Metropolis healthcare
Exploring Hemoglobin: Levels, Erythropoiesis, and Factors
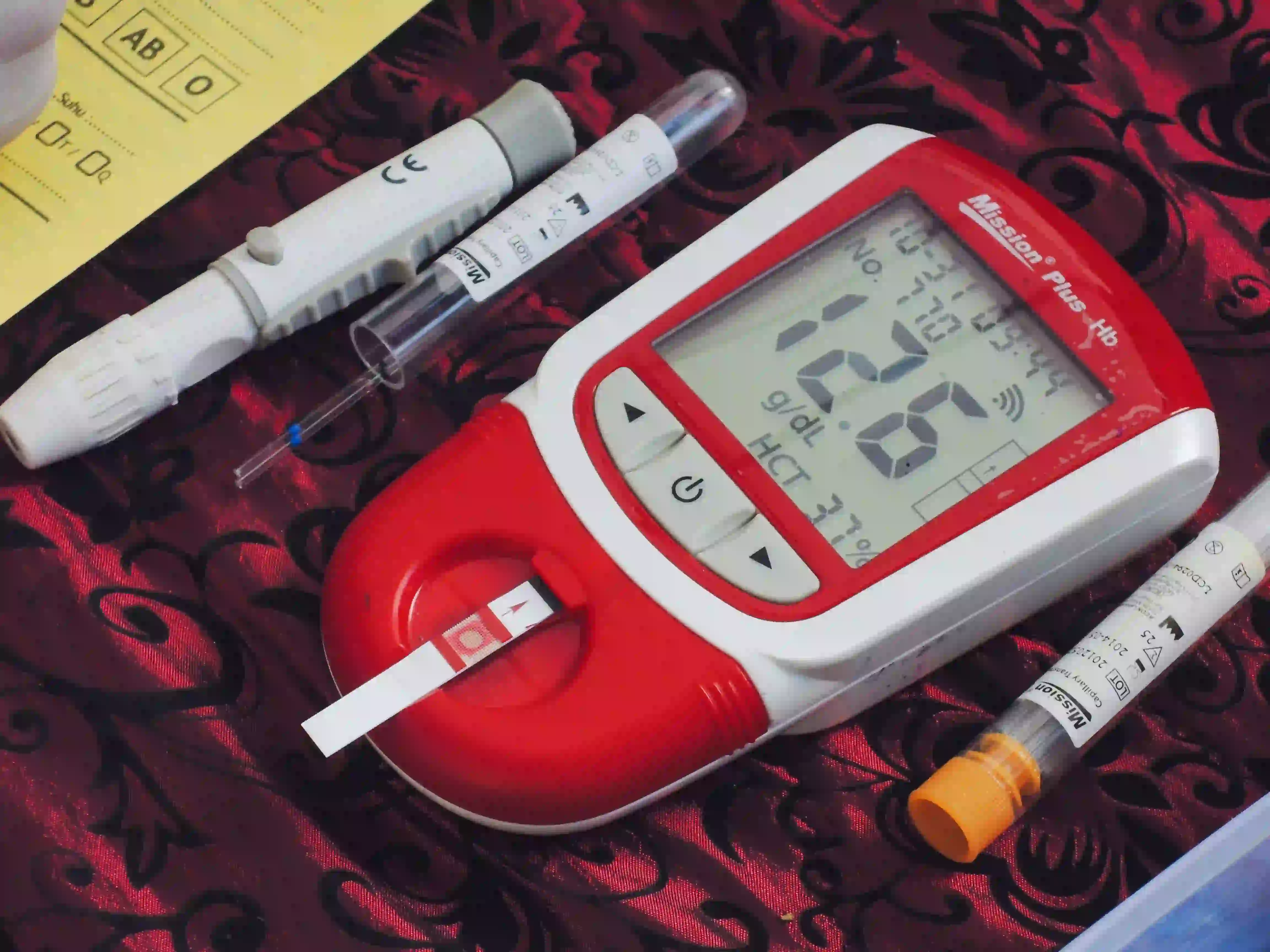
Haemoglobin is a protein molecule found in red blood cells that transports oxygen from the lungs to the body's tissues and returns carbon dioxide to the lungs. Normal haemoglobin levels differ depending on age and gender. It's critical to comprehend the typical range of haemoglobin levels at various life stages to evaluate general health and identify any possible underlying disorders. What is Haemoglobin? Haemoglobin is a protein found in your red blood cells. These red blood cells carry oxygen throughout your body, to different organs through the veins. Because of the iron present in the haemoglobin, the blood gets its bright red colour. Haemoglobin in our body is secreted because of the erythropoiesis hormone to maintain the level of red blood cells in our body. What is the process of erythropoiesis? Our body contains a hormone named erythropoietin (EPO) which increases the level of red blood cells in our body. Our kidneys secrete EPO in the body. The process of erythropoiesis involves the following steps: Our tissues are deficient in oxygen because of the low count of red blood cells. Our kidneys will then secrete EPO to fulfil the deficiency. The EPO will stimulate the bone marrow to produce more red blood cells. Once our kidney finds out the increased level of haemoglobin, it reduces the rate of EPO production. Our body will maintain the correct balance after getting a suitable amount of red blood cells. Our kidneys secrete sufficient amounts of EPO to maintain red blood cell production. Our body loses 1% of red blood cells every day. Erythropoiesis replaces the dead red blood cells in our body. Factors affecting erythropoiesis There are various factors which can affect our body to regulate red blood cells. Lungs disease Asthma Chronic obstructive pulmonary disease (COPD) Cancers that impact your bone marrow or blood Leukaemia Lymphoma Myeloproliferative disorders Myeloma Other factors Deficiency in nutrition like iron, folate or B12. High attitudes. Haemoglobin Levels at Different Stages of Life Haemoglobin levels are higher in infancy due to foetal haemoglobin persisting in the bloodstream. However, as the kid develops, these levels naturally drop, reaching a steady range by early childhood. Hormonal changes and rapid growth spurts throughout adolescence might affect haemoglobin levels, causing transient variations. The haemoglobin range stabilises and remains relatively stable in adults. Haemoglobin levels may drop slightly due to age-related changes and particular health disorders. Understanding the haemoglobin range by age and gender is critical for maintaining good health and detecting potential health problems. Maintaining a person's general health and well-being depends heavily on haemoglobin. It transfers oxygen from the lungs to all the body's tissues and organs. Depending on age and gender, different haemoglobin levels fall within the normal range. Here is an overview: Infancy Haemoglobin levels in infants throughout the first few months of life are typically greater than those in older children and adults. This is mainly because foetal haemoglobin is still present in their blood. For babies, the average haemoglobin varies from 14 to 24 grams per deciliter (g/dL). It is essential for the infant's growth and development and the oxygen supply required for quick bodily processes. Childhood Children's haemoglobin levels progressively decline and stabilise as they enter early childhood and beyond. For kids between the ages of 1 and 9, the average haemoglobin range is generally between 11 and 14 g/dL. These levels guarantee the developing infant gets enough oxygen for their developing body and brain cells. Adolescence Hormonal shifts and quick growth spurts are frequent during adolescence. These variables may affect haemoglobin levels and cause small changes. During this time, it is common to observe a brief rise or fall in haemoglobin levels. Male adolescents' typical haemoglobin levels vary from 12 to 16 g/dL, and female adolescents' average levels are 11 to 15 g/dL. Adulthood As people grow older, their haemoglobin levels usually stabilize and remain constant. The normal range for men is typically 13 to 17 g/dL, whereas the range for women is 12 to 15 g/dL. The lower end of the spectrum for females is caused by physiological variations between the sexes, including monthly blood loss experienced by women. These levels guarantee the body enough oxygen to maintain daily functions, metabolism and general health. Older Adults Haemoglobin levels may modestly fall in older adults, especially for people over 65. This is frequently brought on by the body's ageing process and the existence of particular medical diseases. The typical normal range for seniors is between 11 and 15 g/dL for females and 12 to 16 g/dL for males. You should remember that these ranges could change based on a person's health and medical issues are crucial. The Importance of Monitoring Haemoglobin Levels in Each Life Stage Monitoring haemoglobin levels is essential for regular physical examinations, especially for people exhibiting weariness, breathlessness, or extreme pallor. Low haemoglobin levels indicate anaemia, defined by a shortage of red blood cells or a reduced ability to carry oxygen. On the other hand, elevated haemoglobin levels may indicate dehydration, a few lung conditions, or problems with the bone marrow. To maintain general health and well-being, you must keep your haemoglobin levels at an adequate level. A well-balanced diet full of iron, folic acid and vitamin B12 can encourage the development of healthy haemoglobin. Individuals should also prioritise getting enough sleep, managing their stress levels and engaging in regular physical activity to promote ideal haemoglobin levels. Book Haemoglobin Test Conclusion The typical range of haemoglobin levels is essential for maintaining overall health, as they range from higher levels in infancy to stable levels in adulthood, with possibly slight declines in later age. People can improve their well-being and length of life by detecting and monitoring these values and taking proactive steps to ensure that tissues and organs are adequately oxygenated. Metropolis Healthcare is a trustworthy pathology service provider that can be considered for your next haemoglobin test. They are known to deliver the most accurate test reports within time with the facility of home sample collection if needed.
Malaria: Symptoms, Causes, Treatment and Prevention
Malaria is caused by which mosquito? Female mosquitoes with the Plasmodium parasite spread the infectious illness called malaria. These female mosquitoes bite humans to spread the parasites into the blood flow, which causes symptoms like fever, exhaustion, vomiting, and headaches. Symptoms typically start to show up 8 to 25 days after infection, and while they may first seem moderate, untreated symptoms can worsen and ultimately result in death. It is a common disease in tropical countries. Although it is still the most dangerous mosquito-borne disease, its treatment has significantly improved in recent years. Although there is no vaccine to prevent malaria, the use of indoor residual spraying (IRS), insecticide-treated mosquito nets (ITNs), antimalarial drugs, early diagnosis, and treatment have all helped to reduce the number of new cases and fatalities. Symptoms of Malaria Typically, 10 to 14 days after a mosquito infects you, signs of malaria fever start to show up. The following are signs of malaria fever: Extreme exhaustion Having trouble breathing Nausea and diarrhoea Increased urge to urinate Cough Continent pain Aching joints Dark-coloured or blood-coloured urine Seizures Jaundice How does Malaria Spread? Malaria is caused by the bite of a female anopheles mosquito carrying the illness. Only anopheles mosquitoes may spread Malaria, and they must have previously bitten someone sick to get sick themselves. A small amount of blood carrying microscopic malaria parasites from the infected individual is ingested by the mosquito during the initial bite. When the mosquito bites again about a week later, the parasites combine with its saliva and are passed on to the victim. Malaria is caused by organ transplantation, blood transfusion, and the use of contaminated needles and syringes. In addition, congenital malaria can happen before or during childbirth. Is Malaria an Infectious Disease? Malaria is a contagious disease. The Plasmodium parasite enters the female Anopheles mosquito when it bites a person with malaria. Malaria develops when an infected mosquito bites a healthy person, and the parasite enters the bloodstream. The Plasmodium parasite multiplies quickly in the liver and infects red blood cells within 48 to 72 hours. It weakens the body's immune system gradually. Malaria, in a severe form, could even impede progress in younger children. Diagnosing and Treating Malaria Malaria is diagnosed through blood samples. Under a microscope, the parasites are discernible. Treatment should start immediately after diagnosis. Almost all patients recover completely. It is treated and prevented with the help of antimalarial drugs. Malaria can occasionally prove challenging. The following are some of the problems: Severe anaemia Pregnancy-related malaria Cerebral malaria Renal injury, acidosis, and spleen rupture Failing of several organs, etc. Malaria During Pregnancy Pregnant women experience severe malarial illness frequently, and the mortality rate from severe malaria is close to 50%. This illness is associated with miscarriage, intrauterine death, premature birth, low birth weight, and neonatal death. As part of efforts to prevent and treat malaria, antepartum care (care for healthy pregnancies) is essential because the second trimester appears to have the highest infection rate. Preventive Measures Against Malaria Chemoprophylaxis and insect-bite prevention are now complementary approaches to prevent malaria. Although various malaria vaccines are in development, none are yet on the market. Chemoprophylaxis: In European countries, travellers only need to take a medicine called chemoprophylaxis for malaria if they are going to one of three (or four) categories of countries where the disease is endemic. The selection of medications is influenced by the travel destination, the length of potential vector exposure, the resistance pattern of the parasite, the rate and seasonality of transmission, age, and pregnancy. Depending on the extent of endemicity and the seasonality of transmission, chemoprophylaxis may also be advised for indigenous small children and pregnant women in endemic countries. Personal Strategies for Preventing Mosquito Bites: Malaria is primarily transmitted at night since most anopheles mosquitoes eat at night. The use of mosquito bed nets, preferably insecticide-treated nets, sleeping or resting in screened or air-conditioned rooms, dressing in clothing that covers the majority of the body, and using insect repellent as directed on the product label are all examples of personal protective measures to lower the risk of mosquito bites. Controlling Mosquitoes: The effectiveness of vector control strategies depends on the vector species, the biology of the mosquito, the epidemiological situation, the cost, and the acceptability of the people. The primary measures concentrate on reducing human-mosquito interaction, eliminating larvae through environmental management, and using larvicides or mosquito larvae. Book Malaria Test To Sum Up Malaria is caused by female mosquitoes and can cause severe health issues, and sometimes can be fatal. Talking to your doctor about using drugs to prevent malaria before travelling to or staying briefly in a region where the disease is endemic is advisable. You must take these prescription drugs before, during, and after your visit. Metropolis Healthcare is a renowned pathology lab and diagnostic centre that offers various blood tests like Malaria test to determine malaria transmission. This healthcare centre is preferred by many patients because of: Highly accurate reports Patients can also check reports online within 24 hours Well-equipped labs and highly skilled technicians Patients' reports are kept confidential
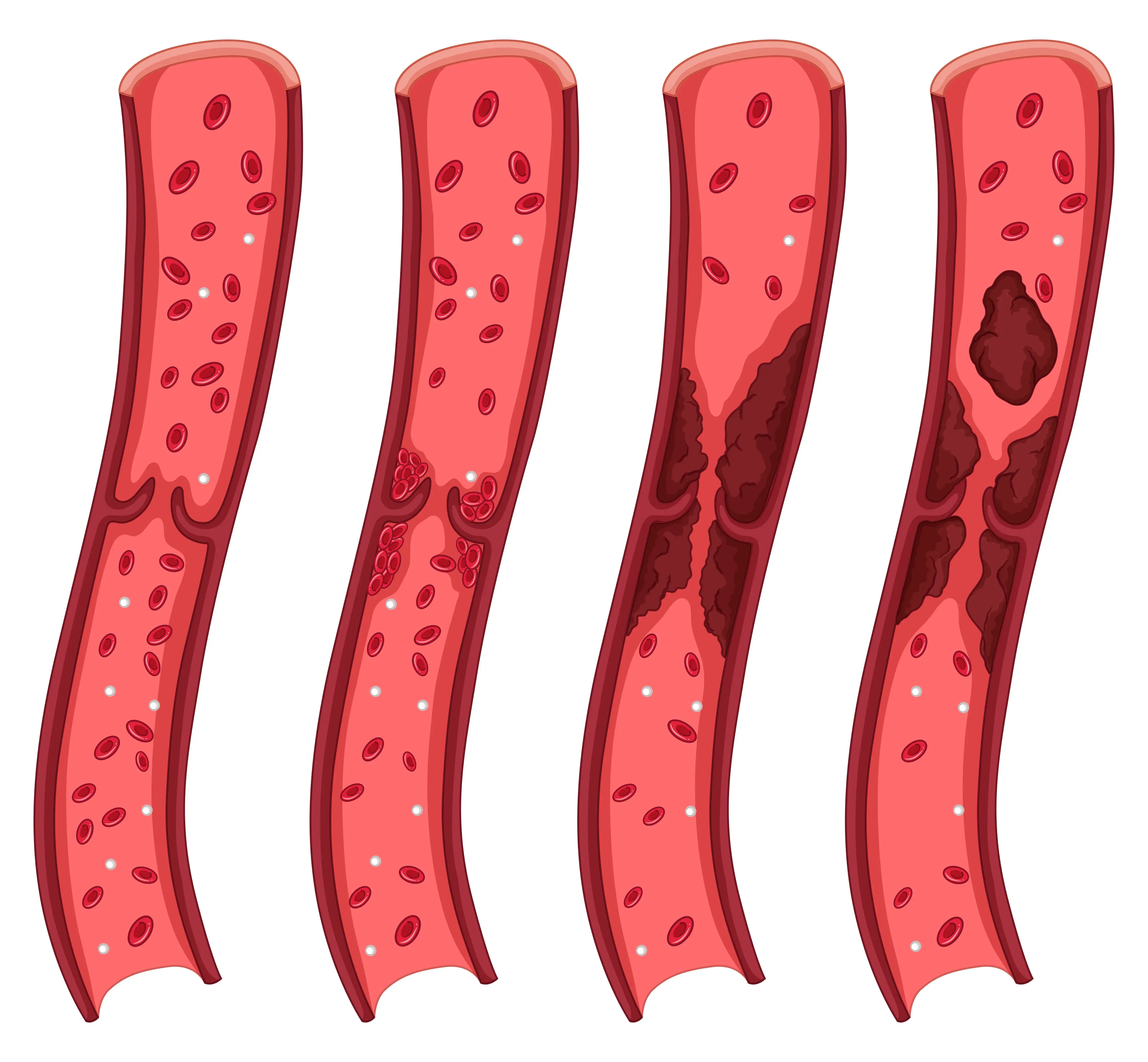
Exploring Thrombus and Thrombosis: Types, Symptoms, and Treatment
Introduction A thrombus is a type of blood clot that develops inside a blood vessel and does not travel to any other site, unlike an embolism. Thrombi (plural for thrombus) lodge itself into a blood vessel and hampers the blood flow through that vessel, blocking the normal blood flow and oxygen from the other tissues. Lack of blood flow results in the destruction of the cells, and cell damage and could also cause cell death or necrosis in that area. The development of a thrombus is referred to as thrombosis. Types of Thrombi A blood clot is usually formed in response to a physical injury. The platelets in the blood quickly clot to form a plug at the injury site and prevent bleeding. However, a thrombus interrupts the normal functioning of the blood vessel. If a section of the thrombus breaks off and travels to other body areas, it causes an embolism. This embolism can lodge itself in different body parts but can be exceptionally dangerous if they reach vital organs like the lungs, heart, or brain. A thrombus is classified on the bases of which blood vessel they develop in Arterial thrombosis: A thrombus formed in the artery, especially in the brain or heart, is known as arterial thrombosis. The arteries carry blood from your heart to the other parts of your body. Arterial thrombosis is one of the leading causes of strokes and heart attacks. Venous thrombosis: A thrombus formed in a vein is called venous thrombosis. The veins carry deoxygenated blood from the body back to the heart. A typical example of this kind of blood clot is when it happens deep inside the vein in a disorder called deep vein thrombosis (DVT) Causes of Thrombus A clot can be caused by a series of chemical reactions in the blood cells called proteins and platelets. When you are healthy, your body can regulate its clotting process according to its needs. However, the probability of developing a thrombus can increase when you are not in the best health. It can be found in individuals who: Use tobacco excessively Are overweight or have obesity Has high cholesterol Is overly stressed Has a sedentary or inactive lifestyle Has cancer Conditions like atrial fibrillation, coronary artery diseases, diabetes and clotting disorders like antiphospholipid syndrome can also cause thrombosis. Diagnosis of thrombosis If your doctor suspects thrombosis, several diagnostic tests can help confirm the condition: Blood tests: Your doctor may recommend a blood test called D Dimer Test to check for the presence of a protein fragment called 'D-dimer.' This fragment is typically present when a blood clot starts to dissolve. Ultrasound scans: This non-invasive imaging technique can show if there are any blood clots in the veins. CT (computed tomography) scanning with intravenous dye: In some cases, your doctor may recommend a CT scan with the use of intravenous dye to check for pulmonary embolism (PE). The dye helps highlight any blockages or abnormalities in the arteries supplying blood to the lungs. Ventilation-perfusion scans: These scans involve using radioactive compounds to visualise parts of the lungs that are not receiving adequate oxygen and blood flow. These diagnostic tests play a crucial role in helping doctors accurately diagnose thrombosis and determine appropriate treatment plans based on their findings. Symptoms of thrombosis The symptoms of thrombosis depend on the location and size of the thrombus as well as the complications that it may cause. Most blockages occur in smaller blood vessels like the brain, lungs, legs, or arms. Here are a few of the symptoms of a thrombus based on its location: Lungs A thrombus in the lungs can cause a pulmonary embolism, the symptoms of which include Sharp pain in the chest and surrounding areas including the neck, jaws, shoulders, arms and back Pain while breathing Breathing trouble when active and sometimes even at rest Neck or brain Thrombi in the brain or neck can cause a stroke or transient ischemic attack. These symptoms include: Slurring or garbled speech Weakness or difficulty in controlling one side of the body A noticeable droop on one side of the face Agitation, confusion, or any unusual changes in behaviour Heart A blockage in the heart results in a heart attack and can display symptoms like Discomfort or severe pain in the chest Dizziness or fainting Trouble breathing Stomach A thrombus in the stomach can cause mesenteric ischemia. Early signs of this include Bloating, vomiting and nausea Diarrhoea can also include blood Fever Severe stomach or abdominal pain, especially after a meal Artery in the leg or arm Pale skin in some areas The skin may feel cool to the touch Tingling or numbness Wounds, sores and blisters Sloughing skin is a result of the skin falling away from the tissue under it Necrosis or tissue death A vein in the legs or arms Skin looks darker or redder in some areas It can cause pain in certain affected areas Fluid buildup resulting in swelling Skin that is warm to the touch Treatment for thrombus The treatment of thrombus includes medication, surgeries and minimally invasive procedures. These can include: Blood thinners keep your blood from clotting easily; while they cannot get rid of an existing clot, they can prevent it from growing. Thrombolytic treatments use medication to dissolve any blood clots. However, these are primarily used in emergencies as they can accommodate a thrombus in critical areas like the heart or brain. Thrombectomy is a direct way of removing a clot. The surgeon may opt for a minimally invasive technique or open surgery. In case of complications arise due to thrombosis, you may have to undergo additional treatment as and when needed. How to take care of yourself if you have a thrombus? There are certain things you can do if you already have been diagnosed with a thrombus: Ensure you take your medications regularly. Meet your doctor often. Make lifestyle changes needed to fix the root cause of the clot. Connect with others in similar conditions. Book D Dimer Test Conclusion Thrombosis is a condition that is unpredictable and can quickly become life-threatening. One needs to do everything in their control to prevent a thrombus from developing, but if already developed, it is essential to ensure the situation doesn't deteriorate. Have a line of open communication with your doctor and ask them anything you may want to know about this condition. Regular health checkups and blood tests can help you identify early signs of the disorder and help you take preventive actions whenever possible. Metropolis Labs helps its customers with at-home sample collection and accurate results so you can get your necessary blood and body fluid tests down without disrupting your routine. Read more about the various tests offered at their website.
Understanding Blood Tests: Types, Names, and Their Significance
Introduction Blood testing is the lab analysis of the blood found in your body. Blood testing is usually prescribed if you need to keep track of the progress of a specific treatment, manage health conditions such as high cholesterol, diabetes, illness, or routine checkup. Blood testing is widespread and is usually done by the doctor themselves or at your local diagnostic centre. Knowing the different blood test names and meanings can help you better understand their uses and benefits. Why do blood tests matter? A blood test is carried out for a wide variety of reasons: To find out how well vital organs such as your heart, liver, kidneys, or thyroid are working To help diagnose lifestyle diseases like diabetes, cancer, coronary heart disease, or AIDS/HIV To understand whether the prescribed medicine is working To diagnose clotting or bleeding disorders To identify health issues at an early stage To monitor chronic diseases and health conditions The blood test reports help your doctor get a basic idea of your overall health and prescribe specialised tests to get an accurate diagnosis. Types of blood tests The list of blood tests can be very long. Here are some of the common ones that you need to know about. Complete blood count (CBC) This routine blood test checks ten different components of the blood, including red blood cells, white blood cells, platelets, haemoglobin, and hematocrit. Any abnormalities in the normal levels of these components can indicate nutritional deficiencies, anaemia, blood cancer, infections, problems with the immune system, or clotting problems. You may have to undergo a few follow-up tests to get a more precise diagnosis of your issues. Basic metabolic panel (BMP) This test checks for the following eight components in the blood: Glucose Calcium Sodium Potassium Bicarbonate Chloride Blood urea nitrogen Creatinine You may be asked to avoid eating anything for at least 8 hours before the sample is taken, depending on the parameters you need to measure and the doctor's instructions. Abnormal results in this test may be a result of diabetes, kidney disease, or hormone imbalance. Comprehensive metabolic panel (CMP) In this test, all the parameters checked in the BMP are measured along with a few others, like total protein, albumin, alkaline phosphatase, alanine aminotransferase, aspartate amino transferase, and bilirubin. Abnormalities in these tests can indicate many health issues depending on whether the levels of components are higher or lower than the normal range. Lipid panel Lipid test is used to check the levels of two types of cholesterol in the body: High-density lipoprotein (HDL): It is also known as good cholesterol because it helps the liver remove harmful toxins from the body by breaking them down into waste. Low-density lipoprotein (LDL): It is also called bad cholesterol as it can cause plaque which clogs the blood vessels and increase the risks of heart disease. Thyroid panel The thyroid panel blood test, or the thyroid function test, is used to identify how well your thyroid functions when reacting to or producing hormones like Thyroxine, Triiodothyronine, and Thyroid-stimulating hormone. Abnormal levels of hormones in the body can indicate conditions such as thyroid growth disorders, low protein levels, and abnormal levels of estrogen or testosterone. Cardiac biomarkers An enzyme is a protein which helps the body carry out chemical processes like breaking down food or clotting blood. Some of the standard blood tests for enzymes include Creatine kinase Troponin Creatine kinase-MB Abnormal levels of enzymes indicate a wide range of issues that may need further testing. Sexually transmitted infection (STI) tests Most STIs are diagnosed with the help of a blood test or a blood and urine test combined. Some of the common STIs that can be identified using a blood test are Gonorrhea herpes HIV syphilis chlamydia In some cases, blood tests have their limitations. For example, a test for HIV will be able to detect the virus only after a month of the infection. Coagulation panel A coagulation test is used to measure how long it takes for your blood to clot as well as how effectively it clots. Clotting is important for wound healing; however, if a clot forms in an artery or vein, it can block the blood flow to vital organs and cause health issues. The results of these tests help doctors diagnose haemophilia (the condition in which you bleed excessively), liver conditions, Vitamin K deficiency, leukaemia, and thrombosis. Electrolyte panel This blood test helps measure the levels of different minerals in your body. Any imbalance in these levels may indicate problems with vital organs like the kidneys, lungs, or heart. Along with all the parameters in the BMP and CMP, this test also checks the magnesium and anion gap levels. Allergy testing An allergy blood test can identify increased levels of immunoglobulin E (IgE). It can help detect allergies for such as pollen, pets, various food items, and other substances. Autoimmune diseases An autoimmune disease is a result of your immune system accidentally attacking your body instead of protecting it from parasites, cancer, and viruses. Autoimmune tests include the following: C-reactive protein tests peripheral blood smears erythrocyte sedimentation rate CE complement blood tests antinuclear antibody tests After preliminary testing, blood tests can also be used to identify specialised issues such as cancer, heart disease, and endocrine system disorders. Book CBC Test Conclusion A blood test can give you an overall idea of your health. It can be used to identify diseases or illnesses at an early stage. It also helps your healthcare provider understand how well your body is responding to treatment. Most people get routine blood tests at least once a year to stay on top of their health. You can talk to your doctor about some routine tests to ensure you are in optimal health or opt for medical testing packages available at Metropolis Labs. Metropolis Labs offers all the tests you need based on your age, health and lifestyle.
Exploring Hemoglobin: Normal Range, Levels, Low Hemoglobin and More
Your body needs oxygen to function, and anyone with insufficient blood cells or red blood cells that do not function properly risks their body not getting enough oxygen supply. Without sufficient oxygen, the different parts of the body will not function properly, resulting in numerous health issues. Haemoglobin is a protein usually found in the red blood cells; they are iron-rich and allow the flow of oxygen to the body's other tissues through the blood. Although low levels of haemoglobin are a sure indicator of anaemia, higher than normal haemoglobin range indicates severe health conditions. Understanding haemoglobin range and what it means for your health is essential for anyone who wants to live a healthy lifestyle. What Is Haemoglobin? Haemoglobin is the protein present in the red blood cells responsible for transporting oxygen to the rest of the body. Each haemoglobin protein has four atoms of iron, meaning it can carry four oxygen molecules simultaneously. The haemoglobin then attaches itself to the red blood cells and delivers oxygen wherever the blood flows. As all the billions of cells in your body need oxygen to maintain and repair themselves, haemoglobin plays a significant role in maintaining your health. Haemoglobin is also why your red blood cells get a disc-like shape. This shape enables them to move swiftly within the blood vessels. How Is Your Haemoglobin Range Tested? A simple blood test, also called a haemoglobin test, assesses your haemoglobin levels. The lab technician will take your blood sample and then send it to the testing centre. It is part of the complete blood count (CBC) test. This is a reasonably risk-free test, although you may feel mild pain from the needle entry and slightly bruising near the spot. Dizziness is a rare side effect of the test, but it usually disappears quickly. Why Is a Haemoglobin Test Done? Although a haemoglobin test can be recommended for multiple reasons, they usually amount to one of these three reasons. To Diagnose a Condition This is one of the obvious uses of a haemoglobin test. It is usually prescribed if you experience fatigue, dizziness, shortness of breath or weakness. Most of these symptoms indicate conditions like anaemia, polycythemia or other conditions. Checking Your Overall Health Haemoglobin tests are part of the routine blood analysis you may carry out yearly. It comes under the complete blood count test and is primarily done to monitor your overall health and screen for emerging conditions like anaemia. To Keep Track of a Medical Condition Suppose you have an underlying medical condition such as polycythemia vera or anaemia. In that case, your doctor may suggest regular haemoglobin tests to monitor your condition and alter your treatment if needed. Normal Haemoglobin Range Your haemoglobin range depends on factors such as your age and gender. Here is what normal haemoglobin ranges look like. Infants: 11-18 Young children: 11.5-16.5 Adult male: 13-16.5 Adult females (not pregnant): 12-16 Adult female (pregnant): 11-16 Interpreting Your Results High Haemoglobin Range High haemoglobin levels may signify a rare blood disorder known as polycythemia. In this disorder, your body produces excess red blood cells, which makes your blood thicker than usual. Due to this, you are at a higher risk of developing clots, strokes and heart attacks. It is a serious lifelong condition, which may be fatal without correct treatment. Other causes of your results being near the higher haemoglobin range could be dehydration, living at higher altitudes and smoking. It could also indicate other severe conditions such as heart or lung diseases. Low Haemoglobin Range Lower levels of haemoglobin indicate that you may have anaemia. Anaemia is of different types, including the following: Iron-deficiency anaemia: This is one of the most common types of anaemia and usually occurs when you do not have enough iron in your body and cannot make the haemoglobin you need. Although it usually happens because your body may not absorb enough iron, it also can happen in cases of excessive blood loss. Pregnancy-related anaemia occurs as pregnancy and childbirth require significantly higher amounts of iron. Vitamin-deficiency anaemia: This kind of anaemia results from low nutrient levels such as folic acid or vitamin B12. Aplastic anaemia: In this disorder, your immune system destroys the blood-forming stem cells in the bone marrow, resulting in fewer red blood cells. Hemolytic anaemia: This type of anaemia can have a genetic origin or result from another condition. It is caused due to the breakup of red blood cells in the spleen or bloodstream. Sickle cell anaemia: Another genetic condition that occurs because of the abnormal haemoglobin protein that causes the blood cells to have a sickle shape stopping them from flowing through the smaller blood cells. Low Haemoglobin Levels in Infants There are chances that a newborn develops temporary anaemia around the age of 6 to 8 weeks. It is caused when the infant runs out of the RBCs they were born with and have not yet created their new cells. This condition has no adverse effects unless they have an underlying condition. It can also result from breaking down the blood cells too fast, resulting in the yellowing of the skin, known as jaundice. Once you have interpreted your results, your doctor may advise various treatment methods based on the cause of the anaemia. Most often, the treatment for anaemia will include a change in the diet or an addition of a dietary supplement that helps with iron or vitamin deficiency. Polycythemia is a lifelong condition that is not curable. However, medicines help manage the symptoms. Book Blood Test at Home In Summary Haemoglobin is a protein present in the red blood cells that helps transport oxygen through the blood. Higher than normal haemoglobin range is caused due to polycythemia, whereas lower than average haemoglobin usually results in anaemia. Keeping track of your haemoglobin levels is especially important for individuals with a history of anaemia or at risk. Metropolis Labs is one of the leading diagnostic centres in India. They provide customers with the convenience of at-home sample collection, so you do not need to step out of the house, especially when not well. Check out the different diagnostic tests they offer to find the ones that suit you best.
Understanding Conjunctivitis Symptoms and Signs : A Comprehensive Guide
Conjunctivitis, also referred to as pink eye or eye flu, is an eye condition that can make people feel uncomfortable, irritated, and have red eyes. The thin membrane that covers the white area of the eye and the inner surface of the eyelids, the conjunctiva, becomes inflamed, which is how it is identified. To assist you in recognising and comprehending this widespread eye condition, we will break down the conjunctivitis symptoms and indicators in this post. Redness of the Eye The redness of the eyes is one of the main and most obvious signs of conjunctivitis. Because of the pink or red colour of the eye caused by the inflamed blood vessels in the conjunctiva, the condition is frequently referred to as "pink eye." Depending on the underlying cause of conjunctivitis, the degree of redness can range from mild to severe. Itching and Irritation Conjunctivitis frequently causes itching and irritation in the affected eye or eyes. People may feel the urge to touch their eyes to ease the itching, which can range from mild to severe. However, in the event of infectious conjunctivitis, scratching the eyes can exacerbate the illness and possibly transmit the infection. Watery or Discharge from the Eye Conjunctivitis can cause the eyes to tear excessively or discharge. While bacterial conjunctivitis may provide a thicker, yellow or greenish discharge, viral conjunctivitis typically results in a clear and watery discharge. Due to the body's immunological reaction to allergens, allergic conjunctivitis can also result in watery discharge. Swollen Eyelids Conjunctivitis occasionally results in swollen eyelids, making it difficult to fully open or close the eyes. The inflammation that affects the tissues of the eyelids usually causes swelling. Sensitivity to Light (Photophobia) Conjunctivitis can cause photophobia, a condition in which the eyes become sensitive to light. People who have conjunctivitis may experience discomfort and suffering when exposed to bright lights or sunshine. Crust Formation on the Eyelids Particularly after waking up in the morning, bacterial conjunctivitis can cause the development of crusts or "eye boogers" on the eyelids. These crusts develop as a result of dry discharge gathering on the eyelids while you sleep. Foreign Body Sensation Some people with conjunctivitis could feel as though they have grit or a foreign body in their eyes. This sensation may be uncomfortable and increase the desire to massage one's eyes. For early detection and suitable care, it is essential to recognise the symptoms and signs of conjunctivitis. A qualified eye care practitioner must be consulted if you suffer redness, irritation, excessive tearing, or discharge from your eyes in order to make an accurate diagnosis and receive the appropriate treatments. While the majority of conjunctivitis instances are not dangerous and can be treated with self-care or medical procedures, prompt treatment can help reduce discomfort and stop the conjunctivitis from spreading to other people. Keep in mind that having healthy eyes is crucial for sustaining vision and general wellbeing.
The Benefits of At-Home Testosterone Testing for Men's Health
Are you feeling tired, irritable, or experiencing a low sexual drive? These are all symptoms that could be related to low testosterone levels. Testosterone is a hormone. It plays an essential role in men's health and well-being. However, as we age, our testosterone levels can decrease. This can lead to a variety of health issues. The good news is that there is now an easy way to test your testosterone levels from the comfort of your own home. In this blog post, we will explore the benefits of at-home testosterone testing and how it can help improve men's health. Testosterone and men's health Testosterone plays a crucial role in men's health. It affects various body functions. These include muscle mass, bone density, and sexual drive. Testosterone also impacts mood and energy levels. Low testosterone levels are associated with fatigue, irritability, depression, and even an increased risk of heart disease. As men age, their testosterone levels naturally decline. However, lifestyle factors such as stress and poor diet can accelerate this process, resulting in low T levels at an earlier stage of life. Low testosterone levels can have serious consequences for overall health. Men with low T-levels may experience decreased muscle mass. This leads to frailty or osteoporosis later in life. They may also suffer from erectile dysfunction (ED). This causes relationship issues or psychological problems like anxiety or depression. Men need to be aware of the potential risks associated with declining testosterone levels and take steps towards maintaining optimal hormonal balance through regular testing and healthy lifestyle choices. The Benefits of At-Home Testosterone Testing The at-home testosterone test is becoming increasingly popular among men looking to monitor their health and well-being. There are several benefits to using an at-home test kit. These include convenience, privacy, and cost-effectiveness. One major advantage of at-home testing is the ability to avoid the hassle of scheduling appointments or visiting a clinic. With an at-home test kit, you can easily collect your samples and send them off for analysis without ever leaving your house. Privacy is another important benefit of at-home testing. Many men may feel uncomfortable discussing issues related to their sexual health with a healthcare provider in person. At-home testing allows individuals to maintain anonymity while still receiving accurate results. Cost-effectiveness is also a significant advantage of at-home testing. Traditional laboratory tests can be expensive, especially if they require multiple visits or follow-up appointments. By contrast, an at-home test kit provides quick and affordable results from the comfort of your home. There are many benefits to using an at-home testosterone test kit that make it an appealing option for men looking to stay on top of their health and wellness. How to Test Your Testosterone Levels at Home Here's a simple guide on how to test your testosterone levels in the comfort of your own home. Firstly, choose an at-home testosterone test kit. It suits your needs and preferences. Many reputable companies offer these kits online or over the counter in local pharmacies. Make sure to read customer reviews. Consult with a healthcare professional if you are unsure about which kit is best for you. Once you have obtained the kit, carefully read and follow the instructions provided by the manufacturer. Most tests require either a saliva or blood sample. These are collected using a cheek swab or finger prick, respectively. Ensure that all necessary precautions are taken during sample collection to avoid contamination. After collecting your sample, securely package it as instructed and mail it back to the designated laboratory for analysis. The lab will then process your sample and provide accurate results within days or weeks, depending on their processing time. Keep in mind that tracking fluctuations in testosterone levels may require multiple tests over time. Therefore, consider repeating this process every few months for a better understanding of patterns related to diet, exercise regimen, or other lifestyle factors affecting hormone balance. Remember that while at-home testing provides convenience and privacy, discussing results with qualified medical experts is crucial before making any significant changes based on findings from such tests. Treatment for low testosterone levels If you do find that you have low testosterone levels, there are various treatment options available. Your doctor may recommend lifestyle changes such as exercise and diet modifications to help boost your hormone levels naturally. In some cases, medication or hormone replacement therapy may be necessary. Remember that everyone's body is different. What works for one person may not work for another. It's important to work with your healthcare provider to determine the best course of action for managing low testosterone levels based on your individual needs. By utilising at-home testosterone testing and seeking appropriate treatment when needed, men can take proactive steps towards optimising their overall health and well-being. Foods that Boost Testosterone Levels One of the easiest ways to increase testosterone production is by consuming foods that promote it. Foods high in zinc have been shown to help with testosterone production. Additionally, vitamin D-rich foods like salmon and egg yolks can also aid in boosting T levels. Incorporating healthy fats into your diet has also been linked to increased testosterone levels. Foods like avocados, nuts (especially almonds), seeds (like pumpkin or flaxseed), and olive oil are great sources of good fats. Conclusion At-home testosterone testing is an easy and convenient way for men to monitor their hormone levels and take control of their health. By regularly testing your testosterone levels, you can identify any potential issues early on and take action to improve your overall well-being. Whether you are experiencing symptoms related to low testosterone levels or just want to stay on top of your health, an at-home testosterone test is an excellent option that provides accurate results quickly. Taking care of our hormonal balance should be considered as important as any other aspect of maintaining good health. You can book a home visit with Metropolis Labs to get your testosterone test samples collected by professional technicians. By monitoring essential hormones like testosterone, we can keep track of our body's changes over time.
 Home Visit
Home Visit Upload
Upload

















 WhatsApp
WhatsApp