Preventive Healthcare
Hyperaldosteronism: Causes, Symptoms, Diagnosis & Treatment
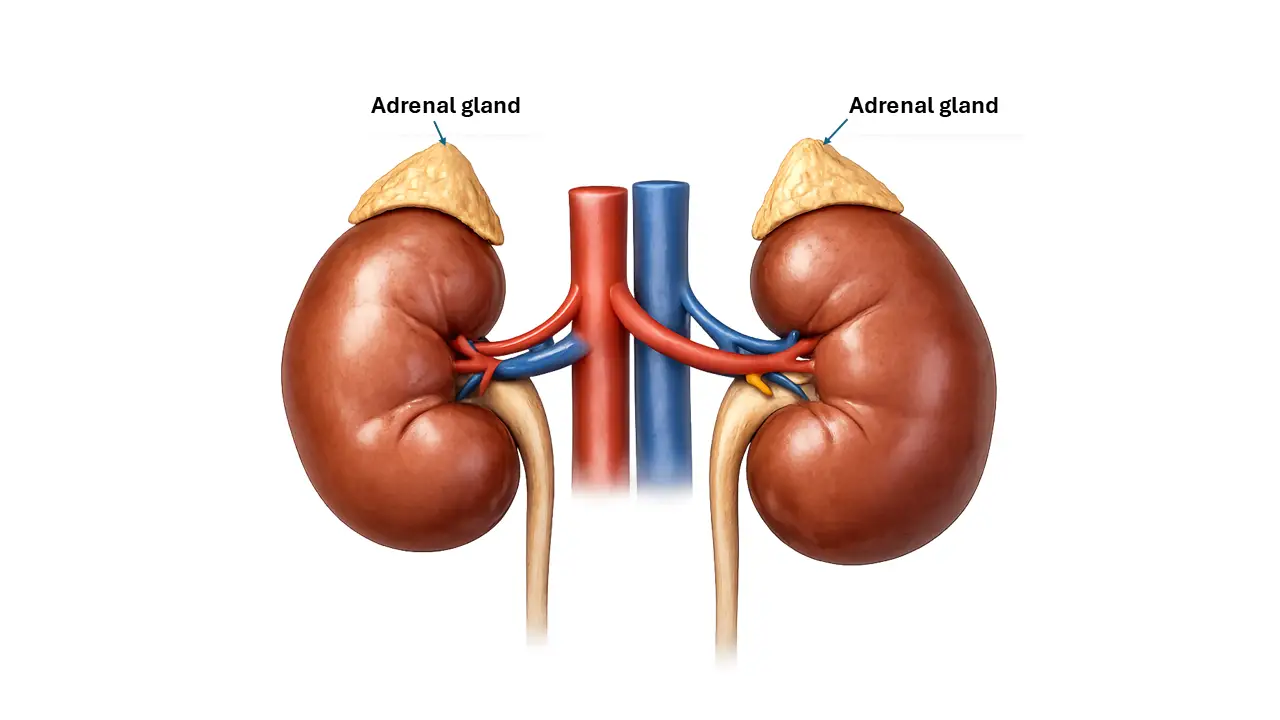
Table of Contents
- What Is Hyperaldosteronism?
- Types of Hyperaldosteronism
- Who Is at Risk of Hyperaldosteronism?
- Symptoms of Hyperaldosteronism
- Why Hyperaldosteronism Causes High Blood Pressure
- How Common Is Hyperaldosteronism?
- How Is Hyperaldosteronism Diagnosed?
- Primary vs Secondary Hyperaldosteronism – Key Differences
- Treatment Options for Hyperaldosteronism
- Prognosis and Long-Term Outlook
- Complications of Untreated Hyperaldosteronism
- Can Hyperaldosteronism Be Prevented?
- Living With Hyperaldosteronism
- Hyperaldosteronism FAQs
- Key Takeaways
What Is Hyperaldosteronism?
Hyperaldosteronism is a condition where the adrenal glands produce too much aldosterone, leading to high blood pressure (often difficult to control) and low potassium levels (hypokalaemia). This hormonal imbalance causes the body to retain excess sodium and water while losing potassium, which can result in symptoms such as fatigue, muscle weakness, frequent urination, headaches, and, over time, heart and kidney complications.
The problem with hyperaldosteronism is that it often looks like “regular” high blood pressure. Many people are treated for years without knowing there’s a hormonal cause behind it. Because of this, the condition is frequently missed or diagnosed late, especially when potassium levels appear normal.
Types of Hyperaldosteronism
Hyperaldosteronism is broadly divided into primary and secondary types, depending on where the problem starts.
Primary Hyperaldosteronism (Conn’s Syndrome)
Primary hyperaldosteronism occurs when the adrenal glands themselves are overproducing aldosterone.
The most common causes include:
Aldosterone-producing adrenal adenoma
This is a benign (non-cancerous) tumour in one adrenal gland that releases excess aldosterone.
Bilateral adrenal hyperplasia
In this condition, both adrenal glands are enlarged and overactive, producing too much aldosterone.
Familial (genetic) hyperaldosteronism
Rare inherited forms of the condition, where abnormal aldosterone production runs in families.
Secondary Hyperaldosteronism
Secondary hyperaldosteronism happens when something outside the adrenal glands triggers excess aldosterone release.
Common causes include:
- Kidney-related conditions that reduce blood flow to the kidneys
- Heart failure and other conditions that cause fluid retention
- Liver disease, especially cirrhosis
- Renal artery narrowing, which affects kidney blood supply
In these cases, the adrenal glands are responding to signals from the body rather than malfunctioning on their own.
Who Is at Risk of Hyperaldosteronism?
Certain groups of people are more likely to have hyperaldosteronism, even if they don’t realise it.
You may be at higher risk if you have:
- High blood pressure that is difficult to control, even with multiple medications
- High blood pressure at a young age, especially before 40
- A family history of hypertension or adrenal disorders
- Adrenal nodules found accidentally during scans done for other reasons
- Associated conditions such as sleep apnoea or atrial fibrillation
Symptoms of Hyperaldosteronism
Symptoms can vary widely. Some people have clear signs, while others feel fine for years.
Common Symptoms
- High blood pressure that doesn’t respond well to standard treatment
- Frequent headaches
- Fatigue or low energy
- Dizziness or light-headedness
Symptoms Due to Low Potassium (Hypokalaemia)
- Muscle weakness or cramps
- Tingling or numbness in the limbs
- Irregular heartbeats
- Temporary paralysis in severe cases
Urinary and Fluid-Related Symptoms
- Frequent urination, especially at night
- Excessive thirst
- Feeling dehydrated despite drinking fluids
Can You Have Hyperaldosteronism Without Symptoms?
Yes. Many people have no obvious symptoms, especially in the early stages. This is one of the main reasons hyperaldosteronism often goes undiagnosed.
Why Hyperaldosteronism Causes High Blood Pressure
Aldosterone controls how much sodium your kidneys retain. When aldosterone levels are too high:
- Sodium and water are retained in the body
- Blood volume increases
- Blood vessels are placed under constant pressure
Over time, this persistent strain damages blood vessels and the heart, increasing the risk of serious cardiovascular problems.
How Common Is Hyperaldosteronism?
Hyperaldosteronism is more common than once believed.
- It affects a significant proportion of people with high blood pressure
- Among those with resistant hypertension, rates are much higher
- Many cases remain undiagnosed because potassium levels can appear normal
In short, hyperaldosteronism is under-recognised, not rare.
How Is Hyperaldosteronism Diagnosed?
When Doctors Suspect Hyperaldosteronism
Doctors may investigate hyperaldosteronism when they see:
- Blood pressure that remains high despite treatment
- Low potassium levels
- High blood pressure starting early in life
Blood Tests
Diagnosis usually begins with blood tests that measure:
- Aldosterone levels
- Renin levels
- The aldosterone-to-renin ratio, which helps distinguish primary from secondary causes
Confirmatory Tests
If screening tests suggest hyperaldosteronism, additional tests may be done to confirm the diagnosis, such as salt-loading or suppression tests.
Imaging Tests
A CT scan of the adrenal glands may be used to look for tumours or gland enlargement.
Adrenal Vein Sampling (When Needed)
In some cases, a specialised test called adrenal vein sampling is used to determine whether one or both adrenal glands are responsible.
Primary vs Secondary Hyperaldosteronism – Key Differences
Hormone patterns:
Primary forms usually show high aldosterone with low renin, while secondary forms have elevated renin levels.
Typical causes:
Primary forms originate in the adrenal glands; secondary forms are driven by kidney, heart, or liver conditions.
Treatment approach:
Primary disease may be treated surgically or medically, while secondary disease focuses on managing the underlying cause.
Treatment Options for Hyperaldosteronism
Surgical Treatment
If only one adrenal gland is affected, surgical removal (adrenalectomy) may cure or significantly improve the condition.
Medical Treatment
For bilateral disease or non-surgical candidates, treatment usually involves medications such as:
- Spironolactone or eplerenone, which block the effects of aldosterone
- Potassium-sparing medications to help maintain normal potassium levels
Treating Secondary Hyperaldosteronism
Treatment focuses on managing the underlying heart, kidney, or liver condition causing the hormonal imbalance.
Lifestyle Measures
- Reducing dietary sodium
- Regular blood pressure monitoring
- Following medical advice consistently
Prognosis and Long-Term Outlook
With early diagnosis and appropriate treatment, outcomes are generally good. Blood pressure and potassium levels often improve, and long-term risks can be reduced.
Surgery may provide lasting benefits in selected cases, while medication is effective for long-term control in others.
Complications of Untreated Hyperaldosteronism
If left untreated, hyperaldosteronism can lead to:
- Heart attack and stroke
- Atrial fibrillation
- Progressive kidney damage
- Increased long-term cardiovascular risk
Can Hyperaldosteronism Be Prevented?
In most cases, hyperaldosteronism cannot be prevented. However, early screening in high-risk individuals can prevent complications and long-term damage.
Living With Hyperaldosteronism
Managing hyperaldosteronism involves:
- Regular follow-up and monitoring
- Adhering to medication and dietary advice
- Seeking medical care if symptoms worsen or blood pressure becomes difficult to control
Urgent medical attention is needed if you experience severe weakness, chest pain, or sudden changes in blood pressure.
Hyperaldosteronism FAQs
What causes hyperaldosteronism?
It is caused by excess aldosterone production, either from the adrenal glands themselves or due to signals from other organs.
Can you have hyperaldosteronism with normal potassium levels?
Yes. Many people have normal potassium levels, especially early on.
Is hyperaldosteronism curable?
Some forms can be cured with surgery. Others are managed effectively with medication.
How long does treatment take to work?
Blood pressure and potassium levels often improve within weeks, though full stabilisation may take longer.
What diet is best for hyperaldosteronism?
A low-sodium diet is usually recommended.
Can hyperaldosteronism come back after surgery?
Recurrence is uncommon but possible, depending on the underlying cause.
Key Takeaways
Hyperaldosteronism is a treatable hormonal cause of high blood pressure that is often overlooked. Recognising the signs early and getting the right tests can significantly reduce long-term health risks and improve quality of life.