Preventive Healthcare
Peritonitis: Causes, Symptoms, And Treatment
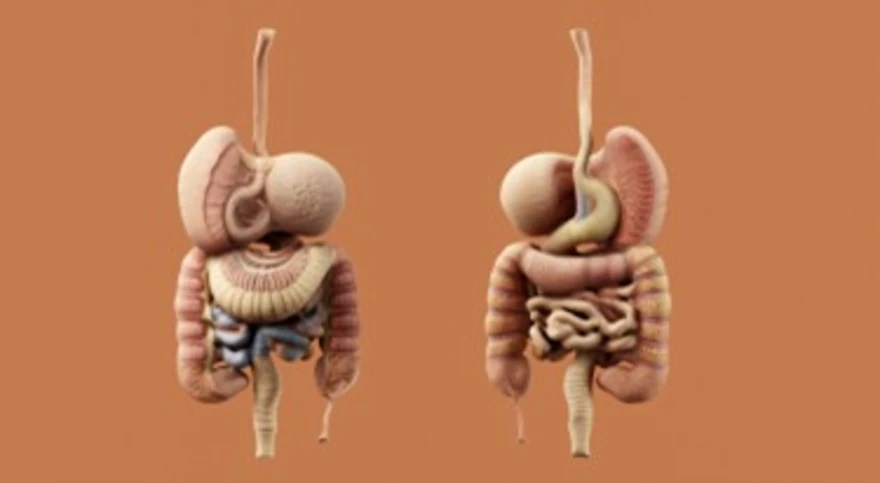
Table of Contents
- What Is Peritonitis?
- Types of Peritonitis
- Causes of Peritonitis
- Symptoms of Peritonitis
- Complications of Peritonitis
- How Peritonitis Is Diagnosed
- Tests for Peritonitis
- Treatment for Peritonitis
- Peritonitis in Peritoneal Dialysis Patients
- Recovery & Post-Treatment Care
- Prevention of Peritonitis
- When to Seek Immediate Medical Help
- Conclusion
- FAQs
- References
What Is Peritonitis?
The peritoneum is a thin, double-layered membrane lining the abdominal cavity and covering most abdominal organs, including the stomach, intestines, and liver. It also helps lubricate and protect these organs. When this membrane becomes inflamed or infected, it leads to peritonitis — a potentially life-threatening condition marked by severe abdominal pain, fever, and swelling.
The condition may arise suddenly (acute peritonitis) or gradually over time (chronic peritonitis). Early symptoms can mimic other abdominal conditions, so accurate diagnosis is vital for proper treatment.
Types of Peritonitis
Peritonitis can occur in several forms depending on its cause and underlying condition:
- Primary (Spontaneous) Peritonitis: This occurs when infection develops without any clear perforation or injury in the abdomen, as described in NIH clinical summaries. It’s most common in people with liver cirrhosis and fluid build-up (ascites), allowing bacteria to spread from the bloodstream into the peritoneal fluid.
- Secondary Peritonitis: It is the most common type; it develops when an abdominal organ ruptures (like the appendix, stomach, or colon) and releases bacteria or digestive fluids into the peritoneal cavity.
- Dialysis-Associated Peritonitis: Found in patients undergoing peritoneal dialysis for kidney failure. Infections can occur if bacteria enter through the dialysis catheter or tubing.
- Tuberculous Peritonitis: Caused by Mycobacterium tuberculosis infection spreading from the lungs or lymph nodes into the abdominal cavity. It is more common in developing regions.
Causes of Peritonitis
Peritonitis causes vary depending on whether the infection is spontaneous or due to an underlying condition.
Common causes include:
- Rupture of an appendix, stomach or intestinal ulcer, or diverticulum, allowing bacteria or digestive contents to enter the peritoneal cavity.
- Abdominal trauma or injury allows infection to enter.
- Post-surgical complications, especially if the intestinal wall is accidentally perforated.
- Liver cirrhosis with ascites, where bacteria travel through the blood or lymphatic fluid.
- Peritoneal dialysis, particularly when sterile technique is compromised, may introduce infection through the catheter.
- Pelvic inflammatory disease (PID) or infection after childbirth or miscarriage.
- An infected gallbladder or pancreas (cholecystitis or pancreatitis) is leaking digestive fluids.
- Bacterial infection spreads from other organs, like the kidneys or intestines.
Symptoms of Peritonitis
The symptoms of peritonitis can appear suddenly and intensify rapidly.
Common warning signs include:
- Sharp, severe abdominal pain that worsens with movement or touch.
- Swelling and tenderness in the abdomen.
- Fever and chills due to infection.
- Nausea, vomiting, or loss of appetite.
- Difficulty passing gas or stool (sign of intestinal paralysis or ileus).
- Fatigue, weakness, or confusion in severe cases.
- Rapid heartbeat and shallow breathing.
- Reduced urine output, indicating dehydration or kidney stress.
Peritonitis is a medical emergency — delay in treatment can rapidly lead to sepsis and septic shock, both potentially fatal if untreated.
Complications of Peritonitis
If peritonitis is not treated promptly, several serious complications can occur:
- Sepsis: Infection spreading throughout the body, potentially leading to multiple organ failure.
- Abscess formation: Pockets of pus within the abdomen that may require surgical drainage.
- Adhesions: Scar tissue formation that can cause bowel obstruction later.
- Chronic kidney or liver problems due to prolonged infection.
- Prolonged hospitalisation or recurrent infections, particularly in dialysis patients.
How Peritonitis Is Diagnosed
Diagnosis involves multiple steps to identify the infection source and its severity:
- Physical Examination: Doctors check for tenderness, swelling, and guarding (when abdominal muscles tighten in response to touch).
- Blood Tests: Detect elevated white blood cell count, inflammation markers, and organ function changes.
- Imaging Tests: X-rays, ultrasounds, or CT scans help locate abscesses, fluid accumulation, or perforation.
- Peritoneal Fluid Analysis: A small sample of abdominal fluid is collected through paracentesis and tested for bacteria, pus, or chemical abnormalities.
- Urine or Stool Test: Used to rule out infections in nearby organs like the bladder or intestines.
- Culture Tests: Identify the specific bacteria causing the infection to guide antibiotic selection.
Tests for Peritonitis
Comprehensive testing services are available to help detect and monitor peritonitis and related conditions:
- Complete Blood Count (CBC): checks for elevated infection markers.
- Kidney and Liver Function Tests: Assess organ performance and detect early signs of dysfunction.
- Culture and Sensitivity Test: identifies the bacteria responsible for infection.
- Ultrasound Abdomen/CT Abdomen: It visualises fluid accumulation or perforation sites.
Treatment for Peritonitis
The following are the commonly used peritonitis treatment methods:
1. Antibiotic Therapy
Immediate intravenous broad-spectrum antibiotics are initiated to control the infection. Once laboratory results confirm the bacterial type, targeted antibiotics are used. In fungal peritonitis, antifungal medications may be prescribed. Treatment usually continues for 10–14 days, depending on infection severity.
2. Surgical Management
Surgery may be required in secondary peritonitis to remove the source of infection. This can involve:
- Repairing a ruptured appendix or ulcer.
- Removing infected tissue or drainage of abscesses.
- Flushing the abdominal cavity with sterile fluid to remove bacteria.
Post-surgery, patients are monitored closely for recurrence, and drainage tubes may remain temporarily to prevent fluid build-up.
Peritonitis in Peritoneal Dialysis Patients
For individuals on peritoneal dialysis (PD), peritonitis is one of the most frequent but largely preventable complications. Infection occurs if bacteria enter through the dialysis catheter.
Preventive care includes:
- Practising strict hygiene during dialysis exchange.
- Using masks and sterile gloves.
- Disinfecting connection sites properly.
Prompt administration of intraperitoneal antibiotics can often resolve infection while allowing dialysis to continue, but recurrent infections may require catheter removal or switching to haemodialysis.
Recovery & Post-Treatment Care
Once the infection is under control, recovery involves close monitoring and lifestyle care:
- Complete the full course of prescribed antibiotics.
- Attend follow-up visits and repeat imaging if needed.
- Consume a balanced, protein-rich diet and maintain adequate hydration to promote recovery.
- Avoid strenuous activity or abdominal strain until cleared by your doctor.
- Maintain wound hygiene and report any new pain or fever immediately.
- Patients on dialysis should review their catheter care techniques with medical staff regularly.
Recovery time can vary from two to six weeks, depending on the cause and overall health.
Prevention of Peritonitis
While not all cases are preventable, risk can be reduced through:
- Maintaining hygiene during peritoneal dialysis.
- Treating stomach ulcers, appendicitis, or gallstones early.
- Avoiding unnecessary abdominal surgeries.
- Managing chronic liver conditions and ascites under medical supervision.
- Ensuring all surgical equipment is sterile.
- Seeking prompt medical help for persistent abdominal pain or fever.
When to Seek Immediate Medical Help
Seek emergency care if you experience:
- Sudden, severe, or persistent abdominal pain
- Persistent vomiting, fever, or chills
- Swollen or hard abdomen
- Difficulty breathing or confusion
Individuals with liver disease, abdominal surgery, or dialysis catheters are at higher risk and must seek immediate evaluation to prevent life-threatening complications.
Conclusion
Peritonitis is a serious medical condition that requires urgent diagnosis and treatment. Early medical intervention with antibiotics and surgery greatly improves recovery outcomes and prevents complications like sepsis.
At Metropolis Healthcare, our advanced diagnostic network and expert pathologists ensure timely, accurate results for effective management. With 10,000+ home collection touchpoints and specialised infection testing panels, you can rely on Metropolis to safeguard your health from detection to recovery.
FAQs
What is a red flag for peritonitis?
Severe, constant abdominal pain with fever, vomiting, and abdominal rigidity is a red flag requiring urgent attention.
Is peritonitis life-threatening?
Yes. Untreated peritonitis can lead to sepsis, multi-organ failure, and death. Timely treatment ensures full recovery in most cases.
How is peritonitis diagnosed?
Peritonitis is diagnosed through physical examination for tenderness and swelling, blood tests for infection, imaging (CT or ultrasound), and peritoneal fluid analysis through paracentesis.
How long does it take to recover from peritonitis?
Most patients recover within 2–6 weeks, depending on infection severity, treatment type, and overall health condition.
Can peritonitis be prevented?
It cannot be completely prevented, but with proper care, you can avoid it. You must maintain sterile technique during dialysis, seek prompt care for abdominal pain, treat ulcers, appendicitis, or gallbladder disease early, and follow good post-surgical hygiene practices.
What is the survival rate for peritonitis?
With timely treatment, 70–80% of patients recover completely. Delayed diagnosis or sepsis significantly lowers survival rates.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4836582/
- https://my.clevelandclinic.org/health/diseases/17831-peritonitis
- https://www.mayoclinic.org/diseases-conditions/peritonitis/symptoms-causes/syc-20376247
- https://www.webmd.com/digestive-disorders/peritonitis-symptoms-causes-treatments




























