renal Disease Is Diagnosed
Healthcare providers diagnose ESRD through a systematic approach:
- Comprehensive medical history: Including family history of kidney disease.
- Physical examination: Checking for swelling, blood pressure, and other symptoms.
- Laboratory testing: To assess kidney function and identify complications.
- Imaging studies: Such as ultrasound, are used to evaluate kidney structure.
- Kidney biopsy: In some cases, it is used to determine the underlying cause.
Tests for ESRD
Essential diagnostic tests for ESRD include:
- Serum creatinine (Creatinine, Serum; GFR with Creatinine, Serum): Measures waste product levels in blood
- Blood urea nitrogen (BUN) (BUN, Urine / 24 hrs or serum BUN): Indicates kidney filtration efficiency
- Complete blood count (CBC Haemogram, EDTA Blood): Detects anaemia and other blood disorders
- Electrolyte panel (Electrolytes, Serum / Electrolytes, Urine): Monitors sodium, potassium, and phosphorus levels
- Parathyroid hormone levels (PTH – Intact Molecule, Serum): Assesses bone metabolism
- Urinalysis (Albumin / Creatinine Ratio, Urine; Creatinine, Urine): Examines protein, blood, and other substances in urine
- 24-hour urine collection (Albumin – Quantitative, Urine 24 Hrs; Creatinine – Quantitative, Urine 24 Hrs): Measures protein loss and creatinine clearance
eGFR Levels Explained
|
eGFR Range |
Kidney Function |
CKD Stage |
|
>90 mL/min/1.73 m² |
Normal or high |
Stage 1 |
|
60-89 mL/min/1.73 m² |
Mildly decreased |
Stage 2 |
|
45-59 mL/min/1.73 m² |
Mildly to moderately decreased |
Stage 3a |
|
30-44 mL/min/1.73 m² |
Moderately to severely decreased |
Stage 3b |
|
15-29 mL/min/1.73 m² |
Severely decreased |
Stage 4 |
|
<15 mL/min/1.73 m² |
Kidney failure (ESRD) |
Stage 5 |
Treatment Options for End-Stage Renal Disease
ESRD treatment focuses on replacing kidney function through renal replacement therapy. The primary treatment options include dialysis and kidney transplantation. Your healthcare team will help determine the most appropriate ESRD treatment based on your overall health, lifestyle, and preferences.
Types of Dialysis for ESRD
Dialysis treatment artificially removes waste products and excess fluid from your blood:
• Haemodialysis: Blood is cleaned through an external machine, typically performed three times weekly at a dialysis centre.
• Peritoneal dialysis: Uses your abdominal lining as a natural filter and can be performed at home.
• Home haemodialysis: Allows more flexible scheduling and improved quality of life.
Kidney Transplant for ESRD
Kidney transplantation offers the best long-term outcome for suitable ESRD patients. A successful transplant can restore near-normal kidney function and significantly improve quality of life. However, transplant recipients require lifelong immunosuppressive medications to prevent rejection. Living donor transplants generally provide better outcomes than deceased donor kidneys.
Medications Used in ESRD
ESRD management involves various medications to control complications:
• Phosphate binders: Control high phosphorus levels
• Iron supplements: Treat anaemia associated with renal failure
• Erythropoiesis-stimulating agents: Stimulate red blood cell production
• Vitamin D analogues: Manage bone disease
• Blood pressure medications: Control hypertension
• Diuretics: Help remove excess fluid
Diet & Lifestyle Guidelines for ESRD
Proper nutrition management is crucial for ESRD patients:
• Protein restriction: Limit to 0.6–0.8 g/kg of body weight per day.
• Phosphorus limitation: Limit dairy products, nuts, and processed foods
• Potassium restriction: Limit bananas, oranges, and tomatoes.
• Sodium reduction: Keep intake below 2-3 g daily.
• Fluid management: May need restriction based on urine output.
• Regular exercise: Engage in light to moderate activity as tolerated to maintain strength and cardiovascular health.
Life Expectancy & Prognosis
ESRD prognosis varies significantly based on age, underlying conditions, and treatment choice. With dialysis treatment, five-year survival rates range from 35 to 85% depending on individual factors. Kidney transplant recipients typically enjoy better long-term survival, with 85-95% surviving five years post-transplant. Early transplantation before starting dialysis offers the best outcomes.
Preventing ESRD in High-Risk Individuals
Prevention strategies focus on managing underlying conditions:
• Diabetes control: Maintain HbA1c below 7%.
• Blood pressure management: Target <130/80 mmHg.
• Regular kidney function monitoring: Annual screening for high-risk individuals.
• Avoid nephrotoxic medications: Limit NSAIDs and certain antibiotics.
• Healthy lifestyle habits: Regular exercise, smoking cessation, and weight management
Home Care Tips for ESRD Patients
Supporting ESRD patients at home involves:
• Medication adherence: Use pill organisers and set reminders
• Dietary compliance: Meal planning with renal dietitian guidance
• Infection prevention: Proper hygiene, especially around dialysis access sites
• Regular monitoring: Daily weight checks and blood pressure measurements
• Emergency preparedness: Know when to seek immediate medical attention.
When to Consider Palliative or Supportive Care (Conservative Management)
Some ESRD patients may choose conservative management focusing on comfort and quality of life rather than life-extending treatments. This approach involves symptom management, nutritional support, and psychosocial care without dialysis or transplantation. Palliative care can be appropriate for elderly patients with multiple comorbidities or those who prefer comfort-focused treatment.
Conclusion
End-Stage Renal Disease (ESRD) is a serious, life-changing stage of renal failure that needs timely diagnosis, structured treatment, and regular follow-up. While it cannot be reversed, early detection of kidney damage, close monitoring, and the right treatment approach, dialysis or transplant, can help improve survival and quality of life.
In this journey, reliable diagnostics matter. Metropolis Healthcare offers 4000+ advanced tests, full body checkups, and speciality kidney testing with quick, accurate reports. Patients can choose home sample collection across 10,000+ touchpoints and enjoy easy booking via website or app, making it simpler to manage ESRD care with comfort, convenience, and trusted expertise.
FAQs
What are the first signs of ESRD?
The first signs of ESRD may include:
- Fatigue
- Swelling
- Changes in urination
- Persistent nausea
How long can you live with end-stage renal disease?
With dialysis and proper care, many patients live for years to decades. A successful kidney transplant often provides better long-term outcomes.
Is ESRD curable?
ESRD cannot be cured, but dialysis and kidney transplants allow patients to live full and productive lives.
What is the best treatment for ESRD?
A kidney transplant is considered the best long-term option, but dialysis is essential for those awaiting a transplant or not eligible for surgery.
Can ESRD patients ever stop dialysis?
Dialysis can be stopped only after a successful kidney transplant or if the patient chooses supportive care due to medical reasons.
What foods should be avoided in ESRD?
An individual with ESRD must avoid the following foods:
- High-potassium foods
- High-sodium foods
- High-phosphorus foods
- Processed and packaged snacks
Can ESRD be prevented?
Yes. Managing diabetes, controlling blood pressure, and regular screening help prevent progression to ESRD.
What eGFR level indicates ESRD?
An eGFR less than 15 mL/min confirms end-stage renal disease.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9073222/
- https://www.mayoclinic.org/diseases-conditions/end-stage-renal-disease/symptoms-causes/syc-20354532
- https://medlineplus.gov/ency/article/000500.htm
- https://emedicine.medscape.com/article/2500089-overview




























