Preventive Healthcare
Demystifying Hyperhidrosis: Causes, Treatments, and Relief Options
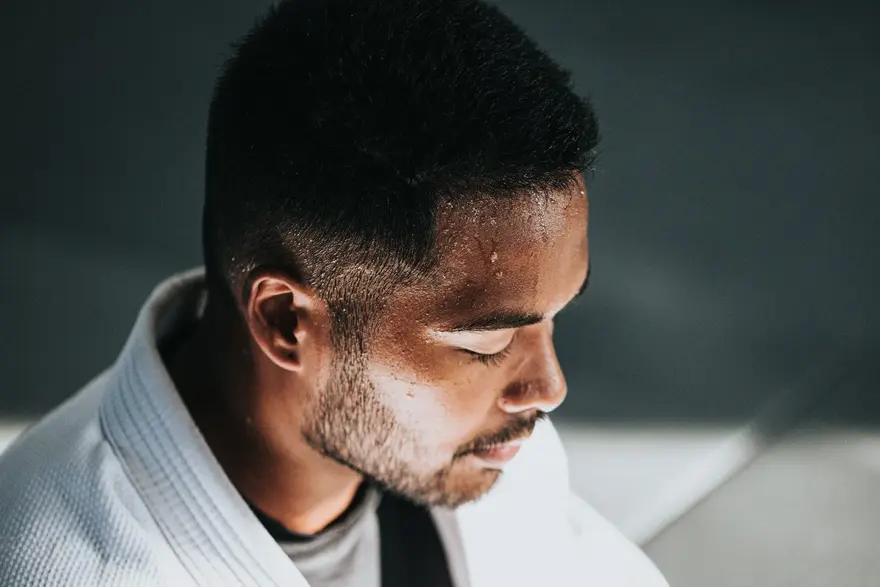
Table of Contents
- What is Hyperhidrosis?
- What are the Types of Hyperhidrosis?
- How Common is Hyperhidrosis?
- What are the Symptoms of Hyperhidrosis?
- Where Will I Have Symptoms of Hyperhidrosis?
- What Causes Hyperhidrosis?
- Does Hyperhidrosis Run in Families?
- What are the Complications of Hyperhidrosis?
- How is Hyperhidrosis Diagnosed?
- What Tests Diagnose Hyperhidrosis?
- How is Hyperhidrosis Treated?
- Are There Side Effects of the Treatment?
- How Soon After Treatment Will I Feel Better?
- Can Hyperhidrosis be Prevented?
- What Can I Expect if I Have Hyperhidrosis?
- Is There a Cure For Hyperhidrosis?
- When Should I See a Healthcare Provider?
- What Questions Should I Ask My Doctor?
- Why Does Sweat Smell Bad?
- Conclusion
Do you constantly battle excessive sweating, feeling uncomfortable and self-conscious? You are not alone! Hyperhidrosis, the condition causing relentless sweat, affects many. This article delves into hyperhidrosis, exploring its causes, symptoms and solutions. Discover how to reclaim your comfort and confidence in everyday life.
What is Hyperhidrosis?
Hyperhidrosis is a medical condition characterised by excessive sweating beyond what the body needs for temperature regulation. It results from overstimulation of cholinergic receptors on eccrine glands, leading to uncontrollable and intense sweating. This condition can affect various body parts, including the palms, soles, armpits, and groin. Individuals with hyperhidrosis experience sweating that goes beyond normal physiological needs, often occurring without a clear trigger.
The condition can significantly impact a person's daily life, leading to social discomfort and emotional distress. Moreover, there are different forms of hyperhidrosis, such as emotionally induced, localised, and generalised. The treatment options range from lifestyle adjustments and antiperspirants to medical interventions like medications and, in severe cases, surgery. Therefore, it is essential to consult a healthcare professional to determine the most suitable approach for managing hyperhidrosis.
What are the Types of Hyperhidrosis?
Hyperhidrosis is classified into two main types:
- Primary Hyperhidrosis: This type is usually inherited and unrelated to other medical conditions. It causes excessive sweating, often localised in specific areas such as palms, soles, or underarms. Primary hyperhidrosis is characterised by sweating beyond what is physiologically necessary and usually has no apparent cause.
- Secondary Hyperhidrosis: Unlike primary hyperhidrosis, secondary hyperhidrosis is associated with other underlying medical conditions. It may lead to generalised excessive sweating all over the body. Conditions like diabetes and menopause hot flashes can contribute to secondary hyperhidrosis.
How Common is Hyperhidrosis?
Hyperhidrosis is a relatively common condition, with prevalence rates varying globally. In the United States, estimates suggest a prevalence ranging from 2.8% to 4.8% of the general population.
What are the Symptoms of Hyperhidrosis?
Hyperhidrosis, or excessive sweating, manifests symptoms that can significantly impact an individual's daily life. Here are common symptoms:
- Wetness on Your Skin: Hyperhidrosis causes abnormal sweat production, resulting in a constant feeling of wetness on your skin.
- Damp Clothing: Individuals with hyperhidrosis often experience damp clothing due to the persistent and heightened levels of sweating.
- Beads of Fluid Dripping: Excessive sweating can lead to beads of fluid dripping from areas such as your cheeks or forehead, impacting daily activities and comfort.
- Itching and Inflammation: The continual exposure to sweat can irritate the skin, leading to itching and inflammation.
- Body Odor: When sweat combines with bacteria on the skin, it produces body odour, a common issue for those with hyperhidrosis.
- Cracked or Peeling Skin on Feet: Prolonged hyperhidrosis can result in cracked or peeling skin, particularly on the feet, emphasising the importance of managing this condition.
Where Will I Have Symptoms of Hyperhidrosis?
Hyperhidrosis primarily affects the following areas of the body:
- Underarms: Excessive sweating commonly occurs in the underarm region.
- Palms: Hands may experience heightened sweating.
- Face: Facial regions, including the forehead, can be affected.
- Scalp: Hyperhidrosis may lead to increased sweating on the scalp.
- Feet: Excessive sweating can be present on the feet.
These areas are the most commonly impacted by hyperhidrosis, causing noticeable and sometimes disruptive sweating.
What Causes Hyperhidrosis?
Hyperhidrosis, characterised by excessive sweating, can have various causes:
- Primary Hyperhidrosis: This form is usually localised and often hereditary. It results from faulty nerve signals triggering overactive eccrine sweat glands, commonly affecting palms, soles and underarms.
- Secondary Hyperhidrosis: Also known as generalised hyperhidrosis, it causes excessive sweating throughout the body or in larger areas. Underlying medical conditions contribute to this type. Several health issues, such as fever, hyperthyroidism, diabetes, acromegaly and neurological diseases, can also contribute to secondary hyperhidrosis.
- Lifestyle Factors: Emotional triggers, stress, anxiety, and certain foods or drinks can exacerbate sweating in individuals prone to hyperhidrosis.
Triggers That Cause Sweating
Various factors can also trigger excessive sweating. Some common triggers include:
- Physical Activity: Exercise or strenuous physical activity increases body temperature, prompting sweating.
- Emotional Stress: Anxiety, nervousness, or emotional stress can lead to excessive sweating.
- Hot Weather: High temperatures or humid conditions cause the body to sweat for cooling.
- Spicy Foods: Consuming spicy foods may stimulate sweat glands.
- Illness: Fever or certain medical conditions can induce sweating.
Understanding these triggers helps manage normal sweating. However, if sweating is excessive and persistent, it may indicate a medical condition like hyperhidrosis.
Medications That Cause Sweating
Some medications can also lead to a medical condition of excessive sweating.
- Antidepressants: Medications like Prozac and Celexa may cause excessive sweating.
- ADHD Stimulants: Some drugs used for Attention Deficit Hyperactivity Disorder (ADHD) can lead to increased perspiration.
- Dementia and Parkinson's Drugs: Medications treating these conditions, like donepezil or benztropine, may induce sweating.
It is essential to be aware of potential side effects of medicine dosage, and if excessive sweating occurs, it is ideal to consult with a healthcare professional.
Medical Conditions That Cause Sweating
Underlying medical conditions may further contribute to hyperhidrosis. Examples include:
- Hyperthyroidism: Overactive thyroid gland.
- Diabetes: Especially if blood sugar levels are not well-controlled.
- Menopause: Hormonal changes in women during menopause can result in increased sweating.
Does Hyperhidrosis Run in Families?
Yes, hyperhidrosis can have a genetic component, and it often runs in families. Primary focal hyperhidrosis, a chronic skin condition characterised by excessive sweating, is linked to genetic changes (mutations) that can be inherited.
What are the Complications of Hyperhidrosis?
Hyperhidrosis, while generally not medically serious, can lead to several complications:
- Skin Infections: Excessive sweating may create a favourable environment for bacterial and viral infections, such as warts and bacterial skin infections.
- Social and Emotional Impact: The condition may cause social discomfort, embarrassment, and emotional distress, impacting an individual's quality of life.
- Skin Breakdown: Prolonged moisture on the skin can lead to maceration, increasing the risk of skin breakdown.
- Odour Issues: Persistent sweating may contribute to body odour, affecting personal hygiene and social interactions.
- Practical Challenges: Excessive sweating may interfere with daily activities, causing discomfort and inconvenience.
How is Hyperhidrosis Diagnosed?
Hyperhidrosis is typically diagnosed based on a thorough medical history, physical examination and evaluation of hyperhidrosis symptoms. The healthcare provider may ask questions about the pattern of sweating, triggers and the impact on daily life. Additionally, the following steps may be involved in the diagnosis:
- Sweat Test: A starch-iodine test may be conducted to visualise areas of excessive sweating. Iodine is applied to the skin, and starch is sprinkled over it. The starch turns dark blue in regions with excessive sweat.
- Blood and Urine Tests: Blood and urine tests may be performed to rule out underlying medical conditions that may cause excessive sweating.
- Skin Conductance Test: This measures the electrical conductance of the skin, helping to assess the amount of sweat produced.
What Tests Diagnose Hyperhidrosis?
Diagnosing hyperhidrosis involves a combination of medical history, physical examination, and specific tests:
- Medical History: The doctor will inquire about sweating patterns, triggers, and family history to understand the nature of excessive sweating.
- Physical Examination: A thorough examination of the affected areas, such as palms, soles, and armpits, helps assess the extent of sweating.
- Starch-Iodine Test: This test involves applying iodine solution mixed with starch to highlight areas of excessive sweating.
- Paper Test: Specialised paper is used to absorb and quantify sweat production, aiding diagnosis.
- Thermoregulatory Sweat Test: This assesses the ability to sweat in response to temperature changes, helping identify the underlying cause.
How is Hyperhidrosis Treated?
Hyperhidrosis, or excessive sweating, can be addressed through various approaches. Antiperspirants and topical anticholinergic medications applied with medicated wipes can help manage sweating at home. Medications, such as prescription antiperspirants containing aluminium or botulinum toxin injections, provide additional relief. Excessive sweating treatment therapies like iontophoresis, using a low electrical current and laser therapy targeting sweat glands, offer effective alternatives.
At-Home Hyperhidrosis Treatment
Managing hyperhidrosis at home involves several self-care measures to alleviate symptoms. Some of these treatments include:
- Choose Breathable Fabrics: Opt for loose, breathable clothing to minimise moisture and promote air circulation.
- Maintain Good Hygiene: Regular showers and keeping affected areas dry help prevent bacterial growth.
- Stay Cool: Avoid triggers like hot environments and manage stress to reduce excessive sweating.
- Foot Care: For plantar hyperhidrosis, use moisture-wicking socks and rotate shoes to keep feet dry.
While these strategies offer relief, severe cases may require medical intervention, so consulting a doctor is advisable.
Hyperhidrosis Medications
Medications prescribed by a doctor may include:
- Topical Medications: Creams or solutions containing ingredients like glycopyrrolate can reduce sweat production.
- Oral Medications: Prescription medications like anticholinergics may be prescribed to decrease sweating.
- Antidepressants: Some antidepressants, like Selective Serotonin Reuptake Inhibitors (SSRIs), may help manage hyperhidrosis.
Hyperhidrosis Treatment Therapies
Hyperhidrosis, or excessive sweating, can be managed with various treatment therapies. These include:
- Botox Injections: Botulinum toxin injections temporarily block nerve signals that activate sweat glands. This popular treatment effectively reduces excessive sweating by inhibiting gland activity.
- Prescription Medications: Anticholinergic drugs, taken orally, are prescribed to diminish sweat production. By targeting the nervous system, these medications help control hyperhidrosis symptoms.
- Iontophoresis: A non-invasive therapy involving a device that delivers a mild electrical current to affected areas. This disrupts sweat gland function, leading to a reduction in sweating.
- Surgical Options (Sympathectomy): In severe cases, sympathectomy is considered. This surgical procedure involves disrupting nerve signals that contribute to excessive sweating.
- Laser Therapy: Laser treatment offers a minimally invasive solution. Laser energy targets and destroys sweat glands, providing a safe and effective option for managing hyperhidrosis.
These excessive sweating treatment options are tailored based on the severity and impact of hyperhidrosis on an individual's daily life.
Hyperhidrosis Surgery
Hyperhidrosis surgery, reserved for severe cases unresponsive to other treatments, involves specific procedures:
- Sympathectomy: A surgical intervention where sympathetic nerves that trigger sweat glands are either cut or clamped.
- Laser Sweat Ablation: Utilises laser technology to selectively target and destroy sweat glands.
- Sweat Gland Removal: Surgical excision or liposuction to remove sweat glands in the affected areas.
While surgery can provide long-term relief, it carries risks, including compensatory sweating in other areas. Therefore, it is crucial to thoroughly discuss potential outcomes and complications with a doctor before opting for surgical intervention.
Are There Side Effects of the Treatment?
Yes, hyperhidrosis treatments may have side effects. Common side effects include:
- Skin Irritation: Some treatments, like antiperspirants and deodorants, may cause skin irritation, cracking, or blisters.
- Compensatory Sweating: Surgical interventions or Botox injections can lead to compensatory sweating in other body areas.
- Nausea and Headaches: Botulinum toxin injections may cause nausea, headaches, and hot flashes.
Hence, discussing potential side effects with a healthcare professional before undergoing any hyperhidrosis treatment is essential.
How Soon After Treatment Will I Feel Better?
The timeframe for improvement after hyperhidrosis treatment varies. Some individuals may experience immediate relief, while others might notice changes over a few weeks to months. The effectiveness and speed of improvement depend on the chosen treatment method and the individual's response.
Can Hyperhidrosis be Prevented?
While hyperhidrosis may not be entirely preventable, certain lifestyle adjustments can help manage hyperhidrosis symptoms. Using aluminium-based antiperspirants, showering more frequently and changing daily routines, such as choosing breathable clothing, can contribute to symptom control. However, consulting a healthcare professional for personalised advice on managing and preventing hyperhidrosis is crucial.
What Can I Expect if I Have Hyperhidrosis?
If you have hyperhidrosis, you can expect the following:
- Excessive Sweating: Hyperhidrosis is characterised by intense and uncontrolled sweating, often exceeding normal thermoregulatory needs.
- Impact on Quality of Life: The condition may significantly affect your quality of life, causing discomfort and emotional distress.
- Chronic Symptoms: Hyperhidrosis is a chronic disorder, and symptoms persist over time.
- Specific Area Affection: Sweating often occurs in particular areas like palms, soles, axilla, or face.
- Potential Triggers: Identifying and managing triggers like stress or spicy foods may help alleviate symptoms.
Is There a Cure For Hyperhidrosis?
While there is no definitive cure for hyperhidrosis, various treatment options can effectively manage hyperhidrosis symptoms. These may include topical treatments, medications, therapies and, in severe cases, surgical interventions. While these approaches can provide relief, they may not offer a permanent solution. Consultation with a professional can help determine the most suitable approach based on the severity and impact of your condition.
When Should I See a Healthcare Provider?
If you are experiencing excessive sweating that significantly impacts your daily life, it is advisable to seek consultation with a healthcare provider. They can help diagnose the underlying cause and recommend appropriate treatment options. Additionally, if other hyperhidrosis symptoms accompany sweating, consulting a healthcare professional is crucial for personalised guidance and effective management of hyperhidrosis.
What Questions Should I Ask My Doctor?
When discussing hyperhidrosis with your doctor, consider asking about the potential causes, available treatment options and expected outcomes. Clarify any concerns about side effects, treatment duration, and whether lifestyle modifications could complement medical interventions. Open communication with your doctor ensures a comprehensive understanding of your condition and an informed decision-making process.
Why Does Sweat Smell Bad?
When sweat interacts with bacteria on the skin's surface, it can lead to an unpleasant odour.
Sweat itself is primarily odourless, but when bacteria break down the proteins in sweat, it produces compounds that result in body odour. This is particularly true for the sweat released by apocrine glands, commonly found in areas with dense hair follicles, such as the armpits and groin. Maintaining good hygiene by regular bathing and using antibacterial soaps helps reduce bacterial activity, minimising body odour.
Additionally, factors like diet, stress, and hormonal changes can influence the composition of sweat, contributing to variations in body odour. The combination of sweat and bacteria on the skin creates the distinctive smell associated with body odour.
Conclusion
Individuals experiencing hyperhidrosis should explore diverse treatment avenues to find what works best for them. Consulting doctors and considering the latest interventions, such as topical antiperspirants, botox injections and surgical options, can provide tailored solutions to manage or alleviate hyperhidrosis. Offering accurate blood testing and health check-up services across India, get yourself tested for hyperhidrosis with Metropolis Labs. Embrace a seamless experience with at-home blood sample collection and online report sharing with Metropolis Labs, your partner in well-being.




























