Preventive Healthcare
Oral Thrush: Causes, Symptoms & How to Treat It Effectively
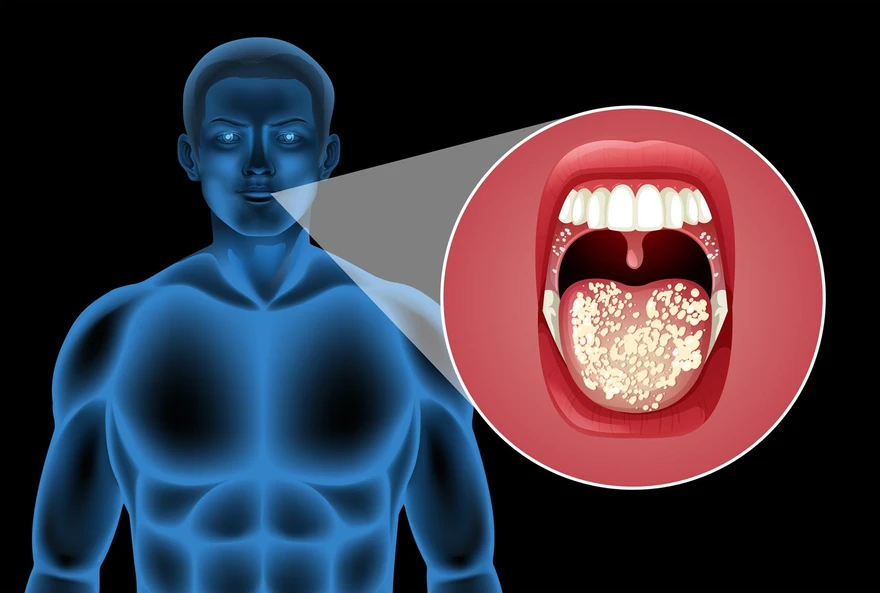
Table of Contents
- What Is Oral Thrush?
- Common Causes of Oral Thrush
- Who Is at Risk for Oral Thrush?
- Symptoms of Oral Thrush
- How Is Oral Thrush Diagnosed?
- Tests Used to Diagnose Oral Thrush
- Effective Treatment for Oral Thrush
- Preventing Oral Thrush
- Oral Thrush in Babies
- Oral Thrush in Older Adults
- Oral Thrush and Diabetes
- Conclusion
- FAQs
- References
What Is Oral Thrush?
Oral thrush is a fungal infection caused by Candida, most commonly Candida albicans. It develops when yeast overgrows inside the mouth, affecting the tongue, gums, inner cheeks, roof of the mouth, and sometimes the throat. It appears as creamy white patches, redness, or soreness and is more common in babies, older adults, and people with weakened immune system. While mild cases clear quickly with treatment, persistent or severe oral thrush may indicate an underlying health condition that needs medical attention.
Common Causes of Oral Thrush
Understanding oral thrush causes helps you identify risk factors and take preventive measures. Oral thrush is caused by several factors that disrupt your mouth's natural bacterial balance:
• Antibiotic use: These medications kill beneficial bacteria that normally keep Candida in check.
• Weakened immune system: Due to HIV/AIDS, cancer treatments, or immunosuppressive medications.
• Diabetes: High blood sugar levels create an environment where yeast thrives.
• Corticosteroid medications: Particularly inhaled steroids used for asthma treatment.
• Poor oral hygiene: Inadequate brushing and flossing allow harmful microorganisms to flourish.
• Dry mouth: Reduced saliva production from medications or medical conditions.
• Dentures: Especially if they don't fit properly or aren't cleaned regularly.
• Hormonal changes: During pregnancy or from contraceptive use.
Who Is at Risk for Oral Thrush?
Certain groups face higher risks of developing thrush due to various health and lifestyle factors:
• Infants and young children: Their developing immune systems offer less protection.
• Adults over 60: Age-related immune decline increases vulnerability.
• People with diabetes: Poorly controlled blood sugar promotes yeast growth.
• Cancer patients: Chemotherapy and radiation weaken the body’s immune defenses.
• Individuals taking antibiotics: These disrupt protective bacterial populations.
• Denture wearers: Especially those with poor denture hygiene.
• Smokers: Tobacco use damages the mouth tissues and reduces immunity.
• People with nutritional deficiencies: Particularly iron, vitamin B12, or folate deficiency.
The NIH notes that oral thrush commonly develops when Candida fungi multiply excessively in weakened immune conditions, such as during chemotherapy, radiotherapy, diabetes, or prolonged antibiotic use.
Symptoms of Oral Thrush
Recognizing oral thrush symptoms early enables prompt treatment and helps prevent complications. The most common signs include:
• White patches: Creamy, cottage cheese-like lesions on the tongue, cheeks, or gums
• Redness and soreness: Inflamed tissues beneath the white patches
• Bleeding: When patches are wiped away, the underlying tissue may bleed.
• Loss of taste: Reduced ability to taste foods properly
• Dry mouth sensation: Feeling like your mouth lacks adequate moisture
• Cracked corners: Painful splits at the corners of your mouth
• Difficulty swallowing: If infection spreads to your throat
• Pain while eating: Discomfort when consuming acidic or spicy foods
How Is Oral Thrush Diagnosed?
Healthcare providers typically diagnose thrush through a systematic approach:
- Visual examination: Your doctor examines your mouth for characteristic white patches and areas of redness.
- Medical history review: Discussion of recent antibiotic use, medical conditions, and symptoms.
- Physical scraping: Gentle removal of patches to examine cells under a microscope.
- Throat culture test: Laboratory analysis of mouth swabs to identify specific fungi.
- Blood tests: To check for underlying conditions like diabetes or immune disorders.
Tests Used to Diagnose Oral Thrush
Several diagnostic tools help confirm thrush and rule out other conditions:
• Microscopic examination: Direct visualization of Candida cells from mouth scrapings
• Throat culture test: Growing organisms from mouth swabs in laboratory conditions
• Endoscopy: Camera examination of throat and oesophagus if symptoms suggest spread
• Biopsy: Tissue sample analysis when diagnosis remains unclear
• Blood glucose testing: To identify undiagnosed diabetes as an underlying cause
Effective Treatment for Oral Thrush
Oral thrush treatment varies depending on the severity of your infection and overall health status. Most cases respond well to antifungal medications, with treatment typically lasting 7–14 days. Your healthcare provider will choose the most appropriate approach based on your specific circumstances.
Early-stage oral thrush often responds well to topical antifungal treatments, while more severe infections may require oral or systemic antifungal medications. Success depends on addressing underlying causes and maintaining good oral hygiene throughout treatment.
Home Remedies for Oral Thrush
Several natural approaches can support conventional oral thrush treatment:
• Salt water rinses: Mix half a teaspoon of salt in warm water and rinse gently.
• Baking soda rinses: Create a mild alkaline environment that discourages yeast growth.
• Probiotic yogurt: Contains beneficial bacteria that help restore natural balance.
• Coconut oil pulling: Swishing coconut oil may have antifungal properties.
• Good oral hygiene: Regular brushing and flossing help prevent bacterial and fungal buildup.
• Sugar reduction: Limiting sweet foods reduces nutrients available to yeast.
Medications for Treating Oral Thrush
Healthcare providers prescribe various antifungal medications based on infection severity:
• Nystatin: Topical antifungal liquid or lozenges for mild infections
• Clotrimazole: Dissolving tablets that coat affected mouth areas
• Fluconazole: Oral tablets for moderate to severe thrush
• Itraconazole: Alternative oral medication for resistant infections
• Amphotericin B: Reserved for severe cases or immunocompromised patients
Preventing Oral Thrush
Prevention strategies focus on maintaining healthy mouth bacteria and addressing risk factors:
• Practice excellent oral hygiene: Brush twice daily and floss regularly.
• Clean dentures properly: Remove and disinfect nightly if you wear dentures.
• Manage underlying conditions: Control diabetes and treat dry mouth.
• Use antibiotics judiciously: Only take prescribed antibiotics when necessary.
• Rinse after inhaler use: Clean your mouth after using steroid inhalers.
• Maintain good nutrition: Eat a balanced diet rich in vitamins and minerals.
• Stay hydrated: Adequate fluid intake supports healthy saliva production.
• Avoid tobacco products: Smoking increases infection risk.
When to See a Doctor for Oral Thrush
Seek medical attention if symptoms last longer than one week, worsen, or keep returning. Also consult a doctor if you experience difficulty swallowing, fever, or white patches spreading to the throat, as these may suggest a deeper yeast infection needing medical treatment.
Oral Thrush in Babies
Babies often develop oral thrush due to an immature immune system. Symptoms include white patches on the tongue or gums, fussiness, and refusal to feed. Breastfeeding mothers may feel nipple pain if the infection spreads. Treatment includes antifungal drops and sterilising pacifiers and bottles to prevent reinfection.
Oral Thrush in Older Adults
Older adults are more prone to thrush due to dentures, dry mouth, medications, and chronic health conditions. Managing dry mouth, improving denture hygiene, and regular dental visits help reduce recurrence. Persistent thrush may indicate diabetes or weakened immune system.
Oral Thrush and Diabetes
People with poorly controlled diabetes are at higher risk because high sugar levels help Candida grow faster. Thrush may be an early sign of uncontrolled blood glucose. Maintaining good sugar control and oral hygiene significantly reduces the risk of recurrent infections.
Conclusion
Oral thrush is a common and easily treatable condition among babies and adults alike, and early diagnosis helps relieve discomfort and prevent complications. Recognizing early symptoms and addressing underlying causes can help prevent recurrence. With simple lifestyle adjustments, maintaining proper oral hygiene, and consistent care, most people can fully recover and maintain a healthy, balanced oral environment.
Metropolis Healthcare offers reliable support with 4,000+ tests, such as throat culture, biopsy, or follow-up blood work, full-body checkups, advanced specialty testing, and accurate, quick-turnaround results. With safe home sample collection, 10,000+ touchpoints, and easy booking through our website, app, call, or WhatsApp, we make high-quality diagnostics accessible and convenient, so you can manage your health with confidence.
FAQs
How long does oral thrush last?
Most cases improve within 7–14 days with proper antifungal treatment. Severe or recurrent infections take longer and may require additional evaluation.
Can oral thrush spread to others?
Oral thrush is not highly contagious, but it can spread through close contact such as kissing, sharing utensils, or breastfeeding. Good hygiene reduces risk.
Is oral thrush the same as a yeast infection?
Yes. Oral thrush is a type of yeast infection caused by Candida overgrowth inside the mouth. The same fungus can cause infections in other body areas.
How do you treat oral thrush in babies?
Pediatric treatment includes antifungal drops, sterilizing pacifiers, cleaning feeding bottles, and treating breastfeeding mothers if needed to prevent reinfection.
References
- https://www.ncbi.nlm.nih.gov/books/NBK367586/
- https://www.mayoclinic.org/diseases-conditions/oral-thrush/symptoms-causes/syc-20353533
- https://www.nhs.uk/conditions/oral-thrush-mouth-thrush/
- https://my.clevelandclinic.org/health/diseases/10956-thrush
- https://www.healthdirect.gov.au/oral-thrush