Latest Blogs
Understanding Varicose Veins: Symptoms, Causes, Diagnosis, and Treatment
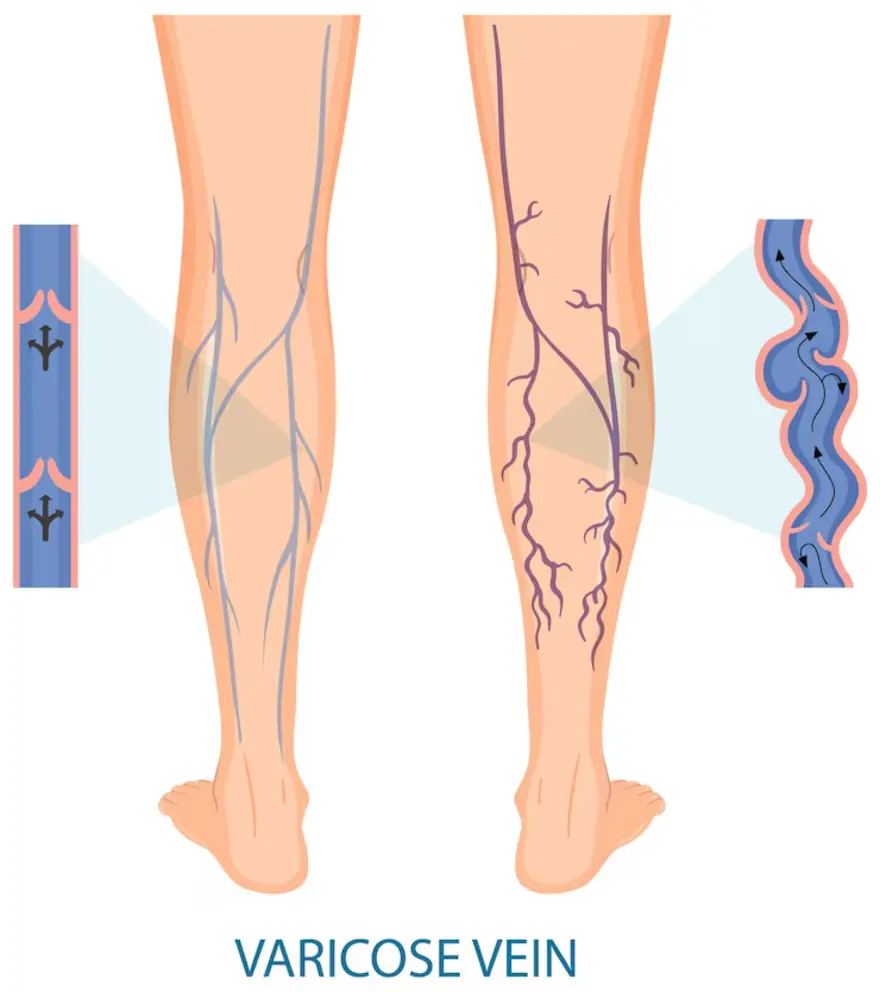
What are Varicose Veins? Varicose veins are swollen and enlarged veins that typically occur in the legs. These veins, located close to the skin's surface, become varicose due to increased pressure, especially from prolonged standing or walking. What is the Difference Between Varicose Veins and Spider Veins? Varicose veins appear knobby and twisted and have a darkish-blue hue. Spider veins resemble varicose veins but are smaller and nearer to the skin's surface. They often exhibit red or blue colours and can resemble tree branches or spider webs commonly found on the legs or face. Who is Likely to Get Varicose Veins? Varicose veins are prevalent in women, particularly during hormonal shifts like pregnancy and menopause. Moreover, the risk escalates with age but can manifest in adulthood. Certain health conditions, including obesity, Deep Vein Thrombosis (DVT), and familial history, can increase susceptibility. Therefore, it is vital for individuals, especially those with predisposing factors, to maintain wellness and consult medical professionals if symptoms arise. What are the Symptoms of Varicose Veins? Common varicose vein symptoms that arise in people are-; Appearance: Veins appear bulging, twisted, and dark purple or blue. Pain: Legs may feel achy, heavy, or sore, particularly behind the knees. Swelling: Legs, ankles, or feet may swell. Skin: Skin colour alterations around the veins, with potential brown discolourations, can be witnessed if untreated. Other symptoms include itching, burning, throbbing, or muscle cramps around the veins, which often worsen at night. Additional indicators: Sores on the legs, rash, dry, itchy, or thin skin over the affected vein. Where Do Varicose Veins Usually Appear? Varicose veins, or varicosities, present as swollen, twisted veins, can appear throughout the body. Though these are frequently observed in the legs and feet, some common sites include Calves Thighs Areas both behind and in front of the legs, especially near the ankles and feet During pregnancy, these may appear around the lower pelvic region, inner thigh, and buttocks. What Causes Varicose Veins? Varicose veins develop due to weakened or damaged vein walls and valves, which cause blood to pool and veins to become enlarged and twisted. Some other varicose vein causes include: Age: Vein elasticity diminishes with ageing. Pregnancy: Varicose veins in pregnancy occur due to increased blood volume to support the baby's heightening pressure. Overweight: Excess weight adds strain to veins. Prolonged sitting or standing: Extended periods in these positions may elevate risk. Sedentary lifestyle: Lack of activity can contribute to heightened blood pressure. Other factors: Smoking, oral contraceptives, hormone replacement therapy, leg injuries, chronic constipation, and insufficient vitamin K2 levels can also increase susceptibility to varicose veins. How are Varicose Veins Diagnosed? A healthcare professional can opt for any of the following varicose veins diagnosis: Physical examination: Your healthcare provider will assess your legs while standing to observe any swelling and examine the appearance of varicose veins. Medical history inquiry: Symptoms, family history, activity levels, and lifestyle are often discussed to understand potential risk factors. Imaging tests: A Duplex Ultrasound (DUS), a non-invasive method that utilises sound waves to evaluate blood flow in leg vessels, may be prescribed. This can help locate damaged valves contributing to varicose veins. Further investigation: If varicose veins cause pain, skin changes, or other complications, a referral to a vascular specialist may be warranted. What is the Treatment for Varicose Veins? A few varicose vein treatment options available as temporary or permanent treatments are-; Compression stockings: These garments exert pressure on the legs, aiding blood circulation. They are available over-the-counter or as prescription-strength, and insurance coverage may apply if symptoms are present. Varicose vein surgery procedures Sclerotherapy: Involves injecting a solution into varicose veins to close them. Multiple injections may be necessary, and the procedure can often be performed in the office without anaesthesia. Laser treatment: Uses bursts of light to fade varicose veins. It is a non-invasive procedure without cuts or needles. Catheter-based procedures (radiofrequency or laser energy): These methods involve heating and sealing varicose veins and are particularly effective for larger veins. High ligation and vein stripping: This outpatient procedure ties off and removes varicose veins through small incisions. Ambulatory phlebectomy: Smaller varicose veins are removed through tiny skin pricks, resulting in minimal scarring. This procedure is also performed on an outpatient basis. What are the Complications/Side Effects of the Treatment? Possible complications or side effects of varicose vein treatments include: Temporary bruising or discolouration in the treated area Swelling or discomfort may occur Skin irritation or rash could develop Allergic reactions to medications used during procedures are rare but possible Numbness or tingling sensations may be experienced Blood clots can occur, although they are uncommon Infection or nerve damage is rare, but potential risks Varicose veins may recur over time Scarring or changes in skin texture may occur How Can I Prevent Varicose Veins? Consider these lifestyle adjustments to prevent varicose veins potentially: Incorporate regular exercise to enhance blood flow and muscle tone. Aim for activities like walking or cycling for 30 minutes 3–5 times per week. Maintain a healthy weight to alleviate pressure on the veins. Adopt a balanced diet low in salt and rich in fibre to mitigate water retention, a factor contributing to varicose veins. Be mindful of your sitting posture; avoid crossing your legs and elevate your legs when seated or lying down. Opt for appropriate footwear, avoiding high heels or tight stockings except for compression stockings. Take breaks to change positions frequently, incorporating stretching or short walks every 30 minutes. What is the Outlook for People with Varicose Veins? The outlook for individuals with varicose veins is generally positive. With appropriate management, including lifestyle adjustments and medical interventions as necessary, most people can effectively control symptoms and minimise complications. However, regular monitoring is essential to prevent potential worsening or complications. What are the complications of varicose veins? Potential complications of varicose veins include: Ulcers: Painful sores may develop near varicose veins, particularly around the ankles. Blood clots: Enlarged veins deep within the legs can lead to clot formation. Bleeding: In rare instances, superficial veins may rupture. Leg swelling: Prolonged varicose veins can result in swelling of the legs. Do varicose veins return after treatment? Varicose veins can indeed recur after treatment, with approximately 60% of individuals experiencing a reappearance within five years. Conclusion Varicose veins are common and can recur even after permanent varicose vein treatment. However, with proper management and lifestyle adjustments, individuals can often control varicose vein symptoms and minimise complications. Remember, regular monitoring is key to maintaining vein health. For convenient at-home testing and check-ups, consider using Metropolis Healthcare/Labs services, ensuring comprehensive care from the comfort of your home.
Klinefelter Syndrome: Symptoms, Complications, Diagnosis Explained
What is Klinefelter syndrome? Klinefelter syndrome is a type of genetic condition in which an extra X chromosome is present in the genetic code. In general, individuals have 46 chromosomes, including the XX (female) and XY (male) chromosomes. However, in the case of Klinefelter syndrome in males, the individual has an extra X chromosome, making the total 47. Klinefelter syndrome is a condition that you are born with, and the Klinefelter syndrome symptoms you display may be different from that of another individual. Many people might receive a Klinefelter syndrome diagnosis early in life, but some do not even know they have Klinefelter syndrome till adulthood when they experience symptoms like infertility. Today, most cases of Klinefelter syndrome can be identified through prenatal genetic screening. How common is Klinefelter syndrome? Klinefelter syndrome is a common condition, with 1 in 600 males with the genetic abnormality. However, it is believed that almost 70% to 80% of these individuals may not be aware that they have Klinefelter syndrome. What are the symptoms of Klinefelter syndrome? Your Klinefelter syndrome symptoms may vary in severity based on how many extra X chromosomes you have. Some people with Klinefelter syndrome may display several of the below-mentioned symptoms, while others may not show any apparent signs. Klinefelter syndrome symptoms are categorised into physical and neurological types. Physical Klinefelter syndrome symptoms Physical Klinefelter syndrome symptoms affect the body and how it works. Males with Klinefelter syndrome may have: A smaller penis Undescended testicles Flat feet Atypical body proportions, for example, can be tall with long legs and a shorter trunk Coordination issues Testicular issues, including the lack of sperm or testosterone creation Weak bone structure, increasing the risk of fractures Risk of blood clots Fertility issues Neurological Klinefelter syndrome symptoms Neurological Klinefelter syndrome symptoms include learning differences, mental health issues, and behavioural issues. Including: Anxiety Social, emotional, or behavioural issues Learning difficulties, especially when reading and language challenges Impulsive behaviour Attention-deficit/hyperactivity disorder Speech delay Autism spectrum disorder Depression What causes Klinefelter syndrome? Klinefelter syndrome is when the individual has an extra X chromosome in their genetic code. This can happen in three different ways. Klinefelter syndrome causes include: If there is an extra X chromosome present in the sperm There is an extra X chromosome in the egg The cells divide incorrectly during foetal development, in which case some cells and not all have extra X chromosomes. What are the complications of Klinefelter syndrome? Individuals with Klinefelter syndrome may develop metabolic conditions such as: Type 2 diabetes Hypertension/High Blood Pressure Obesity High cholesterol High triglycerides Other Klinefelter syndrome complications include: Breast cancer Tremors Osteoporosis Gynecomastia Autoimmune conditions like rheumatoid arthritis, lupus, type 1 diabetes, thyroid disease Seizures How is Klinefelter syndrome diagnosed? Klinefelter syndrome can be diagnosed at multiple stages of an individual's life, such as: During foetal development, when running genetic tests like amniocentesis or chorionic villus sampling During childhood or teenage years when your healthcare provider may notice abnormal growth or delayed development (during puberty) During adulthood, if you have to test for fertility issues such as low testosterone Most people with mild cases of Klinefelter syndrome may not display any Klinefelter syndrome symptoms, thus never knowing they have this condition. What tests can help diagnose Klinefelter syndrome? Genetic tests that aim to detect and identify extra X chromosomes help diagnose Klinefelter syndrome. Karyotyping is one of the most commonly used genetic tests where a blood sample is collected and studied to determine the number and type of chromosomes present in the cells. Karyotyping can be used for children, adults and even foetuses before birth. Children with Klinefelter syndrome may also need to undergo neuropsychological testing regularly to identify any learning challenges and help educators navigate the issue effectively. What are the treatment options for Klinefelter Syndrome? As this condition is something you are born with, Klinefelter syndrome treatment revolves around emanating the symptoms and not curing or getting rid of them. Klinefelter syndrome treatment options include Hormone Replacement As individuals with Klinefelter syndrome have issues with fertility and the production of testosterone, Klinefelter syndrome medication can help regulate hormones and minimise some of the symptoms of Klinefelter syndrome. Some people with Klinefelter syndrome may not start puberty, while others may start it but stop midway or regress. This may happen because the testicles "fail" and are not able to create sperm or testosterone. Most healthcare providers may suggest testosterone injections for smaller kids and teenagers, while adults with Klinefelter syndrome may need other Klinefelter syndrome treatment options, such as testosterone gels or patches. The main goals of hormone replacement therapy are: more facial and body hair a deeper voice increasing muscle strength increasing bone health increased sexual desire improved mood, overall mental health, and self-image Therapy As part of your Klinefelter syndrome treatment, you may need to visit: A speech therapist to aid in speech development Physical therapist to build muscles Occupational therapists for better skill and coordination Family, educational, or behavioural therapist for psychological support. Surgery Individuals with Klinefelter syndrome are more likely to develop extra breast tissue that is likely to stay. If the extra tissue causes grief, your doctor may suggest gynecomastia surgery to get rid of the excess tissue. Is Klinefelter syndrome preventable? As Klinefelter syndrome is due to a change in your genetic code, it is almost impossible to prevent. What is the outlook for Klinefelter syndrome? If you or your child receive a Klinefelter syndrome diagnosis, you should meet a genetic counsellor as soon as possible. You may also need to visit an endocrinologist who will advise you on when to start testosterone replacement therapy or other treatment options. How long can a person live with Klinefelter syndrome? Individuals with Klinefelter syndrome can live an entire, happy, healthy life by taking the Klinefelter syndrome treatment. When to see a doctor? Parents should schedule a visit to their healthcare provider if they notice developmental delays like crawling, learning to walk, or talking. In the teenage years, if you see your child has any of the mentioned physical symptoms, such as short torsos, long legs, or is taller than average, then visit the doctor without any delay. Adults with Klinefelter syndrome should visit the doctor if they notice any new symptoms or a change in existing symptoms. Conclusion After learning that your child has Klinefelter syndrome do not panic. With the help of your healthcare provider, regular testing, and therapy, those with Klinefelter syndrome can live a healthy life. We at Metropolis Labs provide reliable health check-ups and testing facilities. For those who are not willing to step out of their house, we also provide an at-home testing facility. Experts collect the sample from your home and the accurate results are shared with you at either Metropolis labs app or online via email.
Everything You Need To Know About Impetigo
What is Impetigo? Impetigo is a common bacterial infection of the skin. It can affect anyone but is most commonly found in children with sensitive skin conditions or adults with weakened immune systems and diseases like diabetes. Impetigo causes the formation of sores and blisters that appear differently depending on the stage of the infection and the part of the body it affects. Impetigo is a highly contagious skin disease caused by bacteria like Streptococcus pyogenes that affect the epidermis (outer layer of the skin). The Impetigo bacteria often enters the body through open cuts, insect bites, or other rashes. However, there have been rare cases in children who showed impetigo symptoms even when they had no prior injury or breakage of skin. Impetigo often occurs in warmer months when children play outside. What are the types of Impetigo? There are three major impetigo types, including: Non-bullous Impetigo This is the earliest stage of Impetigo and the most common type. This stage of Impetigo is characterised by developing one or multiple impetigo sores that itch and quickly burst the skin that has broken open will appear red or raw glands near these sores are often swollen a honey-coloured crust forms over the impetigo sores, but this skin quickly heels without leaving any scars Bullous Impetigo This is rarer than Impetigo and is more commonly found in infants. Approximately 90% of all bullous impetigo cases can be found in children below the age of two years. This type of Impetigo is identified with: Large, fluid-filled blisters on the child's skin Blisters that have become clean and limp before breaking open Crust formation over the sores Ecthyma When any of the above impetigo types are left untreated, they can evolve into ecthyma. This kind of Impetigo infection goes deeper into the child's skin, and the stages involve: Painful blisters that form deep open sores development of thick crusts on the skin with redness around the infected area lingering scars even after the epidermis has healed because the Impetigo infection seeps more deeply into the skin What are the symptoms of Impetigo? Initial impetigo symptoms include the formation of discoloured sores on your child's skin, which can be found in clusters around the nose and lips. The impetigo rash appears red or pink on lighter skin tones, while darker skin tones get a dark red, purple, brown, or grey rash. The Impetigo sores proliferate into more prominent blisters that can ooze, burst, and form a yellowish crust. These clusters of Impetigo blisters can also expand and cover more area on the skin. Impetigo sores are often itchy and painful and can form discoloured marks once the crust phase is completed. What are the causes of Impetigo? Certain types of bacteria, such as Staphylococcus aureus (which causes 80% of non-bullous impetigo cases) and group A streptococcus (which causes 10% of non-bullous Impetigo instances), are the main Impetigo causes. Impetigo infection may occur when one of the bacteria mentioned above enters the child's body through a scrape, cut, insect bite, or rash. Once the bacteria enters the body, impetigo symptoms may appear as inflammation on the skin. Impetigo can also occur when your child scratches some form of rash, like chickenpox or eczema, where the skin breaks, giving way for the bacteria to enter. Impetigo in adults occurs because of breakage in the skin, as mentioned above, and other health conditions, such as tattoo infections, scabies, and herpes. Is Impetigo contagious? Impetigo is a highly contagious disease that can be caught through skin-to-skin contact. You may develop symptoms if you come in contact with open sores, nasal discharge, or mucus of someone infected with Impetigo. This is one of the most common Impetigo causes in children and athletes. Sharing personal items like clothing or towels can also cause the spread of the disease. What are the risk factors? Impetigo can develop in anyone, but certain groups of people are more susceptible to impetigo infections. These include children and adults who: live in places that are humid and warm stay in crowded places for more extended periods, like daycare centres, schools or training facilities have compromised immune systems have diabetes suffer from skin conditions like dermatitis, psoriasis, or eczema have insect bites or rash from poison ivy have itchy infections like scabies, herpes simplex, or lice Age is another important risk factor, as Impetigo is more common among kids between 2 and 5. What are the complications of Impetigo? Impetigo is a mild infection; it may turn serious if left untreated for an extended period. Following infections and harmful immune responses are the main impetigo complications: Soft tissue infection Toxic shock syndrome Rheumatic fever Staphylococcal scalded skin syndrome Adults pose a higher risk of complications related to Impetigo, including: Cellulitis Sepsis Lymphangitis Acute post-streptococcal glomerulonephritis How is Impetigo diagnosed? You may be diagnosed with Impetigo based on how the skin sores look. A skin sample may be sent to the labs for a skin culture, which helps confirm the diagnosis and determine the right antibiotic for the infection. How do you treat Impetigo? Antibiotics are the most common option for impetigo treatment. Your healthcare provider will prescribe topical impetigo therapy, in which an antibiotic ointment is applied directly to the child's skin. However, if the infection has spread to a larger portion of the skin, you may also need to take oral impetigo medication like cephalosporins, sulfamethoxazole, or clindamycin. When to see a doctor? Minor Impetigo infections can go away on their own; however, if the infection develops into deeper or more serious wounds and punctures, you may need to see a doctor. Can I prevent Impetigo? Maintaining good hygiene is one of the best ways to prevent Impetigo infection. Regular baths and hand washing can reduce the amount of bacteria on your skin. The best way to avoid the spread of the rash is to cover the area with an open Impetigo wound or bug bite. Keep your nails clean and clipped, avoid scratching open sores that can cause the spread of the infection, and wash everything that comes in contact with the impetigo sores. Conclusion Impetigo is a highly contagious skin condition caused by bacteria. Most cases can heal independently without impetigo treatment, by taking the proper precautions and following good hygiene. However, more severe impetigo symptoms may require you to visit a doctor and get a skin culture to determine the impetigo cause, followed by a treatment plan. Metropolis Labs India is the leading diagnostic service that provides convenient at-home and in-lab tests. Contact us today to set up your appointment.
Atrial Fibrillation: Symptoms, Causes, Treatment Options & More
Introduction: Atrial fibrillation may not be life-threatening per se. However, if left untreated, the irregular heart rhythm in atrial fibrillation can turn serious. Let's dig deeper to understand it better. What is Atrial Fibrillation? Atrial fibrillation, also known as Afib, is a condition when the heart beats irregularly and often too fast. In Afib, the top part of the heart contracts rapidly, giving a 'fluttering' or 'skipping beat' kind of sensation instead of beating effectively. How Does Atrial Fibrillation Affect the Heart? In atrial fibrillation, the usual pattern of electrical signals in your heart gets disturbed, causing irregularities that can affect how effectively your heart pumps blood. During Afib, the upper chambers of the heart (atria) do not contract properly, causing blood to pool and move inefficiently. As a result, less blood is pumped from the atria to the lower chambers (ventricles) of the heart, affecting the overall circulation of blood in your body. The pooling may also cause blood clots to form, leading to strokes or heart failure. What are the Types of Atrial Fibrillation? There are four types of atrial fibrillation: Paroxysmal atrial fibrillation: The atrial fibrillation symptoms may come and go, lasting from a few seconds to hours, and subside within a week. Persistent atrial fibrillation: In this type of Afib, the irregular heartbeat lasts more than a week. Long-standing persistent atrial fibrillation: This type of Afib is constant, lasting for more than 12 months. Permanent atrial fibrillation: In this type of Afib, the irregular heart rhythm cannot be reversed. What are the Symptoms of Atrial Fibrillation? The commonly felt atrial fibrillation symptoms are: Palpitation (faster heartbeat) Chest pain and discomfort Shortness of breath Dizziness Lightheadedness Fainting Confusion Inability to exercise Some people may not experience atrial fibrillation symptoms at all, i.e., have asymptomatic Afib that can only be detected during regular health check-ups. What causes Atrial Fibrillation? Atrial fibrillation occurs due to an alteration in the heart's electrical system or tissue injury. Hyperthyroidism, high blood pressure and coronary artery disease can also be atrial fibrillation causes. A triggered heartbeat usually sets off Afib. However, it’s hard to pinpoint the exact atrial fibrillation causes for the same. Research is still ongoing to uncover the specific conditions. Beyond this, poor lifestyle choices and family history increase the risk of atrial fibrillation. How is Atrial Fibrillation Diagnosed? For an effective atrial fibrillation diagnosis, you may have to share your medical and family history, routine activities, diet, and symptoms. Then, your doctor may check your heartbeat, pulse, blood, thyroid gland size, etc., to determine how your body is functioning. Tests to Diagnose Atrial Fibrillation Along with a physical examination, your doctor may suggest certain atrial fibrillation diagnosis tests, which may help in selecting the right treatment plans, like: Electrocardiogram (ECG): Measures your heart's electrical activity and detects irregular rhythms. Holter Monitor: Worn for 24 to 48 hours, this monitor records your heart's activity during daily life, providing comprehensive data for understanding and treating atrial fibrillation. Event Monitor: Like a Holter monitor but worn for up to 30 days, the event monitor records heart rhythm only when activated in response to atrial fibrillation symptoms, tracking irregularities. Echocardiogram: Using sound waves, an echocardiogram creates images of your heart's structure and function for the identification of any underlying conditions. Blood Tests: To assess potassium and thyroid hormone levels and evaluate liver and kidney function to rule out imbalances that may cause Afib. What are the Treatments For Atrial Fibrillation? Atrial fibrillation treatment focuses on controlling your heart rate. Your options may include: Medication: Beta-blockers, calcium channel blockers, or antiarrhythmic drugs help control the heart rate. You may also need blood thinners to lower the risk of blood clots and stroke. Cardioversion: Electrical shocks (electric cardioversion) or medication (chemical cardioversion) are used to restore the heart's normal rhythm. This can be a one-time treatment or may need to be repeated. Catheter Ablation: If none of the above works, your doctor may recommend catheter ablation. This involves inserting thin tubes (catheters) into your heart to zap and restore normal electrical signals. Surgical Procedures: Maze surgery or surgical ablation may be used to create scar tissue in your heart to disrupt abnormal electrical pathways and restore normal rhythm. What are the Complications of Atrial Fibrillation? Blood clots (embolus) are a serious complication of Afib. They can reduce blood flow to the brain, resulting in a reduced oxygen supply to brain cells. This can affect cognitive functions such as memory, focus, reasoning, and problem-solving ability. In serious cases of Atrial fibrillation, the embolus can also cause strokes or permanent damage to the brain. Afib wears and tears the heart muscles as the ventricles strain to compensate for the reduced blood flow from the atria. This may result in heart failure if left untreated. What are the Risk Factors for Atrial Fibrillation? The risk factors for atrial fibrillation increase with age (above 65 years), including: High blood pressure Heart disease Diabetes Obesity Excessive alcohol consumption Smoking Sleep apnea (breathing difficulty during sleep) Family history of Afib How do I Stop Worrying About Afib? Managing atrial fibrillation can be overwhelming, but here are some steps to ease your worries: Stay informed about your condition Follow your atrial fibrillation treatment plan Maintain a healthy lifestyle Seek support from doctors, family, and friends. Is Afib a Serious Heart Condition? Yes, atrial fibrillation can be a serious condition, but with proper medication and lifestyle management, you can reduce the risk of complications such as stroke and heart failure and lead an active and fulfilling life. Does Afib Go Away on its Own? In some cases, your atrial fibrillation may resolve on its own, particularly if it is triggered by excessive alcohol consumption and stress. However, for many people, it is a chronic condition that requires continuous management. Does Afib Cause Heart Attacks? While atrial fibrillation itself does not cause a heart attack, the embolus created due to blood pooling can travel to arteries that supply blood to the heart and brain and lead to a heart attack or stroke. What Does Atrial Fibrillation Feel Like? Afib can feel different for each person; however, most people complain of quivering in the chest and a racing heart that may last for a few minutes. Other Atrial fibrillation symptoms discussed above may also manifest. Conclusion Living with atrial fibrillation can be challenging, but remember that you’re not alone. By understanding your condition, following your atrial fibrillation treatment plan, and making healthy lifestyle choices, you can effectively manage atrial fibrillation and reduce the risk of Afib-related complications. Metropolis Diagnostic Lab offers comprehensive diagnostic services tailored to your individual needs. For advanced cardiac testing, you can rely on Metropolis Diagnostic Lab to provide accurate and timely results. Take control of your health journey today with Metropolis Diagnostic Lab by your side.
Inguinal Hernia: Exploring Causes, Symptoms and Treatment Options
While inguinal hernias are non-fatal, they can hamper regular activities. Here is a quick guide on the condition, its causes, symptoms and treatments. What is an inguinal hernia? An inguinal hernia occurs when a tissue, usually a part of the intestine, protrudes through a weak spot in the abdominal muscles into the inguinal canal in the groin area. This type of hernia is prevalent and can cause discomfort or pain, especially when lifting heavy objects, coughing, or straining during bowel movements. What are the symptoms of an inguinal hernia? Symptoms of an inguinal hernia include: Pain or discomfort in the groin while bending over, coughing, or lifting A bulge or swelling in the groin area that becomes more prominent while standing or straining A feeling of heaviness or pressure in the groin Aching or burning sensation at the site of the bulge Weakness, discomfort, or pain in the scrotum in men Nausea and vomiting, particularly if the hernia becomes trapped or incarcerated What are the types of inguinal hernia? There are two main inguinal hernia types: Indirect inguinal hernia: This is most common in children and is caused by a congenital defect in the abdominal wall, a persistent opening that does not close during fetal development, or weakness in the inguinal canal. Direct inguinal hernia: These inguinal hernia types typically develop in older adults due to muscle weakness or ageing. What are the causes of inguinal hernia? A combination of factors typically causes inguinal hernias: Weakness in the abdominal muscles: This is considered a major contributor to inguinal hernias. Increased pressure on the abdominal cavity: Heavy lifting, persistent coughing, straining during bowel movements, or obesity can lead to tissue herniation through weakened areas of the abdominal wall. Congenital predisposition: This means being born with a higher risk due to genes and inheriting weakness in the abdominal wall or inguinal canal. What are the risk factors of inguinal hernia? Several risk factors contribute to the development of inguinal hernia: Male gender: Men are more prone to inguinal hernias due to a natural weakness in the inguinal canal. Inguinal hernia female cases make it to only 1.9%. Old age: Ageing weakens abdominal muscles, increasing the risk of herniation. Family history: Having a family history predisposes individuals to develop inguinal hernias. Obesity: Excess weight puts strain on the abdominal muscles, making hernias more likely. Chronic constipation: Straining during bowel movements increases abdominal pressure, which can lead to inguinal hernia. Heavy lifting: Jobs or activities involving frequent heavy lifting can strain the abdominal muscles and cause inguinal hernia. Chronic cough: Persistent coughing, often due to smoking or underlying respiratory conditions, can weaken abdominal muscles and increase the inguinal hernia risk. Inguinal hernias in newborns Inguinal hernias are common among newborns and premature infants, occurring in about 1% to 5% of babies. These bulges in the groin or scrotum may become more noticeable during periods of increased intra-abdominal pressure, such as when the baby cries and may recede or disappear at other times. How is an inguinal hernia diagnosed? The inguinal hernia diagnosis process may involve the following steps: Medical History: The doctor will inquire about your inguinal hernia symptoms, medical history and risk factors. Physical Examination: The doctor will examine the groin area while you're standing and lying down, looking for a bulge or swelling in the groin or scrotum, which is characteristic of an inguinal hernia. Cough Test: You may be asked to cough or strain during the exam to help the doctor detect the hernia more easily. Imaging Tests: In some cases, imaging tests such as ultrasound, CT scan, or MRI may be recommended to confirm the diagnosis or evaluate the extent of the hernia. What is the treatment for inguinal hernia? Your physician may suggest a surgical repair or watchful waiting approach depending upon inguinal hernia symptoms. Here are the details: Inguinal Hernia Surgery Open procedures: Bassini technique or Lichtenstein tension-free hernioplasty involves making an incision near the hernia, pushing the protruding tissue back into place, and reinforcing the weakened abdominal wall with stitches or mesh. Laparoscopic repair: It involves smaller incisions and the use of a camera and specialized instruments to repair the hernia, often with less pain and quicker recovery. Inguinal Hernia Treatment without Surgery If the inguinal hernia is small and asymptomatic, it may be treated with close monitoring and lifestyle modifications, such as dietary changes and avoiding stress. Temporary Hernia Treatment These methods aim to alleviate symptoms and discomfort. You can wear a supportive corset, binder, or truss to temporarily relieve pain by exerting gentle pressure on the inguinal hernia site. Over-the-counter pain relievers may also be used to manage hernia-related pain temporarily. How can I reduce my risk of getting an inguinal hernia? To reduce the risk of developing an inguinal hernia, you can follow these tips: Avoid Heavy Lifting: Minimise lifting heavy objects, especially if you are not accustomed to it. Lift Properly: Learn and practice proper lifting techniques to avoid strain on your abdominal wall. Maintain a Healthy Weight: Manage obesity through a healthy diet and exercise to decrease the risk of inguinal hernias. Strengthen Core Muscles: Exercises, such as planks, strengthen your core muscles and provide better support to your abdominal wall. Treat Constipation Promptly: Stay hydrated and eat a fibre-rich diet to prevent constipation that strains abdominal muscles. Quit Smoking: Smoking weakens abdominal muscles and increases the risk of chronic coughing. Quitting it can reduce the inguinal hernia causes. Treat Chronic Cough: Treating underlying conditions causing coughing, such as respiratory infections or asthma, can help reduce the risk. What are the complications of inguinal hernia? Complications of inguinal hernia repair surgery may include: Surgical Site Infection: Infections at the incision site can occur, ranging from superficial to deep incisional infections. Mesh Complications: Mesh migration and erosion, where the surgical mesh used to repair the hernia may move from its original position or cause tissue erosion. Recurrence: Despite surgery, hernias can sometimes recur, necessitating further treatment. Chronic Pain: This may be experienced in some cases due to nerve damage, scar tissue formation, or other factors. Urinary Symptoms: In rare cases, surgery for inguinal hernia repair may lead to genitourinary complications, such as urinary retention or other urinary symptoms. Conclusion In conclusion, while inguinal hernia treatment aims to alleviate symptoms, accurate diagnosis through physical examination, ultrasound, or MRI is crucial to effectively managing and mitigating any risks. Routine follow-up appointments with your doctor to monitor recovery progress help treat inguinal hernias better. Metropolis Labs offers comprehensive diagnostic services, including imaging studies like an abdominal ultrasound, CT scan or MRI and blood tests, to support the effective management of inguinal hernias. Trust in Metropolis Healthcare's expertise and commitment to precision in diagnostics for comprehensive care and peace of mind.
ड्राई फ्रूट खाने के 8 अद्भुत फायदे
सूखे मेवे निश्चित रूप से एक स्वादिष्ट स्नैक विकल्प हैं। लेकिन जानते हो? वे सबसे अधिक पौष्टिक और स्वास्थ्यवर्धक स्नैक्स में से एक हैं! हाँ, और सूखे मेवों के इन सभी स्वास्थ्य लाभों के साथ, चुनने के लिए कई अलग-अलग किस्में हैं, इसलिए आप अपनी स्वाद कलियों के लिए एकदम सही विकल्प पा सकते हैं। इसलिए यदि आप एक स्वस्थ नाश्ते की तलाश में हैं जो आपको संतुष्ट महसूस कराए, तो कुछ सूखे फल अवश्य लें! अभी तक आश्वस्त नहीं? सूखे मेवे खाने के कुछ अनगिनत उल्लेखनीय फायदे यहां दिए गए हैं। पोषक तत्वों का महान स्रोत सूखे फल पोषक तत्वों, विशेषकर फाइबर से भरपूर एक स्वस्थ और सुविधाजनक नाश्ता है। फाइबर एक महत्वपूर्ण पोषक तत्व है जो हमें स्वस्थ रखने में मदद करता है, हृदय स्वास्थ्य और रक्त शर्करा नियंत्रण में भी लाभ पहुंचा सकता है। सूखे फल में ताजे फल की तुलना में अधिक विटामिन और खनिज होते हैं, जो इसे पोषण बढ़ाने का एक शानदार तरीका बनाता है। हालाँकि, सूखे फल को कम मात्रा में खाना आवश्यक है, क्योंकि इसमें चीनी और कैलोरी की मात्रा अधिक हो सकती है। सूखे फल चुनते समय, बिना चीनी वाले या केवल हल्के मीठे वाले विकल्पों की तलाश करें, और अतिरिक्त चीनी के लिए लेबल की जाँच करें। थोड़ी सी योजना के साथ, सूखे मेवे आपके आहार का एक पौष्टिक और स्वादिष्ट हिस्सा हो सकते हैं। हीमोग्लोबिन का बढ़िया स्रोत सूखे मेवों का एक बड़ा लाभ यह है कि वे हीमोग्लोबिन-निर्माण और आयरन का एक अच्छा स्रोत हैं, यही कारण है कि यह एनीमिया के खिलाफ लड़ाई में सहायक हो सकता है। इसमें फोलिक एसिड जैसे अन्य आवश्यक पोषक तत्व भी होते हैं, जो नई लाल रक्त कोशिकाओं और विटामिन सी का उत्पादन करने में मदद करते हैं, जो आयरन के अवशोषण में सहायता करते हैं। सूखे फल ऊर्जा और आवश्यक पोषक तत्वों को बढ़ावा देने का एक आसान तरीका है, जिससे यह एनीमिया से पीड़ित या एनीमिया के खतरे वाले लोगों के लिए एक उत्कृष्ट नाश्ता बन जाता है। यदि आप आयरन सप्लीमेंट लेते हैं तो अपने सूखे फलों का सेवन सीमित करना सुनिश्चित करें, क्योंकि बहुत अधिक आयरन हानिकारक हो सकता है। कैंसर को रोकने में मदद करता है शोध से पता चलता है कि सूखे फल कैंसर को रोकने में भी मदद कर सकते हैं। अध्ययनों से पता चला है कि नियमित रूप से सूखे खुबानी खाने से डिम्बग्रंथि के कैंसर के खतरे को कम करने में मदद मिल सकती है। इसके अलावा, सूखे फल को कोलन कैंसर से बचाने में भी मददगार पाया गया है। उच्च फाइबर सामग्री पाचन तंत्र को स्वस्थ रखने में मदद करती है, जबकि एंटीऑक्सिडेंट सूजन को कम करने में मदद करते हैं। इसलिए यदि आप कैंसर को रोकने में मदद करने के लिए एक स्वस्थ नाश्ते की तलाश में हैं, तो कुछ सूखे फल लें। अपनी हड्डियों को मजबूत करें सूखे मेवे आपकी हड्डियों को मजबूत बनाने के लिए एक स्वस्थ और स्वादिष्ट भोजन स्रोत हैं। वे हड्डियों के स्वास्थ्य के लिए आवश्यक विटामिन, खनिज और एंटीऑक्सीडेंट से भरपूर हैं। उदाहरण के लिए, सूखे खुबानी कैल्शियम का एक अच्छा स्रोत हैं, जो मजबूत हड्डियों के लिए आवश्यक है। सूखे आलूबुखारे में मैग्नीशियम और पोटेशियम भी उच्च मात्रा में होते हैं, ये दो खनिज हड्डियों के घनत्व के लिए महत्वपूर्ण हैं। इसके अलावा, सूखे फल सूजन को कम करने और कोशिका क्षति को रोकने में मदद कर सकते हैं। परिणामस्वरूप, प्रतिदिन एक मुट्ठी सूखे फल खाने से आपकी हड्डियों को स्वस्थ और मजबूत रखने में मदद मिल सकती है। वजन घटाने को बढ़ावा दें सूखे फल वजन घटाने को बढ़ावा देने में मदद कर सकते हैं। ताजे फल के विपरीत, जिसमें अक्सर चीनी और कैलोरी अधिक होती है, सूखे फल में चीनी और कैलोरी कम होती है। इसके अलावा, सूखे मेवे फाइबर का एक अच्छा स्रोत हैं, जो खाने के बाद आपको भरा हुआ और संतुष्ट महसूस कराने में मदद करते हैं। इन कारणों से, सूखे मेवों को अपने आहार में शामिल करना वजन कम करने का एक प्रभावी तरीका हो सकता है। सूखे फल चुनते समय, ऐसी किस्मों का चयन करें जो बिना चीनी वाली हों या केवल हल्की मीठी हों। और अपने हिस्से के आकार पर ध्यान देना सुनिश्चित करें, क्योंकि इसके केंद्रित स्वाद के कारण सूखे फल को अधिक खाना आसान है। हालाँकि, थोड़ी योजना और संयम के साथ, सूखे फल किसी भी वजन घटाने की योजना का स्वादिष्ट और स्वस्थ हिस्सा हो सकते हैं। याददाश्त में सुधार करता है याददाश्त के संबंध में, कुछ चीजें स्वस्थ आहार से भी अधिक महत्वपूर्ण हैं। एंटीऑक्सिडेंट और ओमेगा-3 फैटी एसिड से भरपूर खाद्य पदार्थ मस्तिष्क की शक्ति को बढ़ाने और संज्ञानात्मक गिरावट से बचाने में मदद करते हैं। सूखे मेवे इन पोषक तत्वों को आपके आहार में शामिल करने का एक शानदार तरीका है। किशमिश में मौजूद एंटीऑक्सिडेंट मस्तिष्क को क्षति से बचाने में मदद करते हैं, जबकि ओमेगा -3 फैटी एसिड स्वस्थ कोशिका कार्य का समर्थन करते हैं। खुबानी, अंजीर और खजूर जैसे अन्य सूखे फल भी इन पोषक तत्वों से भरपूर होते हैं और स्वस्थ आहार के हिस्से के रूप में इसका आनंद लिया जा सकता है। त्वचा की गुणवत्ता में सुधार करता है सूखे फल में स्वस्थ त्वचा के लिए आवश्यक पोषक तत्व होते हैं, जिनमें विटामिन ए और सी, एंटीऑक्सिडेंट और फाइबर शामिल हैं। बस मुट्ठी भर किशमिश या खुबानी आपकी त्वचा को निखार सकती है, इसकी बनावट और रूप को बेहतर बनाने में मदद कर सकती है। इसके अलावा, सूखे फल में मौजूद प्राकृतिक शर्करा त्वचा को एक्सफोलिएट करने, उसे नरम और अधिक चमकदार बनाने में मदद कर सकती है। तो, अगली बार जब आप ऐसे नाश्ते की तलाश में हों जो आपकी त्वचा के लिए अच्छा हो, तो अस्वास्थ्यकर जंक फूड के बजाय कुछ सूखे फल खाएं। आपकी त्वचा आपको धन्यवाद देगी! स्वस्थ बाल जबकि अधिकांश लोग बालों के स्वास्थ्य के संबंध में जामुन और अन्य ताजे फलों के बारे में सोचते हैं, सूखे फल भी उतने ही फायदेमंद हो सकते हैं। उदाहरण के लिए, सूखे खुबानी बीटा-कैरोटीन का एक अच्छा स्रोत हैं, जिसे शरीर विटामिन ए में परिवर्तित करता है। विटामिन ए बालों के रोम को स्वस्थ रखने के लिए आवश्यक है और सूजन को कम करने और उपचार को बढ़ावा देने में मदद कर सकता है। यदि आप स्वस्थ बालों को बनाए रखने के लिए प्राकृतिक तरीके की तलाश में हैं, तो अपने आहार में कुछ सूखे फल शामिल करें। आपको बिना किसी चीनी के ताजे फल के समान पोषक तत्व मिलेंगे। बस बिना किसी अतिरिक्त चीनी या परिरक्षकों वाली किस्म का चयन करना सुनिश्चित करें। बिदाई शब्द तो, अगली बार जब आप एक स्वस्थ नाश्ते की तलाश में हों या अपने आहार में कुछ विटामिन और खनिज शामिल करना चाहें, तो सूखे फल का एक टुकड़ा लें। आप अपने शरीर का भला कर रहे होंगे! सूखे फल फाइबर, एंटीऑक्सीडेंट, विटामिन और खनिजों का एक उत्कृष्ट स्रोत हैं। यह रक्त शर्करा के स्तर को नियंत्रित करने, हृदय स्वास्थ्य में सुधार करने और ऊर्जा स्तर को बढ़ावा देने में भी मदद कर सकता है। साथ ही, यह स्वादिष्ट है!
अनिद्रा (नींद न आना): क्या है, लक्षण, कारण और उपचार
अनिद्रा एक सामान्य नींद विकार है जिसमें आपको नींद न आने या देर तक नींद न आने जैसी समस्याओं का सामना करना पड़ता है। वापस सोने में कठिनाई या सुबह जल्दी उठना इस नींद विकार का महत्वपूर्ण हिस्सा है। यह एक तीव्र, अल्पकालिक या दीर्घकालिक समस्या हो सकती है जो आ और जा सकती है या महीनों या उससे भी अधिक समय तक बनी रह सकती है। इस स्थिति के सबसे आम कारणों में पारिवारिक दबाव, दर्दनाक घटनाएँ या काम का तनाव शामिल हैं। अध्ययनों के अनुसार, आधुनिक उपकरणों की घुसपैठ और बदलती जीवनशैली के कारण लगभग 93% भारतीयों को पर्याप्त नींद नहीं मिल पाती है। क्रोनिक अनिद्रा के अधिकांश मामले गौण होते हैं, जिसका अर्थ है कि वे किसी अन्य समस्या का दुष्प्रभाव या लक्षण हैं, जैसे कि एक निश्चित चिकित्सा स्थिति, अन्य नींद संबंधी विकार, या कुछ दवाएं। शराब, तंबाकू और कैफीन जैसे पदार्थ भी इस स्थिति का कारण बन सकते हैं। कभी-कभी पुरानी अनिद्रा प्राथमिक होती है, जिसका अर्थ है कि किसी अन्य स्थिति के कारण यह नहीं हुई है। अनिद्रा के लक्षण इस स्थिति के प्रमुख लक्षणों में शामिल हैं: थकान दिन के समय नींद आना याददाश्त और एकाग्रता की समस्या चिड़चिड़ापन दीर्घकालिक तक अनिद्रा निम्नलिखित लक्षण पैदा कर सकता है: सोने में कठिनाई होना आधी रात में जागने के बाद वापस सोने में कठिनाई होना अवसाद चिड़चिड़ापन स्कूल, काम या सामाजिक प्रदर्शन में परेशानी प्रेरणा की कमी तंद्रा गलतियों या दुर्घटनाओं में वृद्धि व्यवहार संबंधी समस्याएं जैसे आक्रामकता या अतिसक्रियता नींद से असंतोष या चिंता सोने के बाद तरोताजा महसूस न होना अनिद्रा के कारण नींद में खलल डालने वाली आदतों या जीवन की घटनाओं के साथ-साथ तनाव अनिद्रा के सबसे आम कारणों में से एक है। अनिद्रा के कारण का इलाज करने से समस्या का समाधान हो सकता है, लेकिन इसमें वर्षों लग सकते हैं। अनिद्रा के सबसे आम कारणों में शामिल हैं: तनाव: स्कूल, काम, वित्त, परिवार और स्वास्थ्य के बारे में चिंताएँ आपको रात में सोने से रोक सकती हैं। किसी परिचित व्यक्ति की बीमारी या मृत्यु, नौकरी छूटना या तलाक जैसी आघात और तनावपूर्ण जीवन की घटनाएं भी अनिद्रा का कारण बन सकती हैं। कार्य या यात्रा कार्यक्रम: आपकी सर्कैडियन लय आपकी आंतरिक घड़ी है जो आपके चयापचय, शरीर के तापमान और नींद-जागने के चक्र को निर्देशित करती है। आपके शरीर की सर्कैडियन लय में गड़बड़ी भी अनिद्रा का कारण बन सकती है। सर्कैडियन लय व्यवधान के महत्वपूर्ण कारणों में जल्दी या देर की पाली में काम करना, बार-बार पाली बदलना और विभिन्न समय क्षेत्रों में यात्रा करना शामिल है। देर शाम ज़्यादा खाना: सोते समय हल्का नाश्ता करना ठीक है, लेकिन शाम को अधिक खाने से लेटने पर आपको शारीरिक रूप से असहजता महसूस हो सकती है। खाने के बाद आपको भोजन और एसिड का पेट से अन्नप्रणाली में वापस प्रवाह और सीने में जलन का भी अनुभव हो सकता है जो आपको जगाए रख सकता है। ख़राब नींद की आदतें: सोते समय उत्तेजक गतिविधियाँ जैसे; अनियमित सोने का समय; असहज नींद का माहौल; खाने के लिए अपने बिस्तर का उपयोग करना, टीवी देखना और काम करना, और झपकी लेना नींद की खराब आदतें हैं जो समय के साथ अनिद्रा का कारण बन सकती हैं। सोने से पहले वीडियो गेम खेलना या टीवी, कंप्यूटर और स्मार्टफोन का उपयोग करना भी आपके नींद के चक्र को बाधित कर सकता है। अन्य सामान्य अनिद्रा कारणों में शामिल हैं: मानसिक स्वास्थ्य समस्याएं: अवसाद, चिंता और अभिघातजन्य तनाव विकार जैसी अन्य मानसिक स्वास्थ्य समस्याएं नींद में खलल डाल सकती हैं और बाधित कर सकती हैं। चिकित्सीय स्थितियाँ: अनिद्रा से जुड़ी सामान्य चिकित्सीय स्थितियों में कैंसर, पुराना दर्द, हृदय रोग, मधुमेह, अस्थमा, अतिसक्रिय थायरॉय्ड, अल्जाइमर रोग, जीईआरडी या गैस्ट्रोएसोफेगल रिफ्लक्स रोग और पार्किंसंस रोग शामिल हैं। दवाएँ: विभिन्न नुस्खे वाली दवाएँ भी आपके प्राकृतिक नींद चक्र को बाधित कर सकती हैं। इनमें रक्तचाप या अस्थमा की दवाएं और अवसादरोधी दवाएं शामिल हैं। दर्द, एलर्जी और सर्दी के लिए कई ओवर-द-काउंटर दवाएं और वजन घटाने वाले उत्पाद भी कैफीन की मात्रा के कारण नींद में पड़ सकता है। शराब, निकोटीन और कैफीन: कोला, चाय, कॉफी और अन्य कैफीनयुक्त पेय पदार्थ उत्तेजक हैं जो देर शाम या दोपहर में लेने पर आपकी नींद में खलल डाल सकते हैं। तम्बाकू में निकोटीन होता है जो एक उत्तेजक भी है जो आपकी नींद में खलल डाल सकता है। शराब नींद लाती है लेकिन गहरी नींद के चरणों को रोकती है और आधी रात को जागने का कारण बनती है। नींद से संबंधित स्थितियां: रेस्टलेस लेग सिंड्रोम और उन्हें हिलाने की इच्छा के कारण आपको पैरों में असहजता महसूस हो सकती है, जो आपको उचित नींद लेने से रोक सकती है। स्लीप एपनिया एक और स्थिति है जो आपको रात भर समय-समय पर सांस लेने में बाधा डालती है, जिससे नींद में खलल पड़ता है। अनिद्रा का इलाज तीव्र या अल्पकालिक अनिद्रा अपने आप ठीक हो जाती है। क्रोनिक अनिद्रा उपचार में शामिल हैं: नींद की स्वच्छता शिक्षा: यह आपको उचित व्यायाम और आहार के माध्यम से एक स्वस्थ जीवन शैली विकसित करने में मदद कर सकता है। एक डॉक्टर अनिद्रा के उपचार, इसके कारणों और लक्षणों और उन तनावों के बारे में जानकारी प्रदान कर सकता है जो नींद न आने का कारण बन सकते हैं। आप शोर, रोशनी, गद्दे और तापमान जैसे पर्यावरणीय कारकों को कम करने के विभिन्न तरीकों के बारे में भी जान सकते हैं जो आपकी नींद में खलल डाल सकते हैं। संज्ञानात्मक व्यवहार थेरेपी: थेरेपी में उत्तेजना नियंत्रण शामिल है, जिसका उद्देश्य नींद के बारे में गलत धारणाओं को बदलना है। थेरेपी उन क्रियाओं का भी सुझाव देती है जो नींद को ट्रिगर कर सकती हैं, जैसे: दिन के समय झपकी लेने से बचें नींद आने पर ही बिस्तर पर जाएं शयनकक्ष का उपयोग केवल सोने के लिए करें नियमित रूप से कम से कम 20 मिनट तक व्यायाम करें, लेकिन बिस्तर पर जाने से 4 से 5 घंटे पहले। नियमित जागने और सोने की दिनचर्या बनाए रखना रात के समय शीतल पेय और कॉफी जैसे कैफीनयुक्त पेय पदार्थों से बचें। अपने शयनकक्ष में सोने का उत्तम वातावरण बनाएं। शोर, तापमान पर काम करना और उच्च तीव्रता वाली रोशनी के उपयोग से बचें। नींद प्रतिबंध थेरेपी: इसमें आपके बिस्तर पर बिताए जाने वाले समय को सीमित करना शामिल है,और यह दिन में अत्यधिक नींद आने से रोकता है और जल्दी नींद आने को प्रेरित करता है। व्यवहारिक हस्तक्षेप: इससे आपको चिंता करने और बिस्तर पर पड़े रहने जैसे नींद के साथ असंगत व्यवहारों को दूर करते हुए अच्छी नींद की स्वच्छता अपनाने में मदद मिल सकती है। विश्राम उपचार: बायोफीडबैक तकनीक और प्रगतिशील मांसपेशी छूट जैसे उपचार उत्तेजना को कम कर सकते हैं। एकाग्रता और कल्पनाशीलता को प्रशिक्षित करने से सोने से पहले संज्ञानात्मक सतर्कता को कम करने में भी मदद मिल सकती है। ये प्रक्रियाएँ तनाव के कारण होने वाली नींद में बाधा से निपटने में भी आपकी मदद कर सकती हैं। औषधियाँ: बेंज़ोडायजेपाइन, ज़ेलप्लॉन, ज़ोलपिडेम और ज़ोपिक्लोन, रामेलटेओन, एस्ज़ोपिक्लोन, टीसीए या ट्राइसाइक्लिक एंटीडिप्रेसेंट्स और एंटीहिस्टामाइन जैसी दवाएं हार्मोनल असंतुलन में सुधार और अंतर्निहित मनोवैज्ञानिक स्थितियों का इलाज करके नींद की कमी को कम कर सकती हैं। निष्कर्ष नींद आपके स्वास्थ्य के लिए नियमित व्यायाम और संतुलित आहार जितनी ही महत्वपूर्ण है। नींद न आने का कारण चाहे जो भी हो, अनिद्रा आपको शारीरिक और मानसिक दोनों तरह से प्रभावित कर सकती है। किसी विशेषज्ञ से संपर्क करना सबसे अच्छा है। वे आपकी नींद में खलल डालने वाली समस्याओं को प्रबंधित करने में आपका मार्गदर्शन करेंगे।
 Home Visit
Home Visit Upload
Upload


















 WhatsApp
WhatsApp