Preventive Healthcare
Optic Neuritis: What It Is, Signs to Watch & Treatment Paths
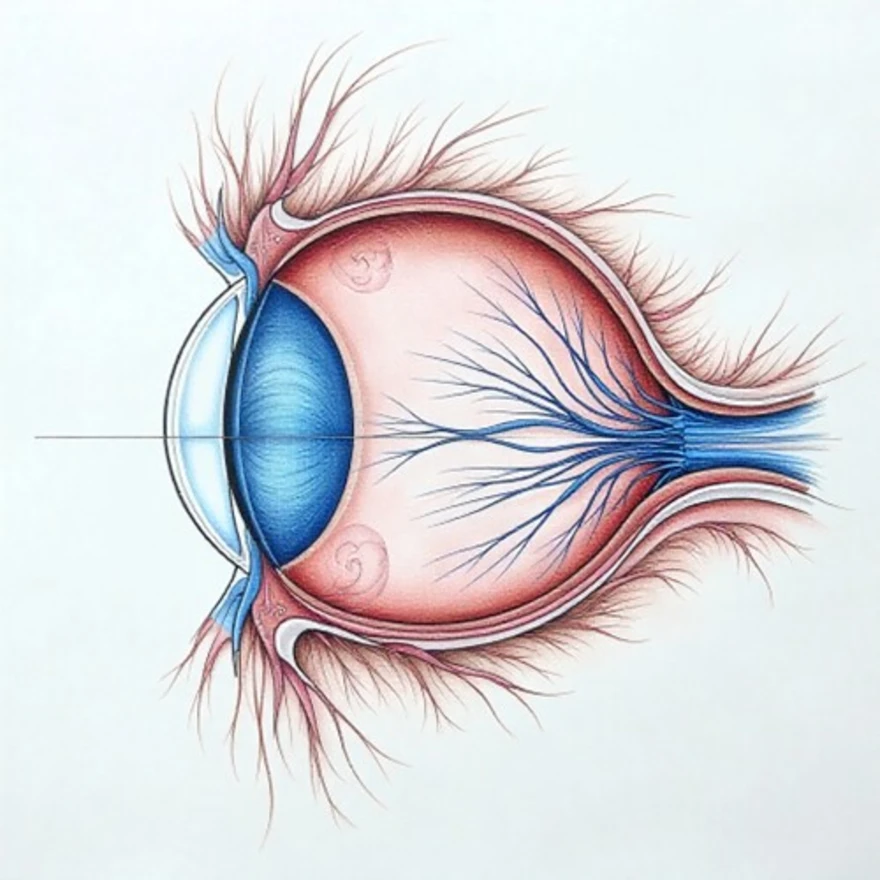
Table of Contents
What is Optic Neuritis?
Optic neuritis is an inflammatory condition affecting the optic nerve—the vital bundle of nerve fibers that transmits visual information from your eye to your brain. Inflammation damages the protective myelin sheath surrounding these nerve fibers, disrupting their ability to transmit clear visual signals.
This condition typically affects one eye, though both eyes can be involved in some cases. The inflammation prevents your optic nerve from functioning properly, leading to sudden vision changes ranging from mild blurring to temporary blindness in the affected eye. According to the American Academy of Ophthalmology, optic neuritis most commonly affects adults between ages 20 and 40, occurring more often in women than in men.
The condition is notable because it can be the first sign of an underlying neurological condition such as multiple sclerosis. The inflammation can develop rapidly, with symptoms typically worsening over hours to days before potentially beginning to improve.
Understanding what triggers optic neuritis is crucial for proper treatment. The condition occurs when your body's immune system mistakenly attacks the myelin sheath protecting your optic nerve fibers. Without this protective coating, nerve signals become scrambled or blocked entirely, resulting in the vision problems characteristic of this condition.
Symptoms of Optic Neuritis
• Sudden vision loss - Ranging from mild blurring to severe vision impairment or, rarely, temporary blindness in one eye
• Eye pain - Particularly sharp, aching pain that worsens when you move your eyes in any direction
• Colour vision changes - Colours appearing washed out, dull, or less vibrant than normal
• Central vision problems - Difficulty seeing objects directly in front of you, creating a dark or blurry spot in your central field of view
• Abnormal pupil reactions - The affected eye's pupil may not respond normally to bright light
• Visual field defects - Missing patches, dark spots, or blind areas in your vision
• Pain behind the eye - Deep, aching discomfort that may persist even when your eyes are closed
The progression of optic neuritis symptoms typically follows a predictable pattern. Vision problems often develop rapidly over 24-48 hours, reaching their worst point within the first week. Pain usually accompanies the vision loss and may be the first symptom you notice, especially when moving your eyes.
Causes and Risk Factors
Understanding the optic neuritis causes helps explain why this condition develops and who might be at higher risk. While the exact cause remains unknown in many cases, researchers have identified several key factors that can trigger this inflammatory condition.
Multiple sclerosis (MS) is the most common underlying condition associated with optic neuritis. Studies show that about 50% of people who experience optic neuritis develop multiple sclerosis within 15 years. This autoimmune disease causes the body's immune system to attack the protective myelin coating around nerve fibers throughout the central nervous system.
Autoimmune conditions beyond multiple sclerosis also increase your risk. Systemic lupus erythematosus (lupus) can trigger optic neuritis when the immune system attacks healthy tissue throughout the body, including the optic nerve. Other autoimmune diseases like neuromyelitis optica spectrum disorder (NMOSD) and sarcoidosis can also cause optic nerve inflammation.
Infectious diseases represent another major category of optic neuritis causes. Viral infections, particularly those affecting the respiratory system, can trigger an inflammatory response that damages the optic nerve. Bacterial infections like syphilis, Lyme disease, and tuberculosis have all been linked to optic neuritis development. Even childhood diseases like measles and other viral infections can occasionally lead to optic nerve inflammation.
Additionally, having a family history of multiple sclerosis or other autoimmune conditions increases your likelihood of developing optic neuritis. Previous viral infections, particularly respiratory illnesses, may also elevate your risk.
Diagnosis of Optic Neuritis
- Detailed medical history - Your doctor will ask about your symptoms, when they started, how quickly they developed, and whether you have any family history of autoimmune diseases or neurological conditions.
- Comprehensive eye examination - This includes checking your visual acuity, colour vision, pupil responses, and examining the optic nerve using specialised instruments.
- Neurological assessment - Your doctor will test your reflexes, coordination, and other neurological functions to look for signs of underlying conditions like multiple sclerosis.
- Visual field testing - This computerised test maps your complete field of vision to identify any blind spots or areas of vision loss.
- Advanced imaging studies - MRI scans of your brain and optic nerves can reveal inflammation and help identify underlying neurological diseases.
Early and accurate optic neuritis diagnosis is crucial because prompt treatment can significantly improve your visual outcomes and help prevent future episodes.
Tests Used to Diagnose Optic Neuritis
• Visual acuity testing - Measures how clearly you can see letters on an eye chart at various distances
• Colour vision assessment - Uses specialised plates or computer tests to evaluate your ability to distinguish different colours
• Pupillary light reflex testing - Checks how your pupils respond to bright light, looking for the characteristic Marcus Gunn pupil sign
• Ophthalmoscopy - Allows direct visualisation of your optic nerve head to assess for swelling or other abnormalities
• Optical coherence tomography (OCT) - Provides detailed images of your retinal nerve fibre layer to detect thinning or damage
• Visual evoked potential testing - Measures the electrical activity in your brain in response to visual stimuli
• MRI - The most important imaging test, revealing optic nerve inflammation and any brain lesions suggestive of multiple sclerosis
Treatment Options for Optic Neuritis
Effective optic neuritis treatment focuses on reducing inflammation, speeding recovery, and preventing future episodes. Treatment approaches vary depending on the underlying cause and severity of your condition.
Corticosteroids represent the primary optic neuritis treatment for most patients. High-dose intravenous methylprednisolone is typically given for 3–5 days, sometimes followed by a short oral prednisone taper. These anti-inflammatory medications help reduce optic nerve swelling and may speed visual recovery, although they do not necessarily affect the final visual outcome.
When optic neuritis is associated with multiple sclerosis, disease-modifying therapies (DMTs) are essential for preventing future relapses and slowing progression. These medications help prevent future relapses and slow the progression of neurological damage. Options include interferons, glatiramer acetate, and newer oral medications like fingolimod or dimethyl fumarate.
For cases related to other autoimmune conditions like lupus, treatment focuses on managing the underlying disease. This might involve immunosuppressive medications like methotrexate, azathioprine, or mycophenolate mofetil, depending on your specific condition and overall health status.
Infectious causes require targeted antimicrobial therapy. If syphilis is identified as the trigger, appropriate antibiotic treatment can help prevent further nerve damage. Similarly, Lyme disease-related optic neuritis responds to specific antibiotic regimens.
Recovery and Prognosis
• Timeline for improvement - Most people begin noticing visual improvement within 2-4 weeks of starting treatment, with continued recovery over several months
• Extent of recovery - Some people may recover significant vision, though complete restoration isn't always possible
• Residual effects - Some patients experience persistent colour vision problems or subtle visual field defects even after recovery
• Risk of recurrence - Some people experience additional episodes, particularly those with underlying multiple sclerosis
• Long-term monitoring - Regular follow-ups are essential to monitor recovery and detect any signs of associated neurological disease
• Functional impact - Most people return to their normal daily activities, though some may need workplace accommodations or driving restrictions
The speed and completeness of your recovery depend on several factors, including how quickly you received treatment, the severity of initial inflammation, and whether you have an underlying condition like multiple sclerosis.
Can Optic Neuritis Lead to Permanent Vision Loss?
Most individuals with optic neuritis do recover significant vision, though the extent varies considerably between patients. Permanent vision loss can occur, particularly when treatment is delayed or when extensive axonal damage has occurred before inflammation is controlled. Long-term visual outcomes depend on how quickly treatment begins, the severity of inflammation, and whether an underlying condition like multiple sclerosis is present.
Even when some permanent changes occur, they're often subtle and don't significantly impact daily activities. Many people notice slight changes in colour perception or contrast sensitivity that don't interfere with driving, reading, or work-related tasks.
What to Do If You Experience Vision Loss or Eye Pain?
• Seek immediate medical attention - Contact your eye doctor or visit an emergency department if you experience sudden vision loss combined with eye pain
• Don't wait to see if symptoms improve - Early treatment within the first few days of symptom onset offers the best chance for full recovery
• Prepare for your appointment - Write down when symptoms started, how they've progressed, and any recent illnesses or medications you've taken
• Bring a companion - Vision problems can make navigating medical appointments challenging, and having support helps ensure you don't miss important information
• Ask about underlying conditions - If diagnosed with optic neuritis, discuss your risk for multiple sclerosis and other autoimmune diseases
• Follow treatment recommendations - Take prescribed medications as directed and attend all follow-up appointments, even if your vision improves
Conclusion
Optic neuritis represents a serious but treatable condition that demands immediate medical attention when symptoms first appear. Understanding the warning signs: sudden vision loss, eye pain with movement, and colour vision changes, empowers you to seek timely care that can preserve your sight and identify underlying conditions like multiple sclerosis, lupus, or infectious diseases such as syphilis, Lyme disease, or measles complications.
The journey from symptom onset through optic neuritis diagnosis and treatment requires patience and persistence, but the prognosis is generally encouraging. With proper optic neuritis treatment, including corticosteroids and management of underlying conditions, most people recover substantial vision within months. Advanced optic neuritis radiology and comprehensive testing help ensure accurate diagnosis and appropriate treatment planning.
At Metropolis Healthcare, we support your journey towards better health with comprehensive diagnostic services designed around your needs. Our extensive portfolio of over 4,000 tests includes specialised neurological and autoimmune and neurological panels that help identify underlying causes of optic neuritis. Through our network of more than 220 laboratories and 4,600 service centres, we provide convenient access to accurate testing that guides effective treatment decisions.
For comprehensive health monitoring and peace of mind, explore our diagnostic services today. Your vision and neurological health deserve the precision and care that advanced testing provides.
FAQs
Can Optic Neuritis Be Prevented?
While you cannot completely prevent optic neuritis, maintaining good overall health, managing autoimmune conditions properly, and seeking prompt treatment for infections may reduce your risk of developing this inflammatory condition.
Is Optic Neuritis Related to Multiple Sclerosis?
Yes, optic neuritis is strongly associated with multiple sclerosis. Approximately 15-20% of people with multiple sclerosis first present with optic neuritis, and those with optic neuritis have increased risk for developing multiple sclerosis.
How Long Does Recovery Take From Optic Neuritis?
• Most people begin experiencing visual improvement within 2-4 weeks of starting treatment
• Significant recovery typically occurs over 3-6 months
• Complete recovery may take up to one year in some cases
What Is the Role of Steroids in Treating Optic Neuritis?
Corticosteroids like methylprednisolone reduce optic nerve inflammation and may speed visual recovery. While they don't necessarily improve final visual outcomes, they can help restore vision more quickly and reduce symptom severity.
References
- https://my.clevelandclinic.org/health/diseases/14256-optic-neuritis
- https://eyewiki.org/Diagnostic_Approach_to_Atypical_Optic_Neuritis
- https://www.ncbi.nlm.nih.gov/books/NBK557853/
- https://medlineplus.gov/ency/article/000741.htm
- https://jamanetwork.com/journals/jamaneurology/fullarticle/795756