Latest Blogs
Heart Attack Testing- Are You at Risk?
A heart attack occurs when the heart does not receive adequate blood flow due to blockage in the blood vessels. Accumulation of fat, cholesterol, and other substances cause blockage. Plaque buildup in the artery is known as atherosclerosis. If this plaque ruptures, it can form clots that block the blood flow within the heart. Impaired blood flow destroys parts of the heart muscle and leads to a heart attack. A heart attack is usually of two types: STEMI (ST-elevation-Myocardial Infarction) and Non-STEMI. A STEMI is associated with abnormality in the ECG wave in which the ST segment appears higher than in a normal ECG wave; it occurs due to complete blockade of blood supply to the heart for a prolonged time. A Non-STEMI heart attack usually occurs when the heart does not get required oxygen due to severe narrowing of arteries or transient occlusion. Heart Attack causes and Risk Factors Coronary artery disease is a leading cause of heart attack. Other reasons for heart attack are: Lack of oxygen in the blood Drug misuse Spasms within the blood vessels Tearing of blood vessels The Risk Factors for Developing a Heart Attack are: Age Diet-related factors Obesity High cholesterol Smoking and alcohol consumption Stress Sleeping problems Diabetes, prediabetes Heart Attack Symptoms The common heart attack symptoms are: Chest pain, discomfort Nausea Shortness of breath Severe pain in the arm or shoulder Sweating Fatigue Lightheadedness Pain in the upper body and jaw. Difficulty breathing What Happens During and After a Heart Attack? A heart attack lowers the blood and oxygen flow to the heart. Abnormal rhythms are developed in the heart. Some heart tissues can die due to the lack of blood and oxygen. It can weaken the heart, leading to heart failure. It can affect the functioning of the heart valves. Heart Attack Diagnosis Blood pressure, pulse are measured to assess the heart’s functioning and overall cardiac health. Following a heart attack, an electrocardiogram (ECG or EKG) is usually done to check for damage to the heart muscle. A doctor may also ask for a chest x-ray to see if the heart is enlarged or if there is fluid buildup around the lungs. Let's understand this in detail: Electrocardiogram (ECG or EKG) An ECG test measures the heart’s electrical activity. An ECG can find problems with the heart's muscles and valves, and monitor its rhythm. Sticky patches (electrodes) are placed on the chest, arms, and legs to record signals as waveforms, viewed on a screen or printed on paper. Being the first heart attack diagnosis test, an ECG is a simple, painless test that takes just a few minutes. It helps diagnose heart conditions, such as a heart attack, congestive heart failure or an irregular heartbeat. Chest x-ray A chest x-ray uses electromagnetic energy beams to produce images of the structures within the chest. It is generally safe and has very low radiation exposure. It is not recommended for pregnant women and young children as they are more sensitive to radiation effects. Blood tests A blood test for heart attack diagnosis is often done to check for troponin, a protein released into the bloodstream when the heart is damaged. A doctor may ask for blood tests to check for enzymes released when heart muscle cells die. Cardiac injury profiles are a group of blood tests that measure the levels of various components in blood that are usually affected during a heart attack. Troponin I and CK-MB being the tests of choice. Imaging Tests These tests include a computed tomography (CT) scan, magnetic resonance imaging (MRI), echocardiogram and nuclear stress test. Echocardiogram An echocardiogram (echo) test uses ultrasound waves to create images of your heart. A doctor can use the echo to evaluate the heart’s structure and functioning. It can also help diagnose problems with the heart’s muscles or valves. Non-STEMI heart attack diagnosis Non-stemi heart attack diagnosis is made using blood tests, imaging tests and electrocardiograms. The blood test detects indicators of Non-STEMI, such as elevated creatine kinase-myocardial band (CK-MB), troponin, myoglobin, and lactate dehydrogenase (LDH). Imaging tests such as an echocardiogram, cardiac MRI, computed tomography angiography (CTA) or coronary angiogram are done to look for artery blockages. An electrocardiogram may also be done to check for changes in the heart's electrical activity that can occur with Non-STEMI. Getting a heart attack diagnosis is important if any symptom occurs, as early treatment can save your life. Heart Attack Treatment Heart attack treatment aims to correct the blood flow within the heart and restore oxygen levels in the blood. The following treatment methods can help a heart attack patient: Medications Clot busters Blood thinning medicines Pain relievers Nitroglycerin Blood-pressure lowering medicines Cholesterol-lowering drugs Surgical Procedures Coronary artery bypass surgery Coronary angioplasty and stenting Pacemaker Valve repair or replacement surgery Cardiac Rehabilitation (rehab) Exercise and education programme to improve heart health after surgery. Alternative Treatments Lifestyle modifications Heart-healthy diet It is crucial to receive treatment for heart attack at the right time. The sooner you receive medical help after suffering a heart attack, the more successful your therapeutic outcomes are likely to be. Complications A heart attack can be life-threatening. It affects your heart health and its functioning in the long term. Heart Attack Prevention Your lifestyle, especially food and exercise, is your best weapon against heart disease and stroke. The following are some of the suggestions for a healthy heart: Quit Smoking and Alcohol Smoking and alcohol consumption increases the risk factors for heart attack. Quitting smoking and alcohol is the best thing you can do for your heart. Eat a Healthy Diet Eating a diet high in fruits, vegetables, whole grains, and low in saturated and trans fats can help reduce heart disease and stroke risk. Get Active Just 30 minutes of moderate-intensity exercise can help reduce your risk of heart disease and stroke. Manage your Blood Pressure If you have high blood pressure, working with your doctor to manage it can help reduce the risk of a heart attack. Manage your Cholesterol If you have high cholesterol, taking steps to manage it can help reduce the risk of a heart attack. Manage your Diabetes If you have diabetes, consult your doctor to manage your diabetes to reduce the risk of a heart attack. Reduce Stress Effective stress management can help you reduce the risk of a heart attack. Know your Family History A family history of heart diseases can impact your cardiac health. Knowing your family history is important for your doctor to best manage your health. Regular Checkups Regular medical checkups can help identify health problems early when they are easier to treat. Lipid profile assessment, cardiac risk assessment , diabetes risk profile are some tests that may be done as per the doctor’s recommendation. Conclusion Identifying and preventing the risk of a heart attack is essential. Your age, lifestyle, and pre-existing medical conditions determine your risk of suffering a heart attack. It would be best to seek preventive measures immediately to eliminate or minimise these risks.
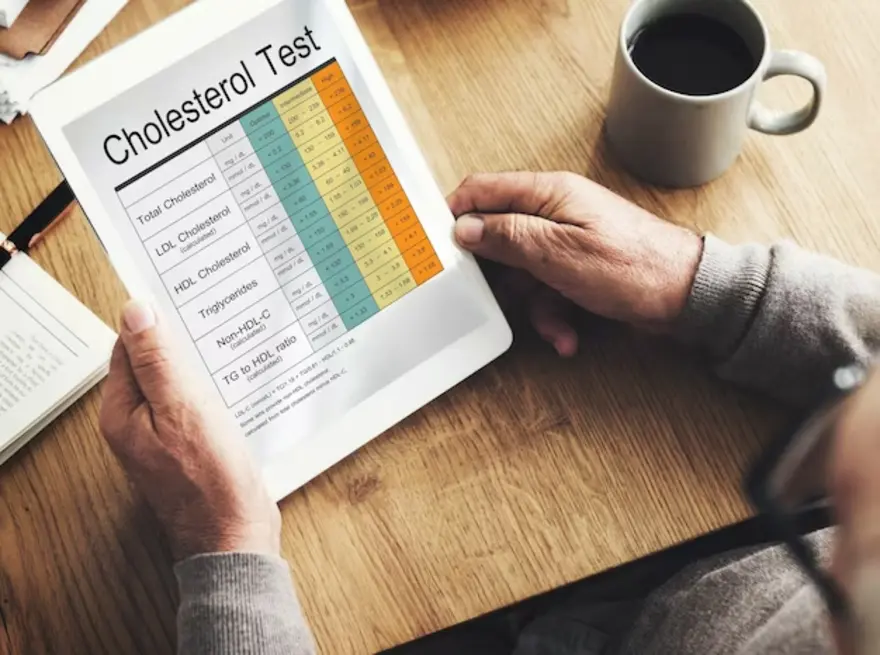
Cholesterol Levels - What You Need to Know
Cholesterol is a waxy substance found in your body and certain foods. It plays a crucial role in various bodily functions, but too much "bad" cholesterol (LDL) can increase the risk of heart disease. "Good" cholesterol (HDL) helps remove excess LDL. Managing cholesterol levels through a healthy lifestyle, diet, and, if necessary, medication is vital for heart health. Read more to know about other factors of Cholesterol and the required total cholesterol normal value. You will also learn about the other cholesterol values in the body. What is meant by Cholesterol? Cholesterol is a waxy, fat-like substance that's found in all the cells in your body. Your body needs cholesterol to make hormones, vitamin D, and substances that help you digest foods. Your body makes all the cholesterol it needs but you also get extra cholesterol from the foods you eat. Your body has a system for getting rid of excess cholesterol but too much cholesterol in your blood can raise the risk of heart disease and stroke. This is because cholesterol can build up in the walls of your arteries, forming plaques. These plaques can narrow or block your arteries, making it difficult for blood to flow to your heart and brain. How do you measure cholesterol levels? Cholesterol levels are measured with a blood test called a Lipid Panel. This test measures LDL cholesterol, HDL cholesterol, triglycerides, and total cholesterol range in your blood. To prepare for a lipid panel, you must fast for 9-12 hours before the test. This means not eating or drinking anything but water during that time. During the test, a healthcare professional will draw blood from a vein in your arm. The blood will be sent to a laboratory for analysis. Your lipid panel results will be available within a few days. Your doctor will review your results and discuss any necessary lifestyle changes or medications. Here are the steps involved in measuring cholesterol levels: Fast for 9-12 hours before the test. Have a blood sample drawn from a vein in your arm. Send the blood sample to a laboratory for analysis. Review the results with your doctor. What are the types of cholesterol? There are two main types of cholesterol: Low-density lipoprotein (LDL) cholesterol: LDL cholesterol is known as "bad" cholesterol because it can build up in the walls of your arteries. It can lead to hardening of the arteries (atherosclerosis), which can increase the risk of heart disease and stroke. The LDL normal value is less than 100 mg/dL (3.4mmol/L). High-density lipoprotein (HDL) cholesterol: HDL cholesterol is known as "good" cholesterol because it helps to remove LDL cholesterol from the arteries. This helps to keep the arteries clear and reduces the risk of heart disease and stroke. The HDL normal value is 40 mg/dL (1mmol/L) or more. There are other types of cholesterol listed below- Very low-density lipoprotein (VLDL) cholesterol: VLDL cholesterol is a type of fat made in the liver and released into the bloodstream. VLDL cholesterol is converted to LDL cholesterol in the bloodstream. Intermediate-density lipoprotein (IDL) cholesterol: IDL cholesterol is formed when VLDL cholesterol loses some of its triglycerides. IDL cholesterol can be converted to LDL cholesterol or HDL cholesterol. Lp(a) cholesterol: Lp(a) cholesterol is a type of cholesterol that is similar to LDL cholesterol, but it has an additional protein attached to it. Lp(a) cholesterol can build up in the walls of the arteries and increase the risk of heart disease and stroke. What do your cholesterol numbers mean? Your cholesterol numbers can help you understand your risk of heart disease and stroke. The four main cholesterol numbers are: Total cholesterol: This is the total amount of cholesterol in your blood. LDL cholesterol: This is the "bad" cholesterol that can build up in your arteries and form plaques. HDL cholesterol: This is the "good" cholesterol that helps remove LDL cholesterol from your arteries. Triglycerides: This is another type of fat in your blood that can raise your risk of heart disease and stroke. Here is a breakdown of what your cholesterol numbers mean: Total cholesterol range- Average: Less than 200 milligrams per deciliter (mg/dL) Borderline high: 200-239 mg/dL High: 240 mg/dL and higher LDL cholesterol range- Optimal: Less than 100 mg/dL Near-optimal: 100-129 mg/dL Borderline high: 130-159 mg/dL High: 160-189 mg/dL Very high: 190 mg/dL and higher HDL cholesterol range- Low: Less than 40 mg/dL in men and less than 50 mg/dL in women Ideal: 60 mg/dL or higher in men and 55 mg/dL or higher in women Triglycerides range- Normal: Less than 150 mg/dL Borderline high: 150-199 mg/dL High: 200-499 mg/dL Very high: 500 mg/dL and higher What is the normal serum cholesterol level? Total cholesterol normal value for adults: Less than 200 mg/dL LDL cholesterol normal range value: Less than 100 mg/dL HDL cholesterol normal range value: 40 mg/dL or higher Triglycerides: Less than 150 mg/dL How often should you get your cholesterol checked? The frequency with which you should get your cholesterol checked depends on your age and risk factors for heart disease and stroke. The American Heart Association recommends that adults aged 20 or older have their cholesterol checked every four to six years. However, if you have any of the following risk factors, you may need to get your cholesterol checked more often: Age 45 or older (men) or 55 or older (women) Family history of heart disease or stroke High blood pressure Diabetes Smoking Obesity High triglycerides Low HDL cholesterol Suppose you have other risk factors for heart disease, such as high cholesterol, low HDL cholesterol, or high triglycerides. In that case, your doctor may recommend checking your cholesterol even more often. It is also essential to talk to your doctor about how often you should check your cholesterol if you take any medications affecting cholesterol levels, such as statins or niacin. What affects your cholesterol levels? Your cholesterol levels are affected by several factors, including: Unhealthy Diet: Eating high in saturated and trans fats can raise cholesterol levels. Saturated fats are found in animal products, such as red meat, butter, and full-fat dairy products. Trans fats are found in processed foods, such as fried foods and baked goods. It is essential to eat a diet that is low in saturated and trans fats and high in fruits, vegetables, and whole grains. Lack Of Exercise: Exercise can help lower your cholesterol levels. Aim for at least 30 minutes of moderate-intensity exercise most days of the week. Weight: Being overweight or obese can raise your cholesterol levels. Losing weight can help lower your cholesterol levels. Smoking: Smoking can raise your LDL cholesterol value levels and lower your HDL cholesterol value levels. Quitting smoking can help improve your cholesterol levels. Medical conditions: Certain medical conditions, such as diabetes, high blood pressure, and kidney disease, can raise cholesterol levels. Medications Consumed: Certain medications, such as statins and niacin, can raise cholesterol levels. Age: As you get older, the LDL cholesterol range by age changes and levels tend to rise. Gender: Men people tend to have higher LDL and lower HDL cholesterol levels than women. Normal cholesterol levels for women may be different. Genetics: Your cholesterol levels can also be affected by your genes. How can you lower your cholesterol? Eat a healthy diet: This means eating a diet low in saturated and trans fats and high in fruits, vegetables, and whole grains. Saturated fats are found in animal products, such as red meat, butter, and full-fat dairy products. Eat fruits, vegetables, whole grains, beans, lentils, nuts, seeds, fish, olive oil, and avocados. Exercise regularly: Aim for at least 30 minutes of moderate-intensity exercise most days. Exercise can help raise your HDL cholesterol levels and lower your LDL cholesterol levels. It can also help you maintain a healthy weight. Perform walking, running, biking, swimming, dancing, and gardening. Maintain a healthy weight: Being overweight or obese can raise your cholesterol levels. Losing weight can help lower your cholesterol levels. Even a tiny amount of weight loss can make a difference. Quit smoking: Smoking can raise your LDL cholesterol levels and lower your HDL cholesterol levels. Quitting smoking can help improve your cholesterol levels and reduce your risk of heart disease and stroke. Manage other medical conditions: If you have other medical conditions, such as diabetes, high blood pressure, or kidney disease, it is vital to manage them carefully. These conditions can raise your cholesterol levels, so managing them can help lower your cholesterol levels and reduce your risk of heart disease and stroke. Conclusion It is important to have your cholesterol levels checked regularly, especially if you have any risk factors for heart disease and stroke. If your cholesterol levels are high, talk to your doctor about how to lower them. With lifestyle changes and medication, you can lower your cholesterol levels and reduce your risk of heart disease and stroke. To learn more about how you check your cholesterol level, you can contact Metropolisindia’s professionals. They will provide you with the convenience of testing at home and the benefit of accurate test results
Lipid Disorders: What Are They And How Can I Treat Them?
Introduction Do you have a lipid disorder, or are you at risk for one? People with high cholesterol or triglycerides have a lipid disorder. A lipid is a type of fat found in your blood. Lipid disorders are common, but many people don't know they have one. High cholesterol and triglycerides can lead to heart disease, stroke, and other problems. However, you can take steps to lower your risk. This blog will discuss the causes, symptoms, and treatment of lipid disorders. What is a Lipid Disorder? Lipid disorders are conditions that prevent the body from properly metabolising fats. As a result, it can accumulate harmful fats in the blood, increasing the risk for heart disease, stroke, and other serious health problems. However, with proper treatment, many people with lipid disorders can manage their condition and live healthy lives. To the untrained eye, it might seem like all fats are the same. However, there are several different types of fats, each impacting the body differently. You should know the difference between these fats to make informed decisions about your diet and lifestyle. What are The Causes of Lipid Disorder? The causes of lipid disorders vary depending on the type of disorder. In general, however, these conditions are caused by an imbalance in how the body metabolises fats. In addition, it can be due to genetic factors, lifestyle choices, or other underlying health conditions. Some of the most common causes of lipid disorders include: High cholesterol: This is one of the most common causes of lipid disorders. Cholesterol is a type of fat found in the blood. Too much cholesterol can lead to a buildup of plaque in the arteries, which can increase the risk for heart disease, stroke, and other problems. High triglycerides: Triglycerides are another type of fat found in the blood. Like cholesterol, too many triglycerides can lead to plaque buildup in the arteries. It can increase heart disease, stroke, and other problems. Obesity: Obesity is a major risk factor for lipid disorders. People who are obese are more likely to have high cholesterol and triglycerides. Obesity can also lead to other health problems, such as diabetes, which can further increase the risk for lipid disorders. Unhealthy diet: A diet high in saturated and trans fats can increase the risk for lipid disorders. These types of fats can raise cholesterol and triglyceride levels. Lack of exercise: A sedentary lifestyle can also increase the risk for lipid disorders. Exercise helps to improve cholesterol and triglyceride levels. Smoking: Smoking is a major risk factor for lipid disorders. Tobacco smoke contains harmful chemicals that can damage the arteries and raise cholesterol and triglyceride levels. Family history: If you have a family history of lipid disorders, you may be at increased risk for these conditions. Diabetes: Diabetes is a condition that can lead to lipid disorders. People with diabetes are more likely to have high cholesterol and triglycerides. Kidney disease: Kidney disease can also lead to lipid disorders. It is because the kidneys play a role in cholesterol and triglyceride metabolism. What are The Symptoms of Lipid Disorder? Lipid disorder symptoms vary depending on the type of disorder. In general, however, these conditions can cause a variety of problems. Some of the most common symptoms of lipid disorders include: Atherosclerosis is a common complication of lipid disorder. It is when your arteries harden and narrow, and it can lead to a heart attack or stroke. Angina pectoris at rest and exertion (pressing pain, burning sensation in the heart region at rest or during physical work) can also be a symptom of lipid disorders. Other lipid disorder symptoms include sudden dizziness, noise and buzz in the ears, memory impairment, and a sharp decrease in concentration. Some people feel pain in the legs when walking. It can also be a symptom of lipid disorders. Fat deposits are formed in the skin (xanthoma) or the eyelid area (xanthelasma). If you have any of these symptoms, it's important to see your doctor so they can run some tests and determine if you have a lipid disorder. Lipid disorders are often detected by blood tests for lipid screening. This may be a part of Lipid Profile screening , Cardiac Risk Assessment or as part of regular whole body check up. Regular blood glucose level testing for Diabetes mellitus is also recommended as its a precursor for lipid disorders. . Apart from these, some specific tests are also used to detect lipid disorders.These include:: Biochemistry of blood and measuring lipid metabolism will give your doctor an idea of your current state and can start to see the effects of treatment. Determination of the coefficient of atherogenicity - determination of the ratio of high and low-density lipoproteins. Ultrasonic duplex scanning of colour vessels using an ultrasound machine. With its help, the doctor determines the foci of poor circulation and compares the blood flow in paired organs. Magnetic resonance angiography - allows you to evaluate the anatomical and functional features of blood flow. Computed angiography is used to visualise large blood vessels and identify their pathological changes. Treatment for Lipid Disorder With lifestyle changes, medications, and regular screening one can often manage the lipid disorders. Conclusion Not all tests and methods are required. They are prescribed at the doctor's discretion and in the absence of contraindications. The treatment of lipid disorders aims to reduce the risk of atherosclerosis and its complications. To do this, you need to normalise your lifestyle and take medications. For example, it would help if you quit smoking, lead an active lifestyle, and eat right. In addition to diet and physical activity, you need to take drugs that lower cholesterol. These include statins, fibrates, niacin, and other drugs. The choice of drug and dosage is determined by the doctor individually.
Rheumatoid Arthritis Self-Care - Tips for Diagnosis & Managing the Disease
Rheumatoid Arthritis is a chronic disease of the immune system. It is an autoimmune disease where your body’s immune cells attack the lining of the joints, known as synovium. The causes for this condition are attributed to genetic factors and environmental triggers. An inflammatory process characterises Rheumatoid Arthritis in the synovium throughout your body. Your immune system is designed to fight bacteria and other foreign invaders that may cause harm to your body. In Rheumatoid Arthritis, the immune system mistakes the cells of the synovium as a foreign invader and begins attacking this lining of the joints. The synovium produces a fluid that helps the joint move smoothly. But as the cells of the immune system attack it, there is inflammation in these cells, leading to the eventual destruction of the cartilage and bone elements of the joint. As a result, one can experience pain, stiffness, and weakness, among other symptoms. The duration of these symptoms varies from one person to another. For some, the symptoms may be aggressive and progress rapidly. For others, it may take several years. There might also be instances where patients experience a period of time with symptoms (flare) and some with no symptoms (regression). What are The Symptoms of Rheumatoid Arthritis? The intensity of symptoms experienced varies over the different stages of Rheumatoid Arthritis. In the early stages, the symptoms include, Joint stiffness lasts for extended periods, such as half an hour. Experience stiffness in the same joints on both sides of the body. Unexplained pain, swelling and tenderness in smaller joints or multiple joints simultaneously. Fatigue and weakness. Symptoms and discomfort that last longer than six weeks. How is Rheumatoid Arthritis Diagnosed? In the earlier stages, the symptoms of Rheumatoid Arthritis may be similar to other types of arthritis. No singular, gold standard test determines the diagnosis of Rheumatoid Arthritis. Hence, the examination for diagnosing consists of a combination of physical and blood tests. ● Physical Examination The doctor or physician checks the joints for swelling or tenderness. The range of motion is also checked across different joints. During the physical examination, you may be asked about symptoms and your medical and family history for any genetic influences and instances of Rheumatoid Arthritis in relatives. ● Blood Examination Post the physical examination, blood tests are conducted to identify any forms of inflammation and autoantibodies that may indicate Rheumatoid Arthritis. The blood tests may include, Rheumatoid factor (RF) test and CCP antibody test (anti-cyclic citrullinated peptide)–. You can take a CCP Antibody test to distinguish it from other types of Arthritis. CCP antibody test is more specific and has less false positives in comparison to RF Erythrocyte sedimentation rate and C reactive protein – higher levels of these tests may indicate the condition. These are non-specific markers of inflammation Antinuclear antibodies – a positive or negative test helps with diagnosis. Complete blood count (CBC) -- is recommended when the doctor finds low red blood cells, an indicator of Rheumatoid Arthritis. ● Imaging Tests In combination with blood tests, imaging tests reveal the diagnosis and progression of the disease such that the doctor can monitor and provide treatment accordingly. The imaging tests recommended include, X-rays showcase the amount of joint damage. Ultrasound and Magnetic Resonance Imaging (MRI) to provide more details on the condition of the joints. These tests can show if the ends of the bones are slowly eroding over time due to inflammation. Imaging tests are also used between treatments to check the progress and results of medications and treatment. How is Rheumatoid Arthritis treated? There is no specific cure for the disease, but early investigations, diagnosis and medications can help keep symptoms under control. The inflammation can be reduced or stopped, and doctors can prescribe medications to relieve symptoms' remission. Treatment in Rheumatoid Arthritis usually involves medication such as disease-modifying anti-rheumatic drugs. Steroids -- Corticosteroids such as Prednisone help reduce inflammation and pain and slow joint damage. Conventional DMARDs -- are intended to slow the progression of rheumatoid arthritis and save the joints from permanent damage. They are used along with biologic response modifiers, such as methotrexate. Targeted synthetic DMARDs -- these are used when conventional and biological response modifiers do not work. Over-the-counter NSAIDs -- Non-steroidal Anti-Inflammatory Drugs can relieve pain and reduce inflammation during treatment. Therapy The doctor may refer you to a physical or occupational therapist to engage in exercises that can help keep the joint flexible. These modifications are also suggested to one’s daily activities to make them more manageable. For instance, helpful equipment and assistive devices can help you get dressed, get a better grip on holding objects, and so on. Surgery Surgery is often the last resort for rheumatoid arthritis when the medications fail to prevent or slow joint damage. The types of surgery that can reduce pain and improve function include, Tendon repair -- targeted to repair the tendons around the joint that have been loosened or ruptured due to inflammation. Total joint replacement -- the damaged parts of the joints are replaced by prosthetic parts. Synovectomy -- aimed to remove the synovium, the inflamed lining of the joints, to reduce pain and improve flexibility. Joint fusion -- only in cases where replacement is impossible, joint fusion is conducted to relieve pain and stabilise or realign a joint. Discussing the pros and cons of surgery before undertaking the procedure is crucial. Ensure that you are informed of all procedures before and after surgery. Other Forms of Self-Care to Manage Rheumatoid Arthritis While medications and treatment are essential, you can also contribute to your recovery by managing diet and lifestyle choices to control rheumatoid arthritis. Eating healthier, being involved in daily movement such as light walking, proper rest, and using heat treatments to relieve joint pain can help. A diet with Rheumatoid Arthritis may include supplements such as omega-3 fish oil and eliminating habits such as smoking, intake of junk food, and so on. Such habits can contribute to preventing and reversing the effects of rheumatoid arthritis in the long run. Consulting the doctor and therapists on recovery methods and cultivating a positive support system and environment are complementary in the recovery process from Rheumatoid arthritis.
Tips on how to prevent heart disease
1. Go for a heart-healthy diet Experts have concluded that people who follow the right food habits have more than 30% lower risk of heart disease. What is the most-recommended heart-healthy diet? Taking a low-calorie but nutrient-rich food is important. Avoid foods like cakes, biscuits, sausages, pudding, butter, red meat, cheese, fatty dairy products, pasta, bacon, etc. These have high saturated content. Include plenty of fruits, vegetables, whole grains, fish, low-fat dairy products, and nuts in your diet. Include low-fat proteins like yogurt, legumes, skinned poultry, and soy products. Reduce the intake of salt. Limit or avoid canned soups, ketchup, mayonnaise, tomato sauce, soy sauce, etc. How much you eat is as important as what you eat. So, control the portion size of the food you eat. Based on the above recommendations, plan daily menus to make sure that you have a well-balanced diet. 2. Exercise regularly Exercising regularly is one of the major steps to avoid heart attack and keep your heart healthy. It is recommended to be physically active to avoid heart ailments.There are three types of exercises that are very effective in preventing cardiac conditions:. Aerobic exercises like running, cycling, brisk walking, swimming, and skipping help to increase the blood circulation. Exercising also helps to lower the blood pressure and decreases the risk of type 2 diabetes. Resistance training like dumbbells, pushups, resistance bands,, and other such exercises help reduce the LDL also known as “bad cholesterol”. It also reduces body fat, one of the major culprits of heart disease. Body-stretching exercises like yoga and Tai-Chi not only lay a good muscular and skeletal foundation, but also help to reduce stress and anxiety. Although these three physical activities are highly recommended, you can do any physical activity that you like. It could be dancing, jogging or playing a favourite sport like tennis and football. Regular physical activity will surely reduce the chances of heart disease. They are the best tools for cardiovascular disease prevention. 3. Live a tobacco-free life Tobacco control is one of the key elements in preventing heart disease. This is because tobacco increases the risk of heart attack by Damaging lungs Clogging arteries Increasing blood clots, Weakening your immunity Increasing inflammation Moreover, carbon monoxide that enters your bloodstream decreases the oxygen supply to all organs and tissues. It also narrows the blood vessels and increases the blood pressure and heart rate. As a result, your heart is forced to pump blood faster than usual. What happens when you quit smoking? Research has proven that your blood pressure decreases in a day, and blood circulation improves in a couple of weeks after you stop smoking. In a few months, your cough will disappear. In a year, the risk of heart disease reduces by 50%. Live a tobacco-free life to keep your heart healthy. 4. Limit alcohol consumption Several studies have shown that people who took less than two drinks daily had a 20% less risk of heart disease. Heavy drinking can increase the risk of: Elevated Blood pressure Irregular heart rhythm Obesity A disorder in the heart muscle called cardiomyopathy Heart failure Moderate drinking (two drinks for men and one for women) will decrease the risk of heart disease. Limit consumption of alcohol to lower the risk of heart disease. 5. Reduce stress Stress leads to the release of a hormone called cortisol. Cortisol can increase the blood sugar, blood pressure, triglycerides, inflammation, bad cholesterol, and decrease the blood flow to the heart muscles. All these are common risk factors that trigger heart diseases. So you should reduce stress by: Exercising regularly Following relaxing strategies like yoga and meditation Having a hobby that can relax you Being positive Spending time with family and friends Enjoy a stress-free life as it is a precaution against a heart attack. 6. Keep your blood pressure under control Excessive blood pressure narrows the arteries supplying blood to the heart due to the build-up of cholesterol and fat. The hardening of arteries leads to the formation of blood clots. This results in an interruption in the flow of oxygen and nutrients to the heart muscles, and ultimately causes a heart attack. So, it is important to keep your blood pressure under control. To control blood pressure, you have to Sleep well Avoid stress Be physically active Reduce sodium intake and Drink less alcohol. 7. Keep diabetes under control How does diabetes increase the risk of heart disease? It damages the cardiovascular nerves and blood vessels. High sugar levels can also damage your arterial walls. The risk of formation of plaque in the blood vessels is high. It can also increase triglycerides. In cases of known diabetics, it is recommended to get the blood glucose (fasting and postprandial) as well as the HbA1c levels tested at periodic intervals. It is also recommended to test the cholesterol and triglyceride levels regularly as they are closely linked with diabetes. How to keep diabetes under control? Be active. Follow the right meal plan. Check blood sugar levels as directed by the physician. Take the prescribed medications. People in the prediabetes range are also at risk for heart diseases. Hence, they should also follow the necessary precautions. It is recommended to monitor the HbA1c levels and lipid profiles at least annually. 8. Keep your triglycerides and cholesterol under control Cholesterol can be in the form of HDL or LDL. HDL or High-Density Cholesterol is known as good cholesterol. LDL, or Low-Density Cholesterol, similarly is synonymous with bad cholesterol. HDL takes the cholesterol to the liver for disposal. On the other hand, too much LDL may cling to your arteries and block them. Clogged arteries prevent blood from reaching the heart and cause a heart attack. Hence, HDL levels should be high, and LDL should be low, if you want to avoid the risk of heart disease. To raise HDL and lower LDL, you should: Boil, grill, or bake foods instead of deep-frying. Use vegetable oils instead of butter. Consume more citrus fruits, grapes, nuts like almonds, and berries. Include whole grains, beans, lentils, and fish, like sardines and salmon, in your diet. Avoid high-calorie foods. Remove the skin from poultry before cooking. As a precaution against heart attack, you should go for periodic checkups and take the tests recommended by the doctor. One of the most important tests is the HDL test. This helps to find out the risk of developing heart disease. If you have any doubts, take the HDL test as early as possible without any delays. Even individuals with diabetes and also those in the prediabetes range should get regular check ups of the cholesterol and triglyceride levels to prevent the risk of heart diseases. Those with a family history of diabetes and hypertension should go periodically for cardiac risk profile assessment to monitor cardiac health.
Understanding Electrolyte Tests, Normal Range & Levels
Electrolytes are minerals like sodium, potassium, and chloride,, with electric charges controlling several vital functions. They enable the transport of nutrients into the cells and help remove the waste matter. An electrolytes panel or electrolyte test determines abnormal levels of electrolytes in the blood to diagnose multiple diseases and health conditions. Significance of electrolytes We know that the total water content in a healthy adult human body is about sixty per cent. Fluids in our body comprise electrolytes. These are vital for regulating the body's fluid balance and stabilising the pH level. In fact, electrolytes are helpful in maintaining heart rhythm, muscle movements, and nerve activities. Electrolytes are present in various body fluids like blood, sweat, and urine. These comprise: Sodium- Facilitates the body's fluid control and enables proper activities of muscles and nerves. Calcium- Besides building bones, calcium regulates heart rhythm, transmits nerve signals, and ensures muscle control. Phosphate- It plays a crucial role in moving compounds and molecules from cells. Magnesium- It boosts functions of the brain and muscles while helping cells to produce energy from nutrients. Chloride- It plays a vital role in the maintenance of a fluid balance between inside and outside the cell structure. Bicarbonate- It helps maintain the pH balance to prevent alkalosis and acidosis The term electrolyte has a close association with an electrical charge. An imbalance of electrolytes means your body cannot maintain balance at the basic chemical level. Electrolytes help cells conduct electricity, induce chemical reactions, and preserve the fluid balance between the inner and outer environment of cells. Electrolyte imbalance and related medical conditions Maintenance of the electrolyte balance is vital for the functioning of the body. Each electrolyte element has a specific role, and an imbalance can lead to different medical conditions requiring restoration of the electrolyte balance. Following are some conditions because of higher or lower electrolyte levels. Hyperkalemia- Excess potassium in the blood leads to arrhythmia, muscle weakness, and confusion. Hypokalemia- Low potassium levels can cause severe issues, including kidney damage. Hypercalcemia- The presence of higher levels of calcium in the blood can affect the heart, brain, and kidneys. It also causes digestive disorders and joint pain. Hypocalcemia- Low sodium levels in the blood may cause behaviour changes, confusion, muscle spasm, and loss of muscle control. Hypernatremia- Excess sodium in the blood causes behaviour issues, coma, or seizures. Hyponatremia- Insufficient sodium levels in the blood cause seizures, coma, confusion, and weak reflexes. Acidosis- Deficiency of bi-carbonate increases the acidity of the blood. This condition is known as acidosis. It may cause shortness of breath and confusion. Alkalosis- It is the opposite of acidosis. The blood becomes alkaline in alkalosis, with higher bicarbonate levels. It can cause muscle twitching and irregular heartbeats. Considering an electrolytes test There are conditions with vague symptoms like severe diarrhoea, vomiting, confusion, weakness, and irregular heartbeats. Physicians may order a serum electrolytes test if they suspect an electrolyte imbalance as the root cause. The electrolytes test involves taking out a blood sample from the individual's vein with a small needle. The test is not very painful as one may experience a minor sting-like sensation as the technician inserts the needle. No fasting is necessary before the electrolyte test unless your physician recommends additional tests like a fasting glucose test. Drink plenty of water to facilitate easy blood withdrawal. The test results will show the levels of electrolytes in mmol/L. The following are normal ranges of electrolytes: Potassium- 3.5 to 5.2 Sodium- 134 to 144 Chloride- 96 to 106 Bi-carbonate- 20 to 29 You need not panic if the results are not within the normal ranges, as several factors like medicines and dehydration can affect these values. Your physician will study the results of the electrolyte test. The main difference between positively charged and negatively charged electrolytes may suggest disorders of the kidneys or lungs. Depending on your medical history and clinical assessment, they may order additional tests if there is an electrolyte imbalance. Visit us for the electrolyte panel test! Highlights of electrolyte test The electrolyte panel test is another term for the Serum Electrolytes Test, which measures the body's electrolyte levels. A physician may order the test as part of a routine health check or to study the abnormal electrolyte levels to understand the underlying causes of irregular heart rhythm, hypertension, and kidney disorders. Measurement of Serum electrolytes may involve testing a particular electrolyte if the physician wants to check the level of a single electrolyte. Usually, the testing of common electrolytes is a routine procedure. Your physician will study the results to know the variance between normal and actual levels of different electrolytes. These levels may be normal, higher, or lower. The physician will correlate the results with other factors before reaching any conclusion. There are multiple reasons for abnormal electrolyte levels. These may not always be serious. Fluid loss because of diarrhoea or excessive sweating may cause an imbalance of electrolytes. Abnormal Serum electrolytes levels can be because of blood pressure medicines or antacids. Why does an individual need an electrolyte test? An electrolytes blood test is helpful in many situations since electrolytes play diverse roles in supporting and maintaining multiple functions. Besides ordering an electrolytes test as a routine screening test, a physician may suggest an electronic panel because: An electrolyte imbalance may involve problems in the liver and kidneys. The electrolyte panel helps monitor kidney and liver functions. It is also helpful to check the nutritional status and hydration if a physician suspects malnutrition or dehydration in a patient. An electrolyte test is helpful for checking brain health, as sodium is a significant electrolyte for a healthy brain. Calcium, potassium, and magnesium are vital electrolytes for proper heart functioning. The test is suitable for monitoring electrolyte levels in diabetes. An electrolyte blood test is suitable to assess nonspecific symptoms, such as appetite loss, dizziness, or fatigue. Physicians use the test to rule out specific endocrine, liver, and kidney conditions. The takeaway The electrolyte test helps assess body fluids. It provides a clear picture of different electrolyte levels in the blood along with the acid-base balance. A physician may order a serum electrolyte test to monitor the effectiveness of various treatments. The test helps understand the course of a specific medical condition. There are multiple causes of an electrolyte imbalance, including dehydration. An electrolyte test helps physicians arrive at a specific diagnosis or rule out a suspected disease. Electrolyte panel may also be a part of testing for other systems like Renal function tests and Comprehensive metabolic panel. Get in touch for a reliable electrolyte panel test!
Triglycerides: Everything You Need to Know
What are triglycerides? Triglycerides are essential fats you can get from foods like butter, oil, and meat. Most of our body fat are triglycerides because they are unused calories we eat but don’t need. Triglycerides in the blood help transfer adipose fat from one tissue to another and glucose in the blood from the liver. It is also a vital constituent of our skin oils. Eating excess food or food that is high in fat content that the body does not require are instantly stored in the fat cells in the form of triglycerides. The VLDL cholesterol particles in our body help transport Triglycerides to the tissues. The enzyme lipase causes the breakdown of triglycerides into fatty acids and monoglycerides. Chemical composition of triglycerides Triglyceride is chemically an ester formed by bonding three fatty acids and a glycerol molecule. We can broadly classify triglycerides into three main types - saturated, monounsaturated and polyunsaturated fatty acids. Some examples of saturated fats are Butyric acid, lauric acid, palmitic acid, myristic acid and stearic acid. We get them from meats like beef, pork, lamb, and chicken with skin; dairy products like cream, cheese, butter and eggs; and coconut, palm and their products. Saturated fats carry the potential to increase your risk of heart diseases. Therefore, we should limit their consumption in our daily diet. As per AHA (American Heart Association) recommendation, the maximum allowed dietary intake of saturated fats should not be more than 13 g per day (for a daily diet of 1200 calories). It is advisable to replace saturated fats with healthier fats, to eat lean meat and poultry without skin, and substitute your diet with more whole grains, plant proteins, and fruits and vegetables. In comparison, unsaturated fats are healthier for you. Contrary to popular belief, they are now found to help lower your risk of heart disease. Some unsaturated triglycerides are Oleic acid, Sappenic acid, Vaccenic acid, Linoleic acid, Gadoleic acid, and Gondoic acid. Unsaturated triglycerides can be found in avocados, olives, peanuts, canola oil, almonds, hazelnuts, pecans, pumpkins, and sesame seeds. How are triglycerides Different from Cholesterol? Triglycerides and cholesterol are different fats that circulate in our bodies. Triglycerides help store and use the fats, which can later be converted into energy when the body requires it. Cholesterol is essential for building cells, body tissues, and hormones like testosterone and oestrogen. What happens when you have hypertriglyceridemia? Triglyceride levels within the normal range are essential to maintain good health. But high triglyceride levels can cause heart problems like coronary artery disease, heart attacks, and arteriosclerosis (hardening of arterial walls). Very high levels of triglycerides in the body can also cause inflammation of the pancreas, known as pancreatitis. Hypertriglyceridemia is caused by a regular intake of excess calories that the body cannot utilise instantly. This can happen due to Excess sugar intake Obesity Smoking Excess alcohol consumption Consuming certain types of medications like beta blockers, diuretics, steroids, retinoids etc. Genetic disorders Thyroid problems Uncontrolled type 2 diabetes., Liver diseases Kidney diseases Checking your triglycerides level A couple of blood tests known as the lipid profile are prescribed to measure your triglycerides and cholesterol levels that can help you keep tabs on your fat levels. The value of triglyceride level also works as an aid for your physician to help you have a controlled diet in case of a risk of heart disease. Triglycerides are measured as milligrams per decilitre of blood. It is a simple blood test which may require you to fast for 12 hours to get an accurate reading. Interpretation Triglycerides level Normal less than 150mg/dL Borderline high 150-199mg/dL High 200-499mg/dL Very high 500+ mg/dL (Readings are for a normal adult blood sample) It is either done as an individual test or in conjunction with other cholesterol and lipid tests as part of Lipid profile tests. What do the values suggest? Any value over 150mg/dL of triglycerides in the blood can be interpreted as follows: It can increase your risk of heart disease like a stroke. You will also need to test for metabolic disorders (high blood pressure and uncontrolled diabetes and obesity combined). It is an indicator of borderline or type II diabetes. Hypothyroidism Genetic disorders may cause poor conversion of fat into energy. In most cases other cholesterol tests like HDL, LDL , Lipid profile, cardiac profile etc are also done along with triglyceride tests to infer better results. Available treatments for increased triglycerides You should talk to your primary health care physician to make lifestyle changes if triglycerides are above the prescribed range. The following lifestyle changes could be recommended: Weight control Regular physical exercises and activities (for at least 30 mins) Stop smoking Prohibit the use of Alcohol Limit sugar Limit refined and processed foods Using healthy fats instead of saturated fats Intermittent fasting Modified diet to suit your needs and health If lifestyle changes are not enough, your physician may prescribe medications like fish oil, niacin or statins, which may help reduce cholesterol and triglyceride levels. How can you change your diet if you have high triglycerides? If you find that you have hypertriglyceridemia, then there are several options to make your diet more health friendly - Limit the use of starchy vegetables like corn and peas. Canned beans should be replaced with black beans, and you should avoid cooking them with pork or sugar. Too much natural sugar should also be avoided. For example, 2 to 3 servings of fruits should be the limit for a single day. Dried foods for consumption should be measured using a teaspoon. Buy canned fish preserved in water rather than in oil. Coconut is a common ingredient in most of our foods. If you have high triglycerides levels, it is better to talk to a doctor about how much coconut you should consume in your daily diet. Monitor your pasta, white bread, cereals, potatoes, and oatmeal servings. Sugary drinks like soda, fruit juices, iced tea, and sweet coffee should be limited. Bakery items made in butter can be skipped or taken as a tiny serving. Processed meats like bacon, sausage, and hams should be limited or avoided. You can replace butter with canola, olive, walnut or flaxseed oils for cooking and salad dressings. Conclusion Triglyceride levels could be high in your blood without any obvious symptoms or visible signs. High levels of triglycerides are a problem because it causes long-term damage and increases the chances of grave diseases or proves to be fatal. Hence, it is important to keep a regular check on your triglyceride levels and get routine screening done with the Lipid Profile Test. This test covers not just triglycerides but also other cholesterol levels that can cause damage to your body and heart. The frequency of the test is dependent on age and current medical conditions as recommended by your treating physician. At times, certain other blood tests to assess the levels of cardiac markers are also suggested. High triglycerides if left untreated may also contribute towards high blood glucose levels. Hence, it is also recommended to keep a check on the blood glucose levels with regular testing and HbA1c monitoring.
 Home Visit
Home Visit Upload
Upload


















 WhatsApp
WhatsApp