Preventive Healthcare
Bicuspid Aortic Valve: What It Means & When to Treat It
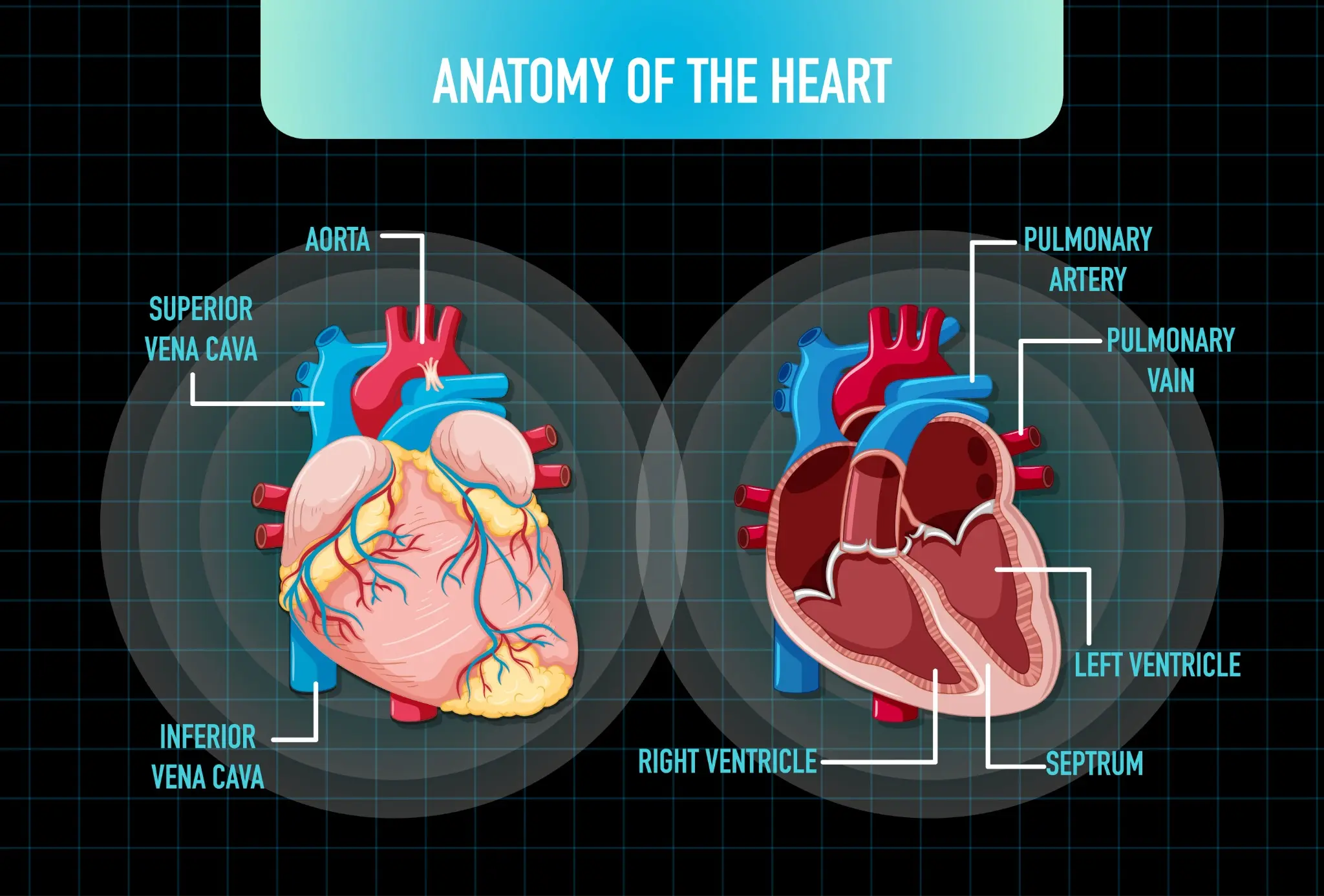
Table of Contents
What Is a Bicuspid Aortic Valve?
A bicuspid aortic valve (BAV) is a congenital heart defect in which the aortic valve, which normally has three leaflets (cusps), forms with only two functional leaflets. This abnormal valve structure can affect how efficiently blood flows from the heart into the aorta, increasing the risk of valve complications over time.
BAV is the most common congenital cardiac malformation, occurring in approximately 1–2% of the population and affecting males about three times more often than females.
Anatomy and Function of the Aortic Valve
The aortic valve is located between the heart's left ventricle and the aorta—the body's largest artery. Its main function is to act as a one-way gate, allowing oxygen-rich blood to flow out of the heart and preventing it from flowing backward during the heart's relaxation phase. The valve's flaps (cusps) open widely with each heartbeat to enable blood flow and close tightly to seal off the aorta from the heart.
Diagram Caption:
A normal aortic valve has three leaflets (tricuspid), while a bicuspid aortic valve has only two leaflets, which may cause abnormal flow patterns and increased wear on the valve over time.
Types of Bicuspid Aortic Valve
- Classic bicuspid: This is the most common form of the two bicuspid aortic valve types, characterised by the presence of two nearly symmetrical cusps that are of similar size and shape, allowing relatively balanced valve function despite the abnormal structure.
- Fusion-type bicuspid: In this type, which arises due to congenital fusion during development, two of the three original cusps are partially or completely fused together, resulting in one abnormally large cusp and one smaller cusp, often leading to uneven blood flow and an increased risk of valve dysfunction over time.
In rare cases, the aortic valve may have only one cusp (unicuspid) or four cusps (quadricuspid). These variants are often associated with more severe valve dysfunction.
Causes and Risk Factors of Bicuspid Aortic Valve
- Congenital defect: BAV is a congenital condition, meaning it develops during the early stages of foetal heart formation. The exact cause is not always known.
- Genetic factors: There appears to be a strong genetic component to BAV. The condition often runs in families, with up to 25% of first-degree relatives also affected.
- Male sex: Males are more likely than females to have a bicuspid aortic heart valve.
- Associated heart conditions: BAV frequently occurs alongside other congenital heart defects, such as coarctation of the aorta (narrowing of the aorta) or abnormalities in the coronary arteries.
- Family history: Having a family history of congenital heart defects increases the risk of developing BAV and related vascular problems.
Symptoms and Clinical Presentation
Many people with a bicuspid aortic valve do not experience symptoms until adulthood, when the valve's abnormal structure begins to cause progressive problems.
Common signs and symptoms may include:
- Chest pain or discomfort
- Shortness of breath, especially with exertion
- Fatigue or reduced exercise tolerance
- Heart murmur (an abnormal whooshing sound heard through a stethoscope)
- Lightheadedness or fainting
- Palpitations or abnormal heart rhythms
- High blood pressure
- Aortic aneurysm (abnormal dilation or bulging of the aorta)
It's important to note that these symptoms can also be associated with other heart conditions. If you experience any concerning symptoms, it's crucial to consult a doctor for proper evaluation and diagnosis.
Heart Murmur Detection
In many cases, a bicuspid aortic valve is first suspected when a doctor detects a heart murmur during a routine physical exam. The abnormal valve structure can cause turbulent blood flow, which creates a characteristic whooshing sound. If a murmur is heard, further testing with an echocardiogram (ultrasound of the heart) can confirm the presence of a bicuspid valve and assess its function.
While a heart murmur doesn't always indicate significant valve disease, it does signal the need for ongoing monitoring. Regular check-ups with a cardiologist can help track the valve's condition and determine if and when treatment may be necessary.
Diagnostic Evaluation
Diagnosing a bicuspid aortic valve requires a thorough cardiac assessment to confirm the structural abnormality and evaluate its impact on heart function. The diagnostic process starts with a detailed medical history, focusing on family history of heart defects and any symptoms like chest pain or shortness of breath.
An echocardiogram is the gold standard for confirming bicuspid aortic valve diagnosis, using ultrasound to visualise the valve structure, blood flow patterns, and any associated issues like stenosis or regurgitation.
After confirming a bicuspid aortic valve, patients typically undergo CT or MRI scanning to assess aortic size, shape, and wall integrity, detecting aneurysms or dilation. The evaluation also screens for related conditions that often occur with bicuspid aortic valves, such as coarctation of the aorta, genetic syndromes like Turner syndrome, and other heart defects. Regular diagnostic reassessment is crucial because the valve's condition can worsen over time, requiring adjustments to management approaches.
Tests for Bicuspid Aortic Valve Diagnosis
- Echocardiogram (Transthoracic and Transesophageal): Uses ultrasound to visualise valve structure, measure blood flow, assess stenosis or regurgitation severity, and evaluate heart size and function.
- Cardiac CT Scan: Provides high-resolution 3D imaging of the aortic valve, root, and ascending aorta to measure dimensions and detect aneurysms, calcification, or dilation.
- Cardiac MRI: Offers precise measurements of heart volumes, valve function, blood flow, and aortic dimensions without radiation.
- Electrocardiogram (ECG/EKG): Records the heart's electrical activity to identify arrhythmias, ventricular hypertrophy, or abnormalities associated with valve disease.
- Exercise Stress Test: Evaluates the heart's response to physical exertion, revealing exercise-induced symptoms and assessing functional capacity.
- Chest X-ray: Shows heart size, aortic contour, and any pulmonary congestion indicating heart failure.
Here are some tests you can book with Metropolis Healthcare:
- Cardiac Test (Heart Screen)
- Cardiac Screen-1
- Cardiac Risk Profile Test
- Cardiac Injury Profile-Maxi
When to Treat a Bicuspid Aortic Valve
- When the valve becomes very narrow and causes chest pain, shortness of breath, fainting, or reduced exercise tolerance, indicating the heart can no longer compensate for the obstruction.
- When the leaking valve leads to symptoms or objective signs of left ventricular dysfunction, enlargement, or decreased ejection fraction on imaging.
- When the ascending aorta or root diameter reaches surgical thresholds — typically 5.0–5.5 cm, or ≥4.5 cm if concomitant valve surgery is planned — due to risk of dissection or rupture, even without valve dysfunction.
- When serial imaging shows accelerated worsening of valve function or aortic dimensions over relatively short periods.
- When severe stenosis or regurgitation exists without symptoms but causes measurable decline in heart function, significant ventricular enlargement, or other cardiac complications.
- When a patient with a bicuspid aortic valve requires coronary bypass or other heart procedures, simultaneously addressing the valve may be recommended.
- When the valve gets infected, often necessitating replacement after appropriate antibiotic therapy.
Medical Management and Monitoring
For patients with bicuspid aortic valve who do not yet require surgery, careful medical management and systematic monitoring are essential. The main goals are preventing complications, slowing disease progression, and detecting changes early to optimise surgical timing when needed.
Patients without significant valve dysfunction or aortic enlargement typically have echocardiograms every 1-2 years, while those with moderate disease or aortic dilation need more frequent monitoring, often annually or semi-annually. Controlling blood pressure is critical, as hypertension accelerates both valve deterioration and aortic expansion. Blood pressure should be optimally controlled below 130/80 mmHg, typically with beta-blockers or angiotensin receptor blockers (ARBs), which reduce aortic wall stress.
While no medications can reverse bicuspid aortic valve disease or definitively prevent progression, managing cardiovascular risk factors like cholesterol, diabetes, and smoking helps optimise overall heart health and may slow advancement.
Patients should know warning signs that warrant immediate medical attention, including new or worsening chest pain, marked shortness of breath, fainting, or rapid heart palpitations.
Surgical and Interventional Options
- Aortic Valve Repair: Involves reconstructing the bicuspid valve to improve function while preserving the patient's native tissue, though this is technically challenging and not always feasible depending on valve anatomy.
- Mechanical Aortic Valve Replacement: Involves replacing the diseased valve with a durable prosthesis that can last for decades but requires lifelong anticoagulation with warfarin to prevent blood clots.
- Bioprosthetic (Tissue) Valve Replacement: Utilises animal-derived tissue valves that generally do not require long-term anticoagulation but have a limited lifespan, typically 10–20 years.
- Ross Procedure: A complex operation replacing the aortic valve with the patient's pulmonary valve, then replacing the pulmonary valve with a donor valve, preserving living tissue in the aortic position.
- ranscatheter Aortic Valve Replacement (TAVR): A minimally invasive procedure in which a replacement valve is delivered via catheter, primarily used in select bicuspid cases with favourable anatomy, though open surgery remains the standard in most younger patients.
- Aortic Root Replacement: Surgical replacement of the enlarged aortic root along with the valve, using a composite graft including both valve and aortic segment, necessary when root dilation exceeds safe dimensions.
- Valve-Sparing Aortic Root Replacement: Sophisticated technique replacing the dilated aortic root while preserving the patient's aortic valve, avoiding a prosthetic valve when leaflets remain healthy.
Lifestyle and Prevention Strategies
- Maintain a heart-healthy diet low in saturated fats, trans fats, sodium, and added sugars
- Engage in regular physical activity as tolerated and approved by your cardiologist
- Achieve and sustain a healthy weight to reduce strain on the heart and valve
- Manage stress through relaxation techniques, mindfulness, or professional counselling.
- Control blood pressure, cholesterol, and blood sugar levels through lifestyle changes and medications as needed
- Avoid smoking and excessive alcohol consumption, which can worsen cardiovascular health
- Practice good dental hygiene and get regular dental check-ups to prevent endocarditis
- Attend all scheduled follow-up appointments with your cardiology team
- Learn to recognise and promptly report any new or concerning cardiovascular symptoms
- Consider genetic counselling and testing if you have a family history of bicuspid aortic valve or other congenital heart defects to guide screening for relatives
Prognosis and Long-Term Outlook
The prognosis for individuals with bicuspid aortic valve varies depending on the severity of the valve abnormality, the presence of associated conditions, and the timeliness of intervention when needed. With proper monitoring, medical management, and timely surgical treatment, many patients with this condition can lead full, active lives. However, bicuspid aortic valve is a lifelong disorder that requires ongoing surveillance and care.
Advances in surgical techniques, including valve-sparing and endovascular approaches, have substantially improved long-term outcomes and survival for patients undergoing intervention However, individuals with bicuspid aortic valve remain at increased risk for complications such as aortic aneurysm, dissection, infective endocarditis, and heart failure compared with the general population. Regular follow-up with a cardiologist specialising in adult congenital heart disease is essential to monitor valve function, assess for related conditions, and make personalised recommendations for management and intervention.
At Metropolis Healthcare, we understand the importance of early detection and management of heart conditions. With a presence in over 750 towns in India, supported by a robust network of more than 220 laboratories, 4600+ service centres, and over 10,000 touchpoints, Metropolis is committed to delivering accurate diagnostic services and personalised care. Our philosophy, rooted in technological innovation, patient-centric care, and reliable diagnostic reporting, has set industry benchmarks for accuracy and efficiency that you can trust.
FAQs
How common is a bicuspid aortic valve?
Bicuspid aortic valve is the most common congenital heart defect, affecting about 1-2% of the population. It is more prevalent in males than females.
Can a bicuspid aortic valve be inherited?
Yes, bicuspid aortic valve can run in families, suggesting a genetic component. First-degree relatives of affected individuals have a higher risk and should be screened with echocardiography.
What are the warning signs of a severe bicuspid aortic valve?
Warning signs include chest pain, shortness of breath (especially with exertion), fainting or lightheadedness, palpitations, fatigue, and declining exercise tolerance. Seek prompt medical attention for these symptoms.
When is surgery needed for bicuspid aortic valve disease?
Surgery is recommended for severe stenosis or regurgitation causing symptoms, left ventricular dysfunction, aortic enlargement, or rapid progression. Significant aortic dilation (>5.5 cm) may also warrant surgery to prevent rupture or dissection.
Can lifestyle changes slow bicuspid aortic valve progression?
While lifestyle changes can't reverse the valve abnormality, controlling blood pressure, maintaining a healthy weight, not smoking, and exercising regularly may help slow complications like aortic dilation or heart failure.
What follow-up is needed after bicuspid aortic valve repair?
Lifelong surveillance with regular echocardiograms and advanced imaging (MRI/CT) is essential to monitor valve function, heart size, and aortic dimensions. Your doctor will recommend a follow-up schedule based on your specific situation.
References
- https://my.clevelandclinic.org/health/diseases/16780-bicuspid-aortic-valve-disease
- https://www.achaheart.org/your-heart/educational-qas/types-of-heart-defects/bicuspid-aortic-valve-bav/
- https://www.mayoclinic.org/diseases-conditions/bicuspid-aortic-valve/cdc-20385577
- https://medlineplus.gov/ency/article/007325.htm




























