Preventive Healthcare
Ventricular Fibrillation: Causes, Symptoms, and Risk Factors Explained
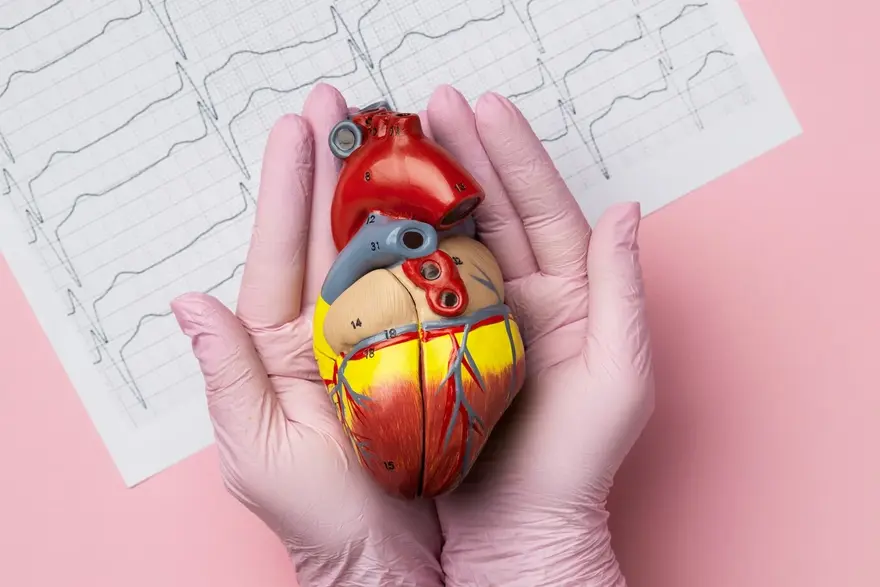
Table of Contents
- What is Ventricular Fibrillation?
- How Does Ventricular Fibrillation Differ from Other Arrhythmias?
- Causes and Risk Factors of Ventricular Fibrillation
- Symptoms of Ventricular Fibrillation
- Diagnosis of Ventricular Fibrillation
- Treatment Options for Ventricular Fibrillation
- Living with Ventricular Fibrillation: What to Expect
- Prevention Strategies for Ventricular Fibrillation
- Conclusion: The Importance of Awareness and Action
What is Ventricular Fibrillation?
Ventricular fibrillation is a life-threatening heart rhythm disorder that requires immediate medical attention. This condition occurs when the heart's lower chambers (ventricles) quiver chaotically, disrupting the heart's ability to pump blood effectively throughout the body. Without prompt treatment, ventricular fibrillation can lead to sudden cardiac arrest and death. Understanding the causes, symptoms, and risk factors associated with this serious arrhythmia is crucial for timely intervention and potentially saving lives. In this article, we will explore the key aspects of ventricular fibrillation, helping you stay informed and prepared.
How Does Ventricular Fibrillation Differ from Other Arrhythmias?
While there are many types of heart rhythm disorders, ventricular fibrillation stands out due to its life-threatening nature. In ventricular fibrillation, the heart's electrical signals become rapid and erratic, causing the ventricles to quiver ineffectively rather than contract and pump blood to the body. This chaotic rhythm prevents adequate blood circulation, leading to sudden cardiac arrest if not promptly treated with defibrillation. In contrast, other arrhythmias like atrial fibrillation or premature ventricular contractions may cause irregular heartbeats but do not always stop the heart from pumping blood altogether.
Causes and Risk Factors of Ventricular Fibrillation
Several factors can contribute to the ventricular fibrillation causes, including:
- Insufficient Blood Flow to the Heart Muscle: Blocked coronary arteries during or after a heart attack can deprive the heart muscle of oxygen, leading to ventricular fibrillation.
- Damage to the Heart Muscle: Conditions like cardiomyopathy or previous heart attacks can weaken the heart, increasing the risk of ventricular fibrillation due to disrupted electrical pathways.
- Electrolyte Imbalances: Abnormal potassium or magnesium levels can disturb the heart's electrical signals, triggering ventricular fibrillation.
- Drug Toxicity: Drugs like cocaine, methamphetamines, and certain medications can affect the heart’s electrical activity, contributing to ventricular fibrillation.
- Electrocution or Trauma: Severe physical trauma or electrocution can directly impact the heart’s electrical system, leading to ventricular fibrillation.
- Sepsis and Infections: Severe infections, especially sepsis, can weaken heart function and increase the risk of ventricular fibrillation.
Here are the risk factors for ventricular fibrillation:
- Previous episodes of ventricular fibrillation
- Having a family history of heart disease or arrhythmias
- Inherited conditions such as long QT syndrome or Brugada syndrome
- A weakened heart muscle (cardiomyopathy)
- Certain medicines that affect heart function
Symptoms of Ventricular Fibrillation
The ventricular fibrillation symptoms can come on suddenly and may include:
- Sudden collapse or loss of consciousness
- Absence of pulse or heartbeat
- Gasping or not breathing
- Chest pain or discomfort (may occur shortly before the onset of ventricular fibrillation)
- Dizziness or lightheadedness
- Rapid or pounding heartbeat (may precede the arrhythmia)
It's important to note that ventricular fibrillation often leads to cardiac arrest within seconds, so prompt recognition and medical attention are vital.
Diagnosis of Ventricular Fibrillation
Diagnosing ventricular fibrillation typically occurs in emergency situations and involves:
- Physical Examination: Doctors will assess the person's responsiveness, breathing, and circulation to determine the presence of cardiac arrest.
- Medical History: Information about pre-existing heart conditions, medications, and family history can help guide the diagnosis and treatment approach.
- Electrocardiogram (ECG or EKG): The primary diagnostic tool for ventricular fibrillation. An ECG shows rapid, erratic electrical activity with no identifiable P waves, QRS complexes, or T waves and a heart rate typically between 300-400 beats per minute.
- Echocardiogram: Uses ultrasound to assess the heart’s structure and function, helping to identify potential underlying heart issues contributing to ventricular fibrillation.
- Blood Tests: Help detect heart damage by measuring enzymes released during a heart attack, such as troponin, and can also identify electrolyte imbalances.
- Imaging Tests (MRI or CT scans): May be used to assess the heart’s condition and identify underlying causes, such as blockages or structural abnormalities.
Rapid diagnosis is essential to initiate appropriate treatment and improve the chances of survival.
Treatment Options for Ventricular Fibrillation
Prompt ventricular fibrillation treatment is critical for survival. The main approaches include:
- Defibrillation: Delivering a controlled electric shock to the heart to reset its rhythm. This is done using an automated external defibrillator (AED) or by medical professionals.
- Cardiopulmonary Resuscitation (CPR): Performing chest compressions and rescue breaths to manually circulate oxygenated blood until an AED arrives or until the person can receive advanced life support measures.
- Medications: Administering anti-arrhythmic drugs like amiodarone or lidocaine to help stabilise the heart rhythm and prevent recurrence of ventricular fibrillation.
- Implantable Cardioverter Defibrillator (ICD): Surgically placing a battery-powered device under the skin to continuously monitor heart rhythms and deliver a shock if it detects ventricular fibrillation. ICDs are often recommended for people at high risk of sudden cardiac arrest.
- Treating Underlying Conditions: Addressing heart disorders, electrolyte imbalances, or other health issues that raise the risk of ventricular fibrillation. This may involve procedures like coronary angioplasty, heart valve surgery, or medication adjustments.
The specific treatment plan depends on the individual's overall health, the cause of ventricular fibrillation, and the severity of the episode.
Living with Ventricular Fibrillation: What to Expect
Surviving ventricular fibrillation often requires ongoing management and lifestyle adjustments, such as:
- Regular check-ups to monitor heart health and adjust treatment as needed
- Lifestyle changes like eating a heart-healthy diet, exercising regularly, reducing stress, and avoiding tobacco and excessive alcohol
- Taking prescribed medications consistently to control arrhythmias and treat related conditions
- Learning to recognise warning signs and being prepared to respond to a cardiac emergency
- Wearing a medical alert bracelet and informing family, friends, and co-workers about your condition.
Prevention Strategies for Ventricular Fibrillation
Preventing ventricular fibrillation involves addressing risk factors and promoting heart health through:
- Managing underlying cardiovascular conditions, such as coronary artery disease, heart failure, and hypertension.
- Adopting a heart-healthy lifestyle, including a balanced diet, regular physical activity, and avoiding smoking and excessive alcohol consumption.
- Controlling diabetes, obesity, and other conditions that can impact heart health.
- Following a prescribed medication regimen and reporting any adverse effects to a doctor.
- Learning CPR and familiarising oneself with the ventricular fibrillation meaning and location of AEDs in frequently visited places.
While not all cases of ventricular fibrillation can be prevented, these strategies can significantly lower the risk and improve overall cardiovascular well-being.
Conclusion: The Importance of Awareness and Action
Ventricular fibrillation is a serious and potentially life-threatening heart rhythm disorder that demands swift recognition and intervention. By understanding the causes, symptoms, and risk factors associated with this condition, individuals can be better prepared to respond effectively and seek timely ventricular fibrillation treatment. Awareness also plays a crucial role in prevention, as adopting heart-healthy habits and managing underlying cardiovascular issues can reduce the likelihood of developing ventricular fibrillation. If you or someone around you experiences symptoms suggestive of this arrhythmia, call emergency services immediately and be prepared to perform CPR if needed.
If you have concerns about your heart health or wish to assess your risk factors, consider reaching out to Metropolis Healthcare. As a leading diagnostic laboratory chain in India, we offer comprehensive cardiac health check-ups and advanced blood tests to help you stay informed about your cardiovascular well-being. Our team of experienced phlebotomists can conveniently collect samples from the comfort of your home, ensuring a hassle-free experience. Take charge of your heart health today and book an appointment with Metropolis Healthcare for personalised care and reliable diagnostic services.




























